Endoscopic thyroidectomy: the transoral approach
Introduction
Endoscopic or minimally invasive surgery (MIS) is becoming more and more popular. Since the first endoscopic cholecystectomy was performed in the early 1980s, endoscopic procedures have become standard in nearly all fields of surgery. In view of the extremely fast technical progress, the evolution of these innovative procedures seems to be unstoppable. Terms like “Natural Orifice Transluminal Endoscopic Surgery (NOTES)”, “scarless operations” or “micro invasive surgery” have readily been adopted and spread by the medical industry to serve as marketing instruments.
In thyroid surgery this effects started later. It is a lot more difficult to find an endoscopic approach to the thyroid simply because of where it is placed in the human body. All the space needed for visibility and for operating has to be created, because there is no natural cavity, and it is quite complicated to create this space.
So far, ways of accessing the thyroid other than via direct open surgery in the neck region proved to be endoscopic at best, but certainly not minimally-invasive. It seemed natural to look for ways that would both create a minimum of visible scars and provide for a short and safe access to the thyroid, such as the transoral approach. Still, such efforts need closer scrutiny before we can declare transoral thyroid surgery a safe and recommendable approach for patients in general.
The rationale of safe and atraumatic thyroid surgery
The era of thyroid surgery in Europe started in the late 19th century by pioneers like Kocher and Billroth. At that time, patients’ survival was the main target to achieve. After developing instruments like the ultrasound dissectors (1), ligation clips and the intraoperative nerve monitoring system (2) patients’ safety became the main aim in thyroid surgery. Today, all these aspects should be a matter of course in a specialized department. Usually, the advantages of minimally invasive procedures are seen in less pain, less bleeding, a faster recovery and better cosmetic results achieved by smaller almost invisible scars. As the first of these demands—the improvement of postoperative pain levels could not be scientifically proved yet—the cosmetic results can be pointed out as the main advantage in these minimally invasive or endoscopic thyroidectomy procedures. By now, we know that the demands on cosmetic surgery is high and increasing, because these results are obvious. On the other hand, cosmetic results have never been so important, when the standards and guidelines in endocrine surgery were developed.
So we must ensure, that all endoscopic and minimally invasive operations do not step back with regard to the procedures’ quality. For example a minimally invasive resection of a single nodule should not be performed if a hemi-thyroidectomy is the adequate operation in open surgery.
The following prerequisites should be considered:
- the advantages of MIS must be ensured (trauma of access, cosmetic aspects);
- safety and size of resected specimen must be equal to open procedures (quality);
- the thyroid tissue must be removed without touching other organs/structures (oncological aspect).
If we can provide the same quality level in open and endoscopic thyroid surgery we must still admit, that the most significant difference is the cosmetic result. The authors own experience is that the importance of an invisible scar at the neck is under cultural aspects of great importance in Southeast Asia (3).
Main aim is to achieve an optimal cosmetic result while keeping the access trauma acceptably low. Another important factor for successful endoscopic thyroid surgery is the short distance for the approach—the access trauma: the closest the access to the thyroid gland the better the approach. For example, the axillo-bilateral-breast-approach (ABBA)-technique cannot be considered as a minimally-invasive method.
In order to achieve the aim of an optimal thyroidectomy we need a short, minimally-invasive access to the thyroid gland which allows optimal cosmetic results: the transoral access.
Reported techniques for transoral thyroid surgery
In literature the resection of ectopic lingual thyroid tissue is the most obvious indication for the transoral approach in patients (4,5). They were already reported in the last century, but actually improved by using robotic surgery (4). These experiences showed that it is possible to remove ectopic thyroid tissues via the transoral access in living humans. We were the first to report on our experiences with the transoral endoscopic resection of the thyroid gland in human cadavers and living pigs (6). This paper encouraged other authors to introduce modified transoral approaches to the thyroid along with the advent of NOTES in pigs or human cadavers (7-9).
Our technique used an additional 3-mm collar access to allow triangulation in transoral surgery. Triangulation means the possibility to prepare bimanually as one can do it for example in classic laparoscopic cholecystectomy in comparison to the single port access. In surgery, with non-flexible, rigid instruments the triangulation is mandatory for a successful endoscopic surgery (10).
We agree that, in using this access, adequate antibiotic prophylaxis is necessary for avoiding infections, as demonstrated by the experience with transoral access to the hypophysis in neurosurgery (6,11).
Our own studies showed that a complete thyroid resection could be achieved on human cadavers via the transoral approach without major difficulties. In ten living pigs we were able to dissect using the obturator without any bleeding. The average operation-access time from the introduction of the axilloscope to the removal of the obturator from the axilloscope just above the larynx was at about 1 minute (Figure 1).
