
Effects of enhanced recovery after surgery on robotic radical prostatectomy: a systematic review and meta-analysis
Introduction
Prostate cancer is the most commonly occurring tumor in the male genitourinary system, with a high incidence rate worldwide (1). With the development of minimally invasive surgery, robotic radical prostatectomy (RRP) has been widely used in the treatment of prostate cancer, which has had great clinical significance in terms of reducing surgical trauma and promoting postoperative recovery (2-4). The nursing methods after robot radical prostatectomy include routine nursing, intraoperative posture management, robotic nursing and enhanced recovery nursing (3).
Enhanced recovery after surgery (ERAS), also known as fast track surgery (FTS) or early recovery, was first conceived and practiced by Kehlet in 1997. It involves a series of measures in the perioperative period that are intended to reduce or decrease physiological and psychological stress, and to promote the early recovery of patients (5-7). It was first applied in gastrointestinal surgery where it achieved positive results, and since then it had been extended to hepatobiliary surgery, orthopedics and urology (8-10).
Studies have shown that ERAS can significantly shorten the hospital length of stay (LOS) and reduce the costs associated with hospitalization without increasing the incidence of surgical complications (11-13). To date, however, its application in radical prostatectomy, especially robot-assisted radical prostatectomy, has been relatively limited (14,15). Although some studies have explored the safety and efficacy of ERAS for RRP, the results are inconsistent (16,17).
At present, there is a lack of systematic review in the literature on whether ERAS is better than conventional protocols. In order to further evaluate the effectiveness and safety of ERAS, we perform this meta-analysis to compare the clinical effects of different recovery pathways, namely ERAS and conventional, for RRP. We present the following article in accordance with the PRISMA reporting checklist (available at https://dx.doi.org/10.21037/gs-21-699).
Methods
Literature search strategy
A systematic search of academic publication databases (PubMed, EMBASE, Web of Science and China National Knowledge) for relevant studies published between January 2000 and February 2021 was conducted. The following keywords (combined with the Boolean operator “and”) were used in the search: enhanced recovery after surgery (ERAS); fast track surgery (FTS); robotic radical prostatectomy (RRP). The literature search was comprehensive, with no limitations on the publishing language. To maximize search sensitivity and identify as many relevant studies as possible, a manual screen of the reference lists of all identified papers was also performed to identify any additional studies of relevance.
Study selection
To be included in this review, studies were required to meet the following inclusion criteria:
- Research must contain indicators for assessing and comparing the effectiveness of ERAS and conventional protocols in terms of patient outcomes;
- Patients must have undergone RRP;
- Full text articles must be available.
Data extraction and quality assessment
Using standardized screening forms, teams of two reviewers independently screened all titles and abstracts that were identified in the literature search. The reviewers obtained full-text articles of all potentially eligible studies, and then evaluated them for eligibility. In performing the evaluation, the following details were recorded: first author’s name, type of study, patient’s age and gender, country of origin, year of publication, sample size, study duration, and primary outcome. The methodological quality was assessed with the Cochrane bias risk assessment tool.
Statistical analysis
The impact of the results in the selected reports was estimated using the risk of bias tool in Review Manager (version 5.3, Cochrane Collaboration, 2014). Mean difference (MD) and 95% confidence interval (CI) were calculated for continuous results. Heterogeneity across the studies was tested using I2 statistics, which provide a quantitative degree of inconsistency. In this meta-analysis, I2 of 25%, 50% and 75% were deemed to represent low, medium and high heterogeneity, respectively. Where I2>50%, potential sources of heterogeneity were identified by sensitivity analyses. These were conducted by removing one study at a time and evaluating its influence on the overall pooled estimate. Where heterogeneity was observed, a random effect model was used. In addition, potential publication bias was assessed using a funnel plot, and sensitivity analysis was performed to examine the robustness of results.
Results
Search process
Through electronic searching, a total of 554 studies of potential interest were identified. After careful reading, 79 studies meeting the inclusion criteria were identified. Of these, a further 71 articles were excluded due to study design differences or insufficient available data. Ultimately, 8 papers were included in this meta-analysis (18-25). Further details relating to the search process and inclusion and exclusion criteria are presented in Figure 1.
