
Angiomyolipoma of the left adrenal gland: a case report and literature review
Introduction
Angiomyolipoma (AML) is part of a family of neoplasms, and is composed of blood vessels, muscle cells, and adipose tissue (1). AML is a rare mesenchymal tumor, most commonly found in the liver and kidney, but rarely in the spleen, bone, lungs, retroperitoneum, and so on (2,3). Adrenal AML is a rare type of solid tumor. Only 21 cases of adrenal AML have been reported in the English-language literature. The clinical manifestations of AML are atypical; some patients present with abdominal pain, but many are asymptomatic. The majority of adrenal AMLs are discovered incidentally during a health check-up or during imaging studies for other disorders of the abdomen. Adrenal AML is rare in clinical settings, and as the studies and literature reports on this disease are few, our understanding of the disease is limited (4-6). In this article, we describe the clinical presentation, imaging features, and treatment of a patient with a left adrenal AML, and review the relevant literature. We also analyzed the imaging findings to further improve understandings and the imaging diagnosis level of this disease.
We present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/gs-21-244).
Case presentation
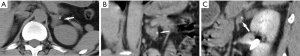
A 40-year-old male underwent his first abdominal routine computed tomography (CT) revealing a left adrenal mass some 3 months ago. One months later, the patient examined his second bilateral renal CT plain and contrast-enhanced scan at our hospital,where a small oval-bounded mass was detected in the left adrenal gland (see Figure 1). Two months later, a routine abdominal ultrasound (US) showed a hypoechoic area of 21 mm × 15 mm in the left adrenal gland. The patient was then admitted to our hospital for further evaluation, management, and surgical treatment.
The patient displayed no symptoms, no obvious mass was found in an abdominal physical examination, and the peritoneal irritation sign was negative. A specialist examination revealed mild tenderness of the bladder. A history of a duodenal ulcer and an endoscopic colon polypectomy were documented. The laboratory investigations, including patient’s epinephrine, adrenocorticotropic hormone, 24-hour urinary catecholamine, plasma cortisol, and aldosterone levels were all within the normal ranges.
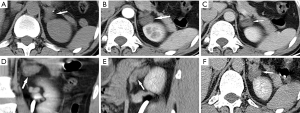
A contrast-enhanced CT showed a round mass of 16 mm × 23 mm round mass in the left adrenal gland with mild enhancement scan (see Figure 2). On a basis of the CT imaging results and the patient’s medical history, we made a preliminary diagnosis of left adrenal adenoma, and the patient was advised to have the mass surgically removed.
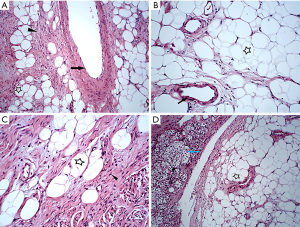
The patient subsequently underwent a retroperitoneal laparoscopic left adrenal resection under general anesthesia. During the operation, a yellowish oval mass of 2.5 cm × 2.5 cm was found in the upper pole of the left adrenal gland, which adhered to the surrounding soft tissue. Intraoperatively, the patient’s vital signs were stable, postoperative recovery was good, and the incision was at the first stage of healing. The postoperative pathology results showed that the tumor was composed of adipose tissue, abnormally formed small blood vessels, and smooth muscle cells (see Figure 3). Accordingly, we ultimately diagnosed AML of left adrenal. After 8 days, the patient had recovered without any discomfort, and was discharged from the hospital.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Literature review
Adrenal AML is very rare. We searched the Medline, Web of Science, PubMed, and Ovid databases for English-language case reports and cases of adrenal AML using the following key words and phrases: (Adrenal or Adrenal Glands or Gland of Adrenal or Glands Adrenal) and (Angiomyolipoma or Angiomyolipomas or Rare Adrenal Tumors). We screened the literature published between January 1, 1990 and December 31, 2020. A total of 18 full-text articles of 21 cases were identified, and carefully read and analyzed. For each case (including our case), the first author and publication year, and details of the patient’s sex, age, tumor size, affected side, presentation, imaging characteristics, surgery, and follow-up results were noted (see Table 1).

Full table
In relation to the 22 reported cases (including our case), adrenal AML patients had a median age of 45.5 years. Of the patients, 8 were male, and 14 were female. Notably, 10 of the 22 cases had tumors on the right side, and of these patients, most (8/10) were female. Conversely, 12 of the 22 cases had tumors on the left side, and of these patients, half (6/12) were male. Interestingly, the age distribution of female patients ranged from 40 to 60 years old, and most reported abdominal back pain. Conversely, the ages of the male patients varied greatly, their clinical manifestations were diverse, and there were no reports of clinical symptoms or abdominal pain. All cases of the adrenal AMLs were nonfunctional (7), and ranged in size of tumor from 0.2–17.3 cm; 86% of the masses exceeded 4.0 cm.
Discussion
The term AML was first coined by Morgan in 1951 and describes a benign renal tumor composed of blood vessels, muscle, and fat (8). AML is now thought to pertain to a group of tumors that are of perivascular epithelioid cell origin (2,3). AML is usually occurred in the kidneys and liver, but is rare in extrarenal locations. As few as 21 documented cases of adrenal AML have been reported.
