Fast and simple fat grafting of the breast
Introduction
In spite of the ongoing debate about the oncologic safety of fat grafting (FG) most plastic surgeons tend to believe that the benefits outweighs the risks (1,2). The use of FG in breast conserving, reconstructive and aesthetic breast surgery escalates at a rapid pace. The main indications for FG are correction of shape and volume. However, despite this, there is still no consensus about the optimal FG technique (3).
The purpose of this paper is to share our experience using a simple and fast sedimentation based FG technique.
Patients and methods
This retrospective study included 176 women undergoing FG of the breast between March 2010 to July 2014 at the Departments of Plastic Surgery, Lillebaelt Hospital, Denmark and Telemark Hospital, Norway. We recorded patient demographics, indications for surgery, operative time, number of procedures, donor site, fat volume, types of complications and time to follow-up.
Surgical technique
The majority of procedures were performed in general anaesthesia using a solution of epinephrine 1:1,000,000 per liter of saline for tumescence. When performed in local anaesthesia we used Klein’s solution for FG containing 0.05% to 0.1% lidocaine, epinephrine 1:1,000,000. Two similar techniques were used for fat harvest, one using syringes, the other using a liposuction device in combination with a canister. In the visualized surgery (Figure 1) we used a liposuction device connected to a disposable collection canister (Shippert Medical, USA) for collection of the fat graft.

The fat and water phase were separated by sedimentation in 60 mL syringes for approximately 5-10 minutes, simply because this seems to be the time it takes for the liquid and fat phase to separate. The ratio between fat and liquid after sedimentation was usually 45:55. The excess liquid was then removed leaving the fat, which was then transferred to 10-20 cc syringes for grafting.
The skin was perforated using an 18-gauge cannula allowing for injection of the FG to the breast in the subcutaneous and subglandular plane. Needle dermatofascial release was performed using 18-gauge cannulas or a V-shaped dissection cannula for release of dermatofascial adhesions and scar tissue.
Results
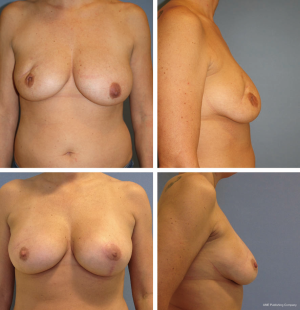
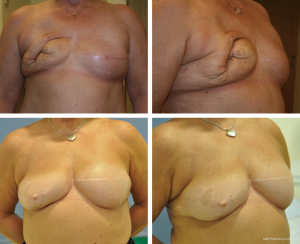
We performed 348 FG’s of the breasts in 176 patients aged 53 (range, 22-71): 19.8% were smokers (35/176), 9% were hypertensive (16/176) and 2% had diabetes (3/176). The FG’s were performed to correct shape and volume following; delayed breast reconstruction (DBR) in 35% (123/348), immediate breast reconstruction 30% (104/348), disfiguration due to scar tissue and/or following breast conserving surgery (BCS) in 21% (73/348) (Figure 2). The remaining 14% (48/348) were correction for correction of breast asymmetry, tuberous and constrictive breast conditions (Table 1).
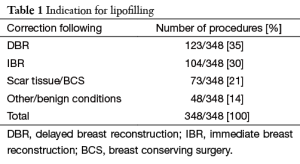
Full table
The FG procedure can be performed in 30 minutes by experienced surgeons in most cases. In this series 43% (75/176) had one FG and 57% (101/176) had multiple (range, 2-8). The abdomen was the preferred donor site, 83% (289/348) followed by the flanks/back 26% (90/348), thighs 19% (65/348), ipsi- and contralateral thorax 7% (23/348) and arms 3% (10/348). In the majority of cases one region was used as donor site, but in skinny patients more regions was necessary. The median volume fat harvested was 270 mL (range, 50-750 mL) and volume injected 120 mL (range, 20-375 mL). Minor complications occurred in 2% (8/348) of procedures, necrosis 0.5% (2/348), local infection 0.1% (1/348) and asymptomatic oil cysts 1.5% (5/348).
Discussion
We have performed 348 fast and easy low vacuum and sedimentation based FG procedures to the breast. The FG can be performed in 30 minutes by experienced surgeons and is simpler and less time consuming than the centrifuge based method (5-7).
