Hepatic artery reinforcement after post pancreatectomy haemorrhage caused by pancreatitis
Introduction
Post-pancreatectomy hemorrhage (PPH) is a major complication occurring in 6–8% of patients after pancreaticoduodenectomy (PD) (1,2). Arterial bleeding is the most frequent cause. Mortality rate could reach 30% after grade C PPH according to ISGPS classification (1-3). Traditionally, a reoperation was performed but the emergence of interventional endovascular procedure has changed the PPH management. Complete interruption of hepatic arterial flow has to be a salvage procedure because of the high risk of intrahepatic abscess following the procedure. Surgical reoperation is still recommended in case of early postoperative bleeding or hemodynamic instability. Herein we report a technique to perform an artery reinforcement after PPH caused by pancreatitis.
Case presentation
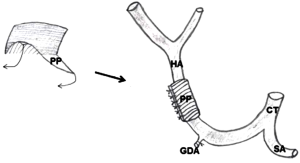
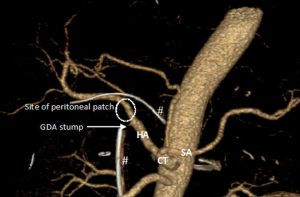
Ampullary carcinoma was diagnosed in a 68-year-old man presenting angiocholitis. PD according to Whipple’s procedure with child’s reconstruction was performed. At postoperative day 5, the patient presented fever. Abdominal drainage evacuated pancreatic leak. Computed tomography (CT) showed no intra-abdominal collection. Pancreatic leak was well tolerated and invasive treatment was unnecessary. At postoperative day 12, the patient presented a sudden violent abdominal pain with arterial hypotension and tachycardia. Blood analysis showed an anemia at 8 g/dL. CT with intravenous contrast injection was performed. Arterial and venous phases showed a contrast extravasation on the hepatic artery (Figure 1). We initially decided to treat the patient with an interventional radiologic procedure. However, hemodynamic parameters of the patient rapidly decreased. Urgent laparotomy was performed. Origin of PPH was found as an erosion of hepatic artery caused by pancreatic leak. Gastroduodenal artery (GDA) stump was intact. Bleeding was stopped with a 5.0 suture without interrupting arterial flow. Arterial reconstruction with graft was not possible to substitute damaged hepatic artery in the septic context. A peritoneal patch was placed around hepatic artery to reinforce damaged arterial wall. The peritoneal patch was harvested from right hypochondrium with a thin preperitoneal fat layer. The patch was sutured around hepatic artery with musculoaponeurotic face placed on the arterial wall (Figure 2). Pancreatic necrosis was removed. Pancreaticojejunal anastomosis was redone because the pancreatic duct external drainage was still in the pancreatic main duct. Abdominal drainage was placed in contact of pancreatic anastomosis and arterial suture.
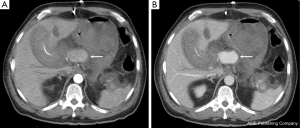
No recurrent bleeding occurred during postoperative course. A new CT was performed to search residual collection in context of fever at day 20. There was no collection, no hematoma nor active bleeding. Hepatic artery was permeable with normal caliber in the portion of peritoneal patch reinforcement (Figure 3). Fever disappeared with systemic antibiotherapy. All drains were removed except intraductal pancreatic drain left for up to 6 postoperative weeks. The patient recovered normal oral feeding. He was discharged at day 30. One-year follow-up showed no sign of tumoral recurrence.
Discussion
PPH is a severe complication, two possible managements exist: radiological or surgical approach. Endovascular procedure consists in catheterizing the artery responsible for the hemorrhage. Hemostasis is obtained by placement of a covered stent (i.e., for hepatic artery) or coils interrupting arterial flow (i.e., gastroduodenal residual artery). Endovascular management has a success rate of 80% after one procedure and could be repeated for recurrent hemorrhage (4). Surgical management consists in re-laparotomy. Hemostasis could be obtained promptly by clamping and suturing when a normal artery is in cause. However, in case of delayed PPH after PD, bleeding occurs frequently in septic context on an artery eroded by pancreatic leak (5). This situation increases the risk of recurrent hemorrhage. Several authors has described preventive techniques to isolate hepatic artery of the pancreatic anastomosis and reduce PPH risk such as placement of a falciform ligament or omental flap (6,7). The technique described in the present case consists in reinforcing directly arterial wall after occurrence of PPH. The use of a peritoneal patch during pancreatic surgery has first been described to replace a portion of portal vein after venous resection with the peritoneal layer placed on the intraluminal side of the vein (8). The results of this technique were only evaluated in small series. No necrosis of the patch was described. In the present report, placement of the musculoaponeurotic layer on the arterial wall could permit a revascularization of the peritoneal patch and integration to the arterial wall.
The present case describes a salvage technique to reinforce damaged artery after PPH in context of pancreatic leak. This simple technique could be useful to avoid complex arterial reconstruction and recurrent bleeding in septic context.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Grützmann R, Rückert F, Hippe-Davies N, et al. Evaluation of the International Study Group of Pancreatic Surgery definition of post-pancreatectomy hemorrhage in a high-volume center. Surgery 2012;151:612-20. [Crossref] [PubMed]
- Wellner UF, Kulemann B, Lapshyn H, et al. Postpancreatectomy hemorrhage--incidence, treatment, and risk factors in over 1,000 pancreatic resections J Gastrointest Surg 2014;18:464-75. [Crossref] [PubMed]
- Wente MN, Veit JA, Bassi C, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 2007;142:20-5. [Crossref] [PubMed]
- Asai K, Zaydfudim V, Truty M, et al. Management of a delayed post-pancreatoduodenectomy haemorrhage using endovascular techniques. HPB (Oxford) 2015;17:902-8. [Crossref] [PubMed]
- Yekebas EF, Wolfram L, Cataldegirmen G, et al. Postpancreatectomy hemorrhage: diagnosis and treatment: an analysis in 1669 consecutive pancreatic resections. Ann Surg 2007;246:269-80. [Crossref] [PubMed]
- Ray S, Sanyal S, Ghatak S, et al. Falciform ligament flap for the protection of the gastroduodenal artery stump after pancreaticoduodenectomy: A single center experience. J Visc Surg 2016;153:9-13. [Crossref] [PubMed]
- Maeda A, Ebata T, Kanemoto H, et al. Omental flap in pancreaticoduodenectomy for protection of splanchnic vessels. World J Surg 2005;29:1122-6. [Crossref] [PubMed]
- Dokmak S, Aussilhou B, Sauvanet A, et al. Parietal Peritoneum as an Autologous Substitute for Venous Reconstruction in Hepatopancreatobiliary Surgery. Ann Surg 2015;262:366-71. [Crossref] [PubMed]