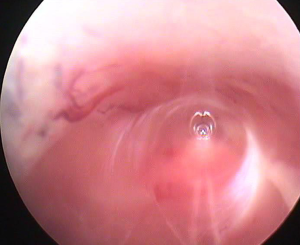
We did not notice any complications or bleedings during this part of the operation, nor did the creation of a 3.5-mm access in the front neck region under visual control cause complications in any of the pigs.
During lateral dissection we identified the inferior thyroid artery in 18 of the 20 lobes that were operated on, so that we could use them as a routing structure for finding the recurrent laryngeal nerve (RLN). We then identified this nerve and the vagus nerve using the bipolar neuro-monitoring probe, which had been introduced through the 3.5-mm trocar (12). After cutting the inferior thyroid artery with the ultrasonic scalpel we completely dissected the entire lobe and removed it as a whole transorally through the tube of the axilloscope.
We then again identified the RLNs and the vagus nerves on both sides. After resection, all 20 RLNs were found and identified, which proved that in no case any of the nerves had been injured: no lesion whatsoever could be found. We removed the instrument tube and did a sublingual suture of the mucosa. Since no bleeding occurred during the entire operation neither swab nor ejector were employed.
The average operation time was 50 minutes (range, 27–103 minutes). The specimen weighed 5.2 grams on average. The pigs were observed for another 2 hours after operation, but did not show any signs of haemodynamic instability or secondary haemorrhage. The documented bleeding 2 hours after the procedure was 0 to 4.5 mL (average, 2.2 mL), not depending on operation time or weight of resected tissue. We did a post-mortem examination of the operation area and documented the operation results.
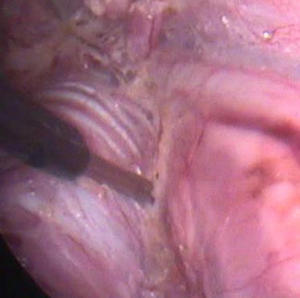
This access was used by Karakas et al. too in his animal-study in 2010 (8). They described the so-called transoral partial parathyroidectomy (TOPP)-technique as a new transoral method. The access via the sublingual access was performed more dorsally, directly in front of the trachea. It is setting up a space at the dorsal side of the thyroid gland. After feasibility studies in ten living pigs they performed parathyroidectomies in two patients, with one patient undergoing a transient palsy of the hypoglossal nerve. He reported on the patient’s low acceptance of the transoral procedure and concluded that the adequate resection is not possible with the actually available instruments (13). In 2014 they reported on five patients who agreed for the TOPP method. In three of them the endoscopic procedure could be completed, in these three patients, a parathyroid adenoma could be removed via the transoral access. In two patients, the procedure had to be converted to the conventional open technique. One patient had a transient RLN palsy, while one patient suffered from a transient palsy of the right hypoglossal nerve. Three patients developed a hematoma of the mouth floor and swallowing problems. Karakas et al. concluded that although feasible, TOPP is still poorly accepted by patients and its complication rate is high. “Thus, TOPP is nonsense with currently available devices (14)” (Figure 2).

Anatomical studies (15) showed that the dorsal TOPP-access is more dangerous for the hypoglossal nerve. The anterior way as Witzel described it in combination with an additional vestibular access (6) seems to be safer. The anterior region of the neck can be reached through the midline of the mouth floor and the suprahyoid muscles. No important nerves and vessels were found in the approach of the so-called EMIT-technique. TOPP set up the space at the dorsal side of the thyroid gland and adjacent to the trachea. The hypoglossal nerve and the lingual nerve as well as their accompanying blood vessels were anatomically related to the approach and could be injured during the procedure. The surgical space is much limited in TOPP (<20 mm in diameter) and current surgical instruments still did not match the requirement of this technique.
Robotic transoral thyroidectomy on two cadavers was described as the so-called robotic transoral periosteal thyroidectomy (TOPOT)-technique (16). They developed TOPOT technique with four ports by using the da Vinci system. This approach provides in their opinion a safe superior access to the thyroid and central neck compartment. Total thyroidectomy and central neck dissection were performed on two human cadavers using the da Vinci robot with the transoral periosteal approach. Complete thyroidectomy and central neck dissection were possible in human cadavers without injury to the RLN (16). They concluded that transoral thyroidectomy using four ports is a feasible method that could be used in living humans.
A tri-vestibular transoral approach in fresh frozen cadavers was described by Park et al. in 2014 (9) “to introduce NOTES to the head and neck area of medicine”. The transoral tri-vestibular approach seems to provide a good view and surgical field for endoscopic thyroidectomy. However, the transoral approach for thyroidectomy remains experimental, and the detailed surgical technique should be refined via further clinical studies, they concluded.
