Breast reconstruction following conservative mastectomies: predictors of complications and outcomes
Introduction
Breast reconstruction following mastectomy can be performed using alloplastic techniques, most commonly tissue expansion followed by implant placement, or autologous techniques in which numerous flap options exist. The goal of breast reconstruction surgery, whether autologous or alloplastic, is to create a breast mound that appears as natural as possible under clothing, and ideally without clothing as well (1). To achieve this goal, certain patient factors and surgical factors that can influence outcomes and complication rates must be taken into consideration.
Patient factors affecting complication rates and outcomes in breast reconstruction that are typically investigated include radiation, chemotherapy, smoking, obesity, age, and medical comorbidities (1-3). Surgical factors common to both alloplastic and autologous reconstruction, such as the timing of the reconstruction and the use of fat grafting, have an effect on outcomes and complications (4-6).
In alloplastic reconstructions, patients are exposed to less surgical risk, fewer scars, less donor site morbidity and fewer irreversible consequences. However, surgical factors like implant type, number of surgical stages, and use of an acellular dermal matrix (ADM) can influence outcomes (7-10). Typical complications and their frequencies in four large series of alloplastic based reconstruction are displayed in Table 1.
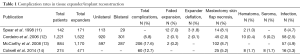
Full table
The optimal method of breast reconstruction differs from patient to patient, however reconstruction with autologous tissue can provide a long lasting, natural feeling breast mound (11). An obvious surgical factor that influences outcomes in autologous reconstruction is the type of autologous flap used. Complication rates in seven large series of autologous reconstruction patients are presented in Tables 2 and 3.
This article will describe patient factors and surgical factors that are predictors of outcomes and complications in alloplastic and autologous breast reconstruction.
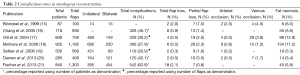
Full table
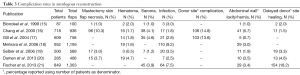
Full table
Tissue expander/implant based reconstruction
Patient factors influencing complications and outcomes
Radiation
Radiation adversely impacts expander/implant based breast reconstruction. Regardless of the timing of administration of radiation therapy, expander placement in a radio-treated field, radiation to temporary expanders postmastectomy, or radiation postmastectomy to implant, patients are at an increased risk of complications and reconstructive failure (2,22). Capsular contracture (23,24), infection (25) and wound-related complications are more common (1), with a wide spectrum of reported complication rates, ranging from 5% to 48% (26). Both aesthetic satisfaction and general satisfaction rates appear to be similar in expander/implant based reconstruction patients with and without radiotherapy (23,27). However, a long-term multicenter analysis demonstrated that patients receiving radiation had significantly lower satisfaction with the surgical outcome, as well as their psychosocial, sexual, and physical well-being (28). The increased complication rate does not exclude a patient requiring radiotherapy from an expander/implant based reconstruction, but the potential for the requirement of an autologous/prosthetic combination, in the form of a latissimus dorsi flap with implant, or a completely autologous reconstructive approach, should be discussed with the patient (1,2).
Chemotherapy
Both neoadjuvant and adjuvant chemotherapy regimens have been investigated in the setting of postoperative complications after mastectomy and breast reconstruction. It appears that neither neoadjuvant (2,13,29,30) nor adjuvant (12,13,30) chemotherapy increase the rate of complications or implant failure in patients undergoing postmastectomy expander/implants breast reconstruction, including in patients who undergo tissue expansion concomitantly. Bevacizumab in particular has been shown to affect surgical wound healing (31). To date, it has not been shown to increase complications in breast reconstruction, though evidence is limited (32). It is suggested to wait 6-8 weeks after completing bevacizumab therapy before performing surgery to minimize risks of complications (31).
Smoking
Smoking is universally considered to be a risk factor for surgical complications. For patients undergoing expander/implant based breast reconstruction, smoking is an independent risk factor for the development of perioperative complications and is associated with an increased risk of reconstructive failure (2,13,33). The rates of mastectomy skin flap necrosis and infectious complications are significantly higher in smokers compared to non-smokers (33). Complication rates as high as 37.9% in smokers have been reported (33), a 2-3 fold increase compared to non-smokers (13,33). Smokers are also five times more likely to experience reconstructive failure (13). The rate of complications in ex-smokers, defined as patients who have stopped smoking between 1 and 12 months preoperatively, can also be higher than non-smokers (33). The significant association between cigarette smoking and complications in the setting of tissue expander/implant reconstruction necessitates advising patients on smoking cessation and informing them of the increased risks.
Obesity/body mass index (BMI)
Obesity is defined as a BMI of 30 or greater. Obesity is an independent risk factor for the development of perioperative complications in patients undergoing expander/implant based reconstruction (13,14). Patients who are obese have nearly twice the risk of developing a perioperative complication (13). The risk of reconstructive failure is seven times greater in obese patients when compared to non-obese patients. Overweight patients, defined as a BMI of 25 or greater, are also at an increased risk of postoperative complications and reconstructive failure, though their risk is notably smaller (2,4,9).