Adrenal AMLs have no specific symptoms. A small number of patients have presented with abdominal pain; however, most patients are asymptomatic. AML is usually found occasionally during a medical examination or a routine US and CT examination for another unrelated disease. Our patient was asymptomatic, and only the specialist examination revealed mild tenderness of the bladder. The tumor was incidentally found during CT examinations for an unrelated disease.
Radiological examinations [e.g., US, CT and magnetic resonance imaging (MRI) examinations] play a significant role in the diagnosis of adrenal AML; however, the proportion of the components may effect imaging features (1). Adrenal AML generally manifests on CT imaging as ovoid or round with well-defined borders, with calcification and fat density, and no or mild enhancement. When AML is large (>4 cm) or heterogeneous and accompanied by dispersive calcification, it can easily be misdiagnosed as a malignant tumor (4,5,9-11). In one reported case, the adrenal AML presented similarly to malignant tumor metastasis (1). As mentioned above, the image in our case showed that the tumor was oval with a clear boundary, punctate calcification, and slight enhancement.
To make a final diagnosis of adrenal AML, which contains blood vessels, smooth muscle cells, and adipocytes, a histopathological examination needs to be conducted (2). Thus, it is necessary to use surgery to treat adrenal AML. Our review of previously published cases of adrenal AML, including our case (see Table 1), revealed that all 22 reported cases of adrenal AML were treated surgically. Among them, laparoscopic adrenalectomy has a number of advantages, as it is minimally invasive and results in fewer complications, with a lower mortality rate compared with open surgery (2,12,13). In our case, the patient underwent a retroperitoneal laparoscopic left adrenal resection under general anesthesia, and had no postoperative complications.
Conclusions
In conclusion, AML is a mesenchymal cell tumor that belongs to the group of perivascular epithelioid tumors. It is usually found in the kidneys. Extrarenal AML is unusual, and the adrenal gland is an extremely rare location. AML is generally detected incidentally by radiologists during imaging for a physical examination or unrelated imaging process. Due to its non-specific symptoms, signs and imaging findings, clinical diagnoses of adrenal AML may be difficult to make and easily be misdiagnosed. Thus, more clinical and imaging information about this disease is necessary for diagnosis, differential diagnosis, and treatment. Adrenal AML is rare, but a diagnosis of AML should be made if the adrenal mass has smooth edges, has well-defined boundaries, and is non-enhanced with fat density and calcification. Radiologically, the presence of fat, soft tissue, and feeding vessels helps to distinguish AML from other tumors. Due to the increasing number of health screening programs using imaging around the world, we believe that more cases of adrenal AML will be reported in the literature in the future.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/gs-21-244
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/gs-21-244). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the ethics committee of the Affiliated Hospital of Zunyi Medical University, and informed consent was obtained from the patient for the anonymous use of the clinical, imaging, and histologic data for publication. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yang Y, Hu J, Zhang J, et al. Angiomyolipoma of the adrenal gland: clinical experience and literature review. Ann Transl Med 2020;8:654. [Crossref] [PubMed]
- Li W, Pang H, Cao Y, et al. High 18F-Fluorodeoxyglucose Uptake in Adrenal Angiomyolipoma: Case Report and Review of Literature. Medicine (Baltimore) 2015;94:e900 [Crossref] [PubMed]
- Ghimire O, Wenzheng L, Huaping L, et al. Angiomyolipoma of the Adrenal Gland: A Report of Two Cases and Review of the Literature. Am J Case Rep 2017;18:989-94. [Crossref] [PubMed]
- Kwazneski Ii D, Merrill M, Young J, et al. Angiomyolipoma and Malignant PEComa: Discussion of Two Rare Adrenal Tumors. Case Rep Oncol Med 2016;2016:5204092 [Crossref] [PubMed]
- Yener O, Ozçelik A. Angiomyolipoma of the right adrenal gland. ISRN Surg 2011;2011:102743 [Crossref] [PubMed]
- Ahmed M, Mahmoud A, Mikael A, et al. Adrenal Angiomyolipoma: A Case Report. Cureus 2020;12:e6881 [PubMed]
- Lam AK. Lipomatous tumours in adrenal gland: WHO updates and clinical implications. Endocr Relat Cancer 2017;24:R65-R79. [Crossref] [PubMed]
- Lam KY, Lo CY. Adrenal lipomatous tumours: a 30 year clinicopathological experience at a single institution. J Clin Pathol 2001;54:707-12. [Crossref] [PubMed]
- Hu H, Xi X. Giant adrenal angiomyolipoma. J Clin Endocrinol Metab 2012;97:3835-6. [Crossref] [PubMed]
- Hafeez Bhatti AB, Dar FS, Pervez M. Adrenal angiomyolipoma. J Coll Physicians Surg Pak 2013;23:663-4. [PubMed]
- Kord Valeshabad A, Kravis B, Bremer W, et al. Angiomyolipoma of the Adrenal Glands. Clin Genitourin Cancer 2019;17:e553-e555. [Crossref] [PubMed]
- Spartalis E, Drikos I, Ioannidis A, et al. Metastatic Carcinomas of the Adrenal Glands: From Diagnosis to Treatment. Anticancer Res 2019;39:2699-710. [Crossref] [PubMed]
- Antar A, Boyle A, Patel T. Angiomyolipoma of the Adrenal Gland: A Case Presentation and a Review of Adrenal Lipomatous Tumors. Urol Case Rep 2017;12:59-61. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)