Characteristics of included studies
A standard data extraction form was created to collect data from the included studies, including: first author, year of publication, country, age, gender, sample size, recruitment time and primary outcome (Table 1). These studies contained 2 randomized controlled trials (RCTs), 2 prospective cohort studies, and 4 retrospective cohort studies. A total of 967 patients were available for the meta-analysis, which included 462 patients subject to ERAS and 505 patients subject to the conventional protocol. All 8 articles were published from 2013 to 2019, and the sample sizes ranged from 29 to 313.
Table 1
| Study | Country | Type of study | No. patients | Age, years | Years of onset | Primary outcome* | |||
|---|---|---|---|---|---|---|---|---|---|
| ERAS | Control | ERAS | Control | ||||||
| Ploussard, 2020 | France | Prospective cohort study | 156 | 157 | 65.9 | 66.3 | From 2014 to 2019 | 4 | |
| Huang, 2018 | China | Retrospective cohort study | 36 | 37 | 62.1±6.9 | 63.5±7.4 | October 2015 to November 2017 | 1,3,4 | |
| Sugi, 2017 | Japan | Retrospective cohort study | 75 | 123 | 68 [49–75] | 69 [45–76] | August 2013 and June 2015 | 3,4 | |
| Pan, 2018 | China | RCT | 50 | 50 | 68.75±7.24 | 69.56±7.67 | October 2016 to May 2017 | 1,2,4 | |
| Yaiesh, 2016 | Kuwait | Prospective cohort study | 17 | 12 | – | – | February 2014 and May 2016 | 4 | |
| Li, 2020 | China | Retrospective cohort study | 22 | 20 | 67.05±8.04 | 68.90±8.06 | July 2017 to April 2019 | 1,2,4 | |
| Graham, 2019 | United States | Retrospective cohort study | 63 | 63 | – | – | – | 2,4 | |
| Li, 2021 | China | RCT | 43 | 43 | 65.47±7.26 | 64.54±7.38 | March 2016 to January 2019 | 1,2,3,4 | |
*, 1: time of first flatus; 2: time of catheter removal; 3: complication; 4: hospital LOS. ERAS, enhanced recovery after surgery; RCT, randomized controlled trial; LOS, length of stay.
Results of quality assessment
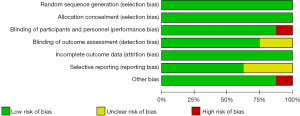
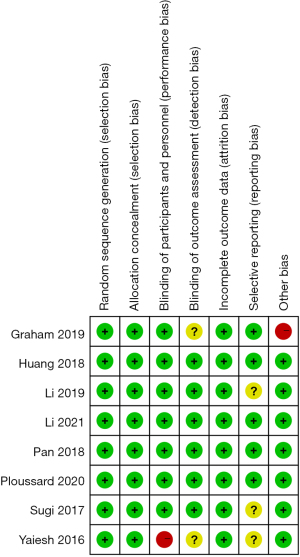
The overall methodological quality was evaluated using the Cochrane bias risk assessment tool. High risk of performance bias and other bias was found in two different studies (Figure 2). A summary of all of the kinds of bias found in each study is presented in Figure 3.
Results of heterogeneity test
Four of the included studies reported time of first flatus. The forest plot (Figure 4) shows that the ERAS group had significantly reduced time of first flatus as compared to the conventional group (MD =−0.58; 95% CI: −0.88, −0.29; P=0.0001; random effect model). The pooled studies were homogeneous (P=0.07; I2=57%).
Four of the included studies, involving a total of 354 patients, reported time of catheter removal. Meta-analysis showed that compared to the conventional group, the ERAS group exhibited significantly shortened time of catheter removal (MD =−1.65; 95% CI: −2.15, −1.16; P<0.00001; random effect model), and there was significant heterogeneity (P=0.010; I2=74%) (Figure 5). Sensitivity analysis was performed by removing Li 2020’s study (20), and the result was not changed (P=0.05; I2=68%).