Breast size
Some genetic factors that contribute to breast size are shared with those that influence BMI. Though the extent to which they are related is not clear, they are covariates (34). In patients undergoing expander/implant based reconstruction, large preoperative breast size, a cup size of D or larger, may be associated with an increased risk of complication and an increased risk of reconstructive failure (25). However, the effect of breast size has not been isolated from BMI and therefore it is not yet established whether large breast size on its own contributes to complications in these patients (2).
Age
Expander/implant reconstruction rates have been increasing in the elderly (28). Age is another factor that is universally associated with poorer outcomes following surgical procedures. Limited data exists on the relationship between age and outcomes in expander/implant based breast reconstruction. Age might be an independent risk factor for complications, though it does not appear to be a significant predictor of reconstructive failure (13). Patients older than 65 may have an increased risk of perioperative complications when compared to younger patients (13).
Medical comorbidities
Hypertension
In a review of 1,170 consecutive expander/implant reconstructions (884 patients) hypertension was found to be an independent risk factor for perioperative complications (13). In this series, a patient was classified as having hypertension if they required medical therapy. The risk was quantified as being two times greater than in a patient without hypertension. The odds of premature removal of a tissue expander and/or explantation of a permanent implant were four times higher in the hypertensive patient (13).
Diabetes mellitus
No significant associations between implant infection and diabetes have been found (13,35). Diabetes has not been shown to be an independent risk factor for the development of postoperative complications or for reconstructive failure (2,13,22). However, it is still advised that breast cancer patients attempt glycemic control in the perioperative period (2).
Prior breast conserving therapy (lumpectomy/irradiation combination)
Expander/implant based reconstruction may be an option in carefully selected patients with cancer recurrence following lumpectomy with irradiation. Patients who have undergone breast conserving therapy are at higher risk of early complications, of higher capsular contracture grade, and slightly inferior aesthetic results (36). Patients with severe breast deformity, multiple scars on the irradiated breast, or with tight/poor soft tissue might be appropriate candidates for the use of a latissimus dorsi flap to cover the prosthesis or for autologous reconstruction (36,37).
Mastectomy type: nipple sparing, skin sparing, skin reducing
The proportion of patients undergoing nipple sparing mastectomies (NSM) is increasing due to its perceived aesthetic benefits (38). The oncologic safety of NSMs is the greatest concern associated with this procedure, as nipple areola complex (NAC) involvement is related to tumor size, distance from the NAC, multicentricity, nuclear grade and lymph node status (38). A percentage of patients undergoing this procedure will have occult disease in the NAC [reported at 9.1% in one series of 66 patients (38)]. Wound healing problems within the NAC and either partial or complete NAC loss are unique complications to this procedure. Patients with larger breasts are at greater risk of nipple necrosis (39). The overall rate of complications in NSMs appears to be similar to that in skin-sparing mastectomies (SSM) (39). NAC preservation is associated with favorable results in aesthetic outcome, nipple sensitivity, and patient satisfaction (40).
SSMs are the conventional approach where the skin ellipse surrounding the NAC is extended (41). SSM is the most common type of mastectomy surgery performed for breast cancer treatment and does not have any unique complications.
Skin reducing mastectomies (SRMs) are performed using a Wise Pattern incision when skin envelope reduction is required (41). The vertical scar approach is an alternative to the Wise pattern technique (41). SRMs are often used for large breasts which in turn are at an increased risk of complications and reconstructive failure (25).
Surgical factors influencing complications and outcomes
Implant texture, shape, and material
Saline and silicone gel implants are available as the final implant material for expander/implant based postmastectomy reconstruction. All implant models have a bladder, or outside shell, made of solid silicone. The shell can be either textured or smooth. Modern expanders are textured to help prevent migration and early capsular contracture. Both saline and silicone implants can be either round, or anatomically shaped (like a teardrop). Patient satisfaction and aesthetic outcome does not appear to be affected by the shape (round or anatomic) of the implant used in the reconstruction (42,43).
Silicone gel implants are traditionally thought to provide a softer, more natural feeling breast when compared to saline implants (3). Decreased visible wrinkling has been thought to be an benefit of silicone implants, however this advantage is not always apparent (44). Patients receiving silicone implants have greater satisfaction with their breasts than those with saline implants (7,8). Silicone is no longer believed to be linked to immunologic (45) or other systemic diseases (3), however degradation of the silicone bladder over time will cause an implant to rupture (1). Thus, due to the possibility of silicone leakage into local tissues, some patients may choose saline implants for peace of mind.
Timing of reconstruction
Alloplastic reconstruction can be performed concomitantly with the mastectomy (immediate), or weeks, months or years later (delayed). While the timing of reconstruction can depend on many factors, immediate reconstruction is generally preferable as the mastectomy skin flaps are pliable and the native inframammary fold is present (1). The greatest benefit of immediate reconstruction could be the potential for fewer operations.