A Trans-Oral Video-Assisted Neck Surgery (TOVANS) called gasless technique (17) has been described and performed on eight patients. Incision was made at the vestibule under the inferior lip. From the vestibule to the anterior cervical region, a subplatysmal tunnel in front of the mandible was created and cervical skin was lifted by Kirschner wires and a mechanical retracting system. This method without CO2 insufflation created an effective working space and provided an excellent cranio-caudal view so that thyroidectomy and central node dissection could be performed safely. Three of the eight patients had papillary microcarcinoma and received central node dissection after thyroidectomy. The sensory disorder around the chin persisted more than 6 months after surgery in all patients. RLN palsy revealed in one patient. Nobody had mental nerve palsy, and no infection developed.
Nakajo et al. (17) believe that this method is innovative and progressive and has not only a cosmetic advantage but also provides easy access to the central node compartment for dissection in endoscopic thyroid cancer surgery.
Yang et al. (18) compared in 2015 the complete endoscopic thyroidectomy via oral vestibular approach versus areola approach for treatment of thyroid diseases in patients. Aim of this study was to evaluate the feasibility, safety, and cosmetic results of 41 endoscopic thyroidectomies via the oral vestibular approach (ETOVA) compared with 41 endoscopic thyroidectomies via the areola approach (ETAA) in patients with thyroid diseases. Both the ETOVA and the ETAA procedures are feasible for thyroid diseases. The ETOVA eliminated skin incision scars and gained better cosmetic results in the short-term follow-ups, and the trauma was the same between the two approaches.
Liu (19) reported on a transoral and transtracheal experimental technique. In this study he explored its feasibility in animal models. Transtracheal endoscopic thyroidectomy was performed in anesthetized dogs and pigs. The endoscope was advanced into the pretracheal space via a longitudinal incision on the anterior tracheal wall. Hemithyroidectomies and partial lobectomy were performed using special double-lumen endotracheal tubes and conventional endoscopic instruments. The tracheal wall incision was closed using absorbable sutures, and the animals were sacrificed at day 5 after surgery. Hemithyroidectomy and partial thyroidectomy were successfully performed. No significant complications were encountered during surgery. They summarized that the transtracheal endoscopic thyroidectomy technique is feasible and has the potential to be an alternative method for other types of thyroid surgeries.
Neuromonitoring as an indicator for quality
In open and endoscopic thyroid surgery the loss of function of the RLN seems to be one of the major postoperative problems. In these endoscopic procedures even for the well-trained endocrine surgeon, the identification of the important anatomic structures is unfamiliar and more complicated than in open surgery. Neuromonitoring is a means of reducing the risk to the patient of damage to the RLN and provides functional guidance to the surgeon. The neuromonitoring system allows the surgeon to obtain and interpret triggered and spontaneous electrophysiological signals from the patient as surgery proceeds. Whether monitoring the RLN should be routinely done or not is controversially discussed. Some studies have shown the advantages of such a procedure, others showed also good results without it in their patients (20,21). The transoral resection of the thyroid gland seems to be a promising new and totally endoscopic, minimally invasive procedure. We now intend to show that the neuromonitoring system can be used in this procedure, making it just as safe for the RLN as any other thyroid resection (12) as we could proof in our porcine models (Figures 3,4).