Three of the included studies reported postoperative complications. A random effect model was used to evaluate the heterogeneity of postoperative complications. The results showed that there was no significant difference between the ERAS group and the conventional group in evaluation of postoperative complications [risk ratio (RR) =0.49; 95% CI: 0.23, 1.05; P=0.07], with no significant heterogeneity (P=0.06; I2=64%) (Figure 6).
In evaluating hospital LOS between ERAS groups and conventional groups, 8 articles involving 967 patients were included. LOS was analyzed by random effect model. The MD of LOS was −1.49 with 95% CI: −2.65, −0.34 (P=0.01), which indicated that the LOS of the ERAS group was significantly lower than that in conventional group (Figure 7). The pooled studies were heterogeneous (P<0.00001; I2=96%). A sensitivity analysis was performed by removing Sugi’s study (23), however the result remained unchanged (P<0.00001; I2=94%).
Publication bias
To identify any evidence of publication bias amongst the included studies, a funnel plot for the time of first flatus was produced. The shape of the resulting funnel plot is symmetrical (Figure 8), indicating that no publication bias exists in this meta-analysis.
Discussion
Radical prostatectomy has proven an excellent stage from which to showcase the value of the Da Vinci robot. Because the prostate is located in the depths of the male pelvic cavity, traditional open surgery is characterized by a large incision, significant trauma, increased bleeding, increased postoperative complications, and obvious pain and slow recovery which can easily cause psychological and physiological stress (2,3,26). RRP has become the first choice for the treatment of prostate cancer in recent years (27). Its advantages are minimal trauma, reduced bleeding, rapid recovery, and effective reduction of postoperative complications such as urinary incontinence and positive margins (4,26).
ERAS has been shown to be an effective, reliable and practical clinical nursing method, for example, ERAS has shown great effect in patients with gastrointestinal malignancies, obstetric and thoracic surgery (28-30). Some studies have shown that the implementation of ERAS nursing during the perioperative period for patients undergoing RRP can effectively maintain the stability of the patients’ internal environment, reduce the stress response caused by surgical trauma, and decrease the clinical complications (31-33).
ERAS involves cooperation between the surgical department, the anesthesia department and the nursing team. As such it is dependent on multi-disciplinary collaborative development, and represents a high standard of medical care (34,35). Laparoscopic surgery combined with ERAS has become an important direction for the development of surgical operation (36,37). It was used in the perioperative surgery of gastrointestinal and abdominal tumors (38,39). Research into the applications of ERAS to urology have primarily focused on radical resection of bladder cancers, which can involve intestinal surgery. Research into applications of ERAS in RRP was limited, but still showed positive significance (17,40).
In this study, a meta-analysis was performed to explore the safety and effectiveness of ERAS in perioperative nursing of patients undergoing RRP. The results showed that ERAS could significantly reduce time of first flatus, time of catheter removal and LOS. Gralla’s study (41) reported that FTS could significantly reduce the incidence of complications (P=0.02), but in the meta-analysis presented here no significant difference in postoperative complications was observed. This may be due to the limited research data available for analysis, and additional studies should be carried out to support further investigations into the potential significance of such effects.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://dx.doi.org/10.21037/gs-21-699
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/gs-21-699). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Binder J, Kramer W. Robotically-assisted laparoscopic radical prostatectomy. BJU Int 2001;87:408-10. [Crossref] [PubMed]
- Allan C, Ilic D. Laparoscopic versus robotic-assisted radical prostatectomy for the treatment of localised prostate cancer: a systematic review. Urol Int 2016;96:373-8. [Crossref] [PubMed]
- Gandaglia G, Briganti A, Clarke N, et al. Adjuvant and salvage radiotherapy after radical prostatectomy in prostate cancer patients. Eur Urol 2017;72:689-709. [Crossref] [PubMed]