We find this simple setup appropriate since no technique has proven to be better than others. One reason is that we simply lack a reliable tool to measure fat survival and volume increase following FG (3,8). The encountered complications were similar to other studies, namely fat necrosis, infection and oil cysts (9-11). The most frequent observed complication was oil cysts, which compares to the findings of other studies (10,12-14). Oil cysts in this study were cysts which could be palpated and then confirmed by ultrasonography. We did not routinely scan patients; however incidental findings were always easily identified as benign by ultrasonography or mammography. The overall complication rate was acceptable (2%) which compares to the complication rate of 2.8% reported by Petit et al. (14). The oil cysts occurred in early large volume FG’s which has leaded us to change our approach and reduce the injected volumes. With experience we have found that less is more, which is in line with the findings of others (6).
We have observed that FG improves skin quality in irradiated breasts. This is in concordance to several reports that has shown promising results using FG to radiated breasts thereby enabling reconstruction with implants. This could not have been possible without the use of FG (15-21).
We used FG to optimize and/or correct shape and volume following BCS, immediate and DBRs as well as tuberous and constrictive breasts, breast asymmetry and simple augmentation, which is similar to the indications published in other series (22-26) (Figure 3). We combined FG with dermatofascial release in most cases, which we use to optimize the aesthetic results as reported by others (13,27-29).
It has been questioned if FG can induce or fuel dormant cancer cells and there may be a higher risk of local events in patients with intraepithelial neoplasia following FG (30,31). However, a recent prospective study by Gale et al. showed no evidence of an increased oncologic risk in women treated with FG for breast cancer (32).
When it comes to adipose derived stem cells (ADSC), there seems to be more questions than answers regarding the oncologic safety. The adipose derived progenitor cells used for reconstruction following breast cancer have been found to stimulate local and metastatic breast cancer progression in murine models (33,34). We will have to await further studies and longer follow-up to answer the question about the oncologic safety of using ADSC-enriched solutions for grafting. However, there is no clinical evidence suggesting that there is a higher recurrence rate in patients receiving simple FG compared to controls albeit simple FG solutions also contain stem cells.
Conclusions
Simple fat harvesting using low vacuum and preparation by sedimentation is a fast and effective method to perform FG successfully for correction of shape and volume deficits of the breast following both ablative surgery as well as benign conditions with a high margin of safety.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kling RE, Mehrara BJ, Pusic AL, et al. Trends in autologous fat grafting to the breast: a national survey of the american society of plastic surgeons. Plast Reconstr Surg 2013;132:35-46. [PubMed]
- Skillman J, Hardwicke J, Whisker L, et al. Attitudes of U.K. breast and plastic surgeons to lipomodelling in breast surgery. Breast 2013;22:1200-4. [PubMed]
- Ross RJ, Shayan R, Mutimer KL, et al. Autologous fat grafting: current state of the art and critical review. Ann Plast Surg 2014;73:352-7. [PubMed]
- Kristensen RN, Gunnarsson GL, Børsen-Koch M, et al. Simple sedimentation based fat grafting (FG) of the breast. Asvide 2015;2. [Epub ahead of print]. Available online: http://www.asvide.com/articles/679
- Coleman SR, Saboeiro AP. Fat grafting to the breast revisited: safety and efficacy. Plast Reconstr Surg 2007;119:775-85; discussion 786-7. [PubMed]
- ELFadl D. Lipomodelling of the breast: a review. Breast 2010;19:202-9. [PubMed]
- Missana MC, Laurent I, Barreau L, et al. Autologous fat transfer in reconstructive breast surgery: indications, technique and results. Eur J Surg Oncol 2007;33:685-90. [PubMed]
- Saint-Cyr M, Rojas K, Colohan S, et al. The role of fat grafting in reconstructive and cosmetic breast surgery: a review of the literature. J Reconstr Microsurg 2012;28:99-110. [PubMed]
- Hoppe DL, Ueberreiter K, Surlemont Y, et al. Breast reconstruction de novo by water-jet assisted autologous fat grafting--a retrospective study. Ger Med Sci 2013;11:Doc17. [PubMed]