Possible ways to the “perfect” transoral procedure
For the clinical, not experimental implementation of transoral thyroid surgery patient risk must be minimized. So it seems to be best to combine this new transoral approach with procedures that have been proven to be feasible and successful—so-called hybrid technique—until better instruments for endoscopic thyroidectomy have been developed (22). Developing such new instruments only makes sense when the technique has been shown to be promising. One such hybrid technique is preparation with a collar access using a 3-mm trocar and a 5-mm camera for creating the suprasternal space under the superficial collar fascia as the anterior collar approach in patients (23) or axillary approach then entering this cave via the transoral approach by using an endoscopic obturator under visual control to introduce the third instrument for triangulated preparation followed by transoral removal of thyroid tissue via the tube. With such a procedure we have first experiences in patients. It could be an important step towards safe endoscopic and minimally invasive thyroid resection in the future, because transoral thyroid surgery must still be considered as an experimental procedure (24). The transoral procedure should only be performed in highly specialized centres for endocrine and endoscopic surgery. For avoiding a learning curve in patients and achieving the best results a combination with endoscopic non-transoral techniques—so-called hybrid techniques—might be useful.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Witzel K, von Rahden BH, Stein HJ. The effect of ultrasound dissection in thyroid surgery. Eur Surg Res 2009;43:241-4. [Crossref] [PubMed]
- Dralle H, Sekulla C, Haerting J, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery 2004;136:1310-22. [Crossref] [PubMed]
- Shimizu K, Tanaka S. Asian perspective on endoscopic thyroidectomy -- a review of 193 cases. Asian J Surg 2003;26:92-100. [Crossref] [PubMed]
- Prisman E, Patsias A, Genden EM. Transoral robotic excision of ectopic lingual thyroid: Case series and literature review. Head Neck 2015;37:E88-91. [Crossref] [PubMed]
- Jiang XZ, Chen BS, Wang WC, et al. The diagnosis and the treatment on lingual thyroid. Shanghai Kou Qiang Yi Xue 1993;2:73-6. [PubMed]
- Witzel K, von Rahden BH, Kaminski C, et al. Transoral access for endoscopic thyroid resection. Surg Endosc 2008;22:1871-5. [Crossref] [PubMed]
- Benhidjeb T, Wilhelm T, Harlaar J, et al. Natural orifice surgery on thyroid gland: totally transoral video-assisted thyroidectomy (TOVAT): report of first experimental results of a new surgical method. Surg Endosc 2009;23:1119-20. [Crossref] [PubMed]
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral thyroid and parathyroid surgery. Surg Endosc 2010;24:1261-7. [Crossref] [PubMed]
- Park JO, Kim CS, Song JN, et al. Transoral endoscopic thyroidectomy via the tri-vestibular routes: results of a preclinical cadaver feasibility study. Eur Arch Otorhinolaryngol 2014;271:3269-75. [Crossref] [PubMed]
- von Renteln D, Vassiliou MC, Rösch T, et al. Triangulation: the holy grail of endoscopic surgery? Surg Endosc 2011;25:1355-7. [Crossref] [PubMed]
- Henry JF. Minimally invasive surgery of the thyroid and parathyroid glands. Br J Surg 2006;93:1-2. [Crossref] [PubMed]
- Witzel K, Benhidjeb T. Monitoring of the recurrent laryngeal nerve in totally endoscopic thyroid surgery. Eur Surg Res 2009;43:72-6. [Crossref] [PubMed]
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral thyroid and parathyroid surgery--development of a new transoral technique. Surgery 2011;150:108-15. [Crossref] [PubMed]
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral parathyroid surgery--a new alternative or nonsense? Langenbecks Arch Surg 2014;399:741-5. [Crossref] [PubMed]
- Cai C, Huang Y, Zhang T, et al. Anatomical study of surgical approaches for minimally invasive transoral thyroidectomy: eMIT and TOPP. Minim Invasive Ther Allied Technol 2015;24:340-4. [Crossref] [PubMed]
- Lee HY, Richmon JD, Walvekar RR, et al. Robotic transoral periosteal thyroidectomy (TOPOT): experience in two cadavers. J Laparoendosc Adv Surg Tech A 2015;25:139-42. [Crossref] [PubMed]
- Nakajo A, Arima H, Hirata M, et al. Trans-Oral Video-Assisted Neck Surgery (TOVANS). A new transoral technique of endoscopic thyroidectomy with gasless premandible approach. Surg Endosc 2013;27:1105-10. [Crossref] [PubMed]
- Yang J, Wang C, Li J, et al. Complete Endoscopic Thyroidectomy via Oral Vestibular Approach Versus Areola Approach for Treatment of Thyroid Diseases. J Laparoendosc Adv Surg Tech A 2015;25:470-6. [Crossref] [PubMed]
- Liu E, Qadir Khan A, Niu J, et al. Natural Orifice Total Transtracheal Endoscopic Thyroidectomy Surgery: First Reported Experiment. J Laparoendosc Adv Surg Tech A 2015;25:586-91. [Crossref] [PubMed]
- Miccoli P, Berti P, Frustaci GL, et al. Video-assisted thyroidectomy: indications and results. Langenbecks Arch Surg 2006;391:68-71. [Crossref] [PubMed]
- Chan WF, Lang BH, Lo CY. The role of intraoperative neuromonitoring of recurrent laryngeal nerve during thyroidectomy: a comparative study on 1000 nerves at risk. Surgery 2006;140:866-72; discussion 872-3. [Crossref] [PubMed]
- Witzel K. Hybrid technologies for determining optimal approach in endoscopic thyroidectomy. Surg Endosc 2009;23:456. [Crossref]
- Messenbӓck FG. Endoskopische Schilddrüsenchirurgie. Chir Prax 2004;63:647-57.
- Benhidjeb T, Witzel K, Stark M, et al. Transoral thyroid and parathyroid surgery: still experimental! Surg Endosc 2011;25:2411-3. [Crossref] [PubMed]