- Kehlet H. Enhanced recovery after surgery (ERAS): good for now, but what about the future? Can J Anaesth 2015;62:99-104. [Crossref] [PubMed]
- Jiang W, Mao Q, Xie Y, et al. Enhanced recovery after surgery (ERAS) program in elderly patients undergoing laparoscopic hepatectomy: a retrospective cohort study. Transl Cancer Res 2020;9:4563-4572. [Crossref]
- Li H, Liu Y, Li Q, et al. Effects of a fast track surgery nursing program in perioperative care of older patients with a hip fracture. Eur Geriatr Med 2020;11:519-25. [Crossref] [PubMed]
- Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg 2017;152:292-8. [Crossref] [PubMed]
- Melloul E, Hübner M, Scott M, et al. Guidelines for perioperative care for liver surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg 2016;40:2425-40. [Crossref] [PubMed]
- Pearsall EA, Meghji Z, Pitzul KB, et al. A qualitative study to understand the barriers and enablers in implementing an enhanced recovery after surgery program. Ann Surg 2015;261:92-6. [Crossref] [PubMed]
- Gotlib Conn L, McKenzie M, Pearsall EA, et al. Successful implementation of an enhanced recovery after surgery programme for elective colorectal surgery: a process evaluation of champions' experiences. Implement Sci 2015;10:99. [Crossref] [PubMed]
- Scott MJ, Baldini G, Fearon KC, et al. Enhanced recovery after surgery (ERAS) for gastrointestinal surgery, part 1: pathophysiological considerations. Acta Anaesthesiol Scand 2015;59:1212-31. [Crossref] [PubMed]
- Wang Y, Li J, Weng Y, et al. A new enhanced recovery after surgery pathway for left-sided pancreatic cancer patients after distal pancreatectomy. Transl Cancer Res 2019;8:2613-20. [Crossref]
- Hu JP, Pan JR, Cheng N, et al. Comparison between enhanced recovery after surgery (ERAS) strategy and conventional strategy in laparoscopic radical prostatectomy. Chinese Journal of Endourology 2019;13:158-61. (Electronic Version).
- Zhang ZY, Wang K, Lin CH, et al. The application of enhanced recovery after surgery in laparoscopic radical prostatectomy. Chinese Journal of the Frontiers of Medical Science 2017;9:7-11. (Electronic Version).
- Ploussard G, Almeras C, Beauval JB, et al. Same-day discharge surgery for robot-assisted radical prostatectomy in the era of ERAS and prehabilitation pathways: a contemporary, comparative, feasibility study. World J Urol 2020; Epub ahead of print. [Crossref] [PubMed]
- Zhang X, Jin R, Zheng Y, et al. Interactions between the enhanced recovery after surgery pathway and risk factors for lung infections after pulmonary malignancy operation. Transl Lung Cancer Res 2020;9:1831-42. [Crossref] [PubMed]
- Graham J, Dickerson S, Longhitano Y, et al. Immediate impact of a multidisciplinary enhanced recovery after surgery program for robotic radical prostatectomies. Clinical Nutrition ESPEN 2019;31:116-7. [Crossref]
- Huang Z, Yi L, Zhong Z, et al. Comparison of fast-track versus conventional surgery protocol for patients undergoing robot-assisted laparoscopic radical prostatectomy: a Chinese experience. Sci Rep 2018;8:8017. [Crossref] [PubMed]
- Li J, Yu YE, Xu L. Application of rapid rehabilitation nursing in perioperative period of Da Vinci robot radical prostatectomy. Today Nurse 2020;27:49-51.
- Pan J, Li P. Application effect of fast track surgery combined with collaborative nursing mode in patients undergoing robot assisted laparoscopic radical prostatectomy. Today Nurse 2018;25:58-61.
- Ploussard G, Almeras C, Beauval JB, et al. A combination of enhanced recovery after surgery and prehabilitation pathways improves perioperative outcomes and costs for robotic radical prostatectomy. Cancer 2020;126:4148-55. [Crossref] [PubMed]
- Sugi M, Matsuda T, Yoshida T, et al. Introduction of an enhanced recovery after surgery protocol for robot-assisted laparoscopic radical prostatectomy. Urol Int 2017;99:194-200. [Crossref] [PubMed]
- Yaiesh S, Aldousari S, Abul F, et al. Does a standardized algorithm for managing patients post-robotic-assisted radical prostatectomy improve recovery? Experience with the Optimized Surgical Journey. European Urology Supplements 2016;10:e1288-9. [Crossref]
- Li YF, Zhang J, Zhang P, et al. The application effects of perioperative rapid rehabilitation nursing combined with clinical pathway in patients with prostate cancer undergoing radical prostatectomy. Hebei Medical Journal 2021;43:310-3.