- Hyakusoku H, Ogawa R, Ono S, et al. Complications after autologous fat injection to the breast. Plast Reconstr Surg 2009;123:360-70; discussion 371-2. [PubMed]
- Mu DL, Luan J, Mu L, et al. Breast augmentation by autologous fat injection grafting: management and clinical analysis of complications. Ann Plast Surg 2009;63:124-7. [PubMed]
- Castelló JR, Barros J, Vázquez R. Giant liponecrotic pseudocyst after breast augmentation by fat injection. Plast Reconstr Surg 1999;103:291-3. [PubMed]
- Ho Quoc C, Sinna R, Gourari A, et al. Percutaneous fasciotomies and fat grafting: indications for breast surgery. Aesthet Surg J 2013;33:995-1001. [PubMed]
- Petit JY, Lohsiriwat V, Clough KB, et al. The oncologic outcome and immediate surgical complications of lipofilling in breast cancer patients: a multicenter study--Milan-Paris-Lyon experience of 646 lipofilling procedures. Plast Reconstr Surg 2011;128:341-6. [PubMed]
- Cigna E, Ribuffo D, Sorvillo V, et al. Secondary lipofilling after breast reconstruction with implants. Eur Rev Med Pharmacol Sci 2012;16:1729-34. [PubMed]
- Panettiere P, Marchetti L, Accorsi D.. The serial free fat transfer in irradiated prosthetic breast reconstructions. Aesthetic Plast Surg 2009;33:695-700. [PubMed]
- Ribuffo D, Atzeni M, Guerra M, et al. Treatment of irradiated expanders: protective lipofilling allows immediate prosthetic breast reconstruction in the setting of postoperative radiotherapy. Aesthetic Plast Surg 2013;37:1146-52. [PubMed]
- Rigotti G, Marchi A, Galiè M, et al. Clinical treatment of radiotherapy tissue damage by lipoaspirate transplant: a healing process mediated by adipose-derived adult stem cells. Plast Reconstr Surg 2007;119:1409-22; discussion 1423-4. [PubMed]
- Salgarello M, Visconti G, Rusciani A.. Breast fat grafting with platelet-rich plasma: a comparative clinical study and current state of the art. Plast Reconstr Surg 2011;127:2176-85. [PubMed]
- Sarfati I, Ihrai T, Kaufman G, et al. Adipose-tissue grafting to the post-mastectomy irradiated chest wall: preparing the ground for implant reconstruction. J Plast Reconstr Aesthet Surg 2011;64:1161-6. [PubMed]
- Serra-Renom JM, Muñoz-Olmo JL, Serra-Mestre JM. Fat grafting in postmastectomy breast reconstruction with expanders and prostheses in patients who have received radiotherapy: formation of new subcutaneous tissue. Plast Reconstr Surg 2010;125:12-8. [PubMed]
- Bonomi R, Betal D, Rapisarda IF, et al. Role of lipomodelling in improving aesthetic outcomes in patients undergoing immediate and delayed reconstructive breast surgery. Eur J Surg Oncol 2013;39:1039-45. [PubMed]
- Kanchwala SK, Glatt BS, Conant EF, et al. Autologous fat grafting to the reconstructed breast: the management of acquired contour deformities. Plast Reconstr Surg 2009;124:409-18. [PubMed]
- Panettiere P, Accorsi D, Marchetti L, et al. Large-breast reconstruction using fat graft only after prosthetic reconstruction failure. Aesthetic Plast Surg 2011;35:703-8. [PubMed]
- Spear SL, Wilson HB, Lockwood MD. Fat injection to correct contour deformities in the reconstructed breast. Plast Reconstr Surg 2005;116:1300-5. [PubMed]
- Weichman KE, Broer PN, Tanna N, et al. The role of autologous fat grafting in secondary microsurgical breast reconstruction. Ann Plast Surg 2013;71:24-30. [PubMed]
- Derder M, Whitaker IS, Boudana D, et al. The use of lipofilling to treat congenital hypoplastic breast anomalies: preliminary experiences. Ann Plast Surg 2014;73:371-7. [PubMed]
- Ho Quoc C, Delaporte T, Meruta A, et al. Breast asymmetry and pectus excavatum improvement with fat grafting. Aesthet Surg J 2013;33:822-9. [PubMed]
- Ho Quoc C, Piat JM, Michel G, et al. Fat grafting to improve severe tuberous breast. J Gynecol Obstet Biol Reprod (Paris) 2015;44:503-9. [PubMed]
- Lohsiriwat V, Curigliano G, Rietjens M, et al. Autologous fat transplantation in patients with breast cancer: "silencing" or "fueling" cancer recurrence? Breast 2011;20:351-7. [PubMed]
- Petit JY, Rietjens M, Botteri E, et al. Evaluation of fat grafting safety in patients with intraepithelial neoplasia: a matched-cohort study. Ann Oncol 2013;24:1479-84. [PubMed]
- Gale KL, Rakha EA, Ball G, et al. A case-controlled study of the oncologic safety of fat grafting. Plast Reconstr Surg 2015;135:1263-75. [PubMed]
- Simorre M, Chaput B, Voglimacci Stephanopoli M, et al. Lipofilling in breast reconstruction: is there any population with higher risk of local recurrence? Literature systematic review. Gynecol Obstet Fertil 2015;43:309-18. [PubMed]
- Bertolini F, Petit JY, Kolonin MG. Stem cells from adipose tissue and breast cancer: hype, risks and hope. Br J Cancer 2015;112:419-23. [PubMed]