- Herrell SD, Smith JA Jr. Laparoscopic and robotic radical prostatectomy: what are the real advantages? BJU Int 2005;95:3-4. [Crossref] [PubMed]
- Tang K, Jiang K, Chen H, et al. Robotic vs. Retropubic radical prostatectomy in prostate cancer: A systematic review and an meta-analysis update. Oncotarget 2017;8:32237-57. [Crossref] [PubMed]
- Cao S, Zheng T, Wang H, et al. Enhanced recovery after surgery in elderly gastric cancer patients undergoing laparoscopic total gastrectomy. J Surg Res 2021;257:579-86. [Crossref] [PubMed]
- Carli F. Physiologic considerations of enhanced recovery after surgery (ERAS) programs: implications of the stress response. Can J Anaesth 2015;62:110-9. [Crossref] [PubMed]
- Zhao Y, Zhang S, Liu B, et al. Clinical efficacy of enhanced recovery after surgery (ERAS) program in patients undergoing radical prostatectomy: a systematic review and meta-analysis. World J Surg Oncol 2020;18:131. [Crossref] [PubMed]
- Qiang H, Yuanshui S. Effect of early enteral nutrition on laparoscopic common bile duct exploration with enhanced recovery after surgery protocols. Eur J Clin Nutr 2020;74:666. [Crossref] [PubMed]
- Kim KM, Kwak JG, Shin BC, et al. Early experiences with ultra-fast-track extubation after surgery for congenital heart disease at a single center. Korean J Thorac Cardiovasc Surg 2018;51:247-53. [Crossref] [PubMed]
- Hanna P, Zabell J, Osman Y, et al. Enhanced recovery after surgery (ERAS) following radical cystectomy: is it worth implementing for all patients? World J Urol 2021;39:1927-33. [Crossref] [PubMed]
- Currie A, Soop M, Demartines N, et al. Enhanced recovery after surgery interactive audit system: 10 years' experience with an international web-based clinical and research perioperative care database. Clin Colon Rectal Surg 2019;32:75-81. Erratum in: Clin Colon Rectal Surg 2019;32:e1. [Crossref] [PubMed]
- Lohsiriwat V, Jitmungngan R, Chadbunchachai W, et al. Enhanced recovery after surgery in emergency resection for obstructive colorectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis 2020;35:1453-61. [Crossref] [PubMed]
- Murin P, Weixler VHM, Romanchenko O, et al. Fast-track extubation after cardiac surgery in infants: Tug-of-war between performance and reimbursement? J Thorac Cardiovasc Surg 2021;162:435-43. [Crossref] [PubMed]
- Wilches C, Sulbarán JD, Fernández JE, et al. Fast-track recovery technique applied to primary total hip and knee replacement surgery. Analysis of costs and complications. Rev Esp Cir Ortop Traumatol 2017;61:111-6. [Crossref] [PubMed]
- Zhang H, Wang H, Zhu M, et al. Implementation of enhanced recovery after surgery in patients undergoing radical cystectomy: A retrospective cohort study. Eur J Surg Oncol 2020;46:202-8. [Crossref] [PubMed]
- Ding J, Sun B, Song P, et al. The application of enhanced recovery after surgery (ERAS)/fast-track surgery in gastrectomy for gastric cancer: a systematic review and meta-analysis. Oncotarget 2017;8:75699-711. [Crossref] [PubMed]
- Valicenti RK, Gomella LG, Ismail M, et al. Pathologic seminal vesicle invasion after radical prostatectomy for patients with prostate carcinoma: effect of early adjuvant radiation therapy on biochemical control. Cancer 1998;82:1909-14. [Crossref] [PubMed]
- Gralla O, Haas F, Knoll N, et al. Fast-track surgery in laparoscopic radical prostatectomy: basic principles. World J Urol 2007;25:185-91. [Crossref] [PubMed]
(English Language Editor: E. Davies)