The impact of the timing of alloplastic breast reconstruction on outcomes is not clear. In a prospective, multicenter study, Alderman et al. found complications (both total and major) to be associated with immediate reconstructions (4). They suggested that the higher complication rate in the immediate setting might be due to any additional complications from the mastectomy procedure. In comparison, a review of a prospectively maintained database, from a single center examining only expander/implant reconstruction, did not find the timing of reconstruction to be a significant predictor of reconstructive failure (13). Satisfaction with immediate reconstruction has been reported to be greater than delayed reconstruction (5).
Single-stage breast reconstruction
Single-stage breast reconstruction is appropriate in a patient with small, non-ptotic breasts, and good quality skin and muscle (3). An implant is placed at the time of mastectomy and an ADM is used for support and implant coverage. This is also known as direct-to-implant reconstruction. The disadvantage of a direct-to-implant reconstruction is that aesthetic outcomes might not be as good as tissue expander/implant reconstructions, and often a revision procedure is required (3). Increasing breast cup size is associated with a need for early revision surgery (46). When direct-to-implant reconstruction is used in the right patient, both complication rates and revision rates appear to be comparable to two-staged tissue expander/implant based reconstruction (10). The role for this procedure in patients who will require post-mastectomy radiation is still unclear (46).
Use of an acellular dermal matrix
Traditional submuscular placement of a tissue expander requires the elevation of, and coverage with, the pectoralis major and serratus anterior (and sometimes the rectus abdominis). The use of an ADM has been increasing (47), whereby the pectoralis muscle is used to cover the prosthesis anteromedially, and the ADM is used for coverage laterally. This technique allows placement of tissue expanders with greater intraoperative fill volumes, and therefore fewer expansions are required before exchange for the permanent implant (47). In addition, it might have the potential to reduce the rate of encapsulation (48,49).
The use of ADM avoids elevation of the serratus anterior, which was once thought to decrease post-operative pain. However, a multicenter, blinded, randomized controlled trial did not demonstrate any reduction in postoperative pain when using ADM (50). In addition, an increased risk in complications has been demonstrated when using ADM, in particular, seroma (9,47,51), infection (51,52), and reconstructive failure (9,51) rates.
Use of an autologous flap
Tissue expansion/implant based reconstruction requires enough of a healthy skin envelope for a tension-free closure. The native skin and/or muscle envelope may not be adequate to undergo expansion if there are multiple scars, previous radiation injury, or if there was a large skin resection during mastectomy. In these cases, the use of an autologous flap (most commonly the latissimus dorsi myocutaneous flap) can provide coverage of the expander, and eventually implant. Patients requiring a salvage mastectomy after failed lumpectomy/irradiation can benefit from a latissimus dorsi/implant reconstruction (53).
Use of an autologous flap in previously irradiated breasts appears to reduce the incidence of implant related complications (54). The addition of an autologous flap to the implant based procedure increases the length and complexity of the operation, and adds a donor site with potential morbidity (3). In previously irradiated patients, complication rates and reconstructive failure rates in latissimus dorsi flap plus implant reconstruction are not statistically significant when compared to purely abdominal based autologous reconstruction (55). The most common complication when using a latissimus dorsi flap is a dorsal seroma (56).
Use of fat grafting
Fat grafting is an important tool to manage contour deformities in breast reconstruction. It can smooth out a “step-off” between the chest wall and implant, and help camouflage implant rippling. Fat grafting might help to achieve greater satisfaction, improve surrounding skin quality, and decrease implant exposure in patients who undergo implant based reconstruction after radiation (57,58). However, multiple procedures are often necessary, and potential complications include infection, fat necrosis, and oil cysts. Concerns have also been related to the theoretical interference with breast cancer detection (59), though the American Society of Plastic Surgeons task force did not find evidence to support this (60).
Volume of implant-based breast reconstruction practice
High volume implant-based breast reconstruction teams (surgical oncologist and plastic surgeon) tend to have lower complication rates when compared to low volume teams (where high volume teams had performed greater than 300 procedures together) (61). Low volume teams (fewer than 150 procedures performed together) were shown to have higher rates of infection (61). However other studies have failed to show this relationship between complications and surgical team volume (62).
Autologous reconstruction
Patient factors influencing complications and outcomes
Radiation
Radiation appears to negatively affect certain outcomes in autologous breast reconstruction. Radiation contributes to poor cosmesis (63,64), though does not appear to increase major complication rates (63,65). Flaps experience a higher rate of fat necrosis when irradiated. When irradiated muscle-sparing free transverse rectus abdominis myocutaneous (TRAM) flaps were compared to irradiated deep inferior epigastric perforator (DIEP) flaps, rates of fat necrosis were similar (66).
Challenges exist when radiotherapy is required after reconstruction (67). The autologous breast mound can compromise the design and delivery of radiotherapy (68), however increased tumor recurrence and worse clinical outcomes have not been demonstrated (1). Nevertheless, it has been suggested that the technique of delayed-immediate reconstruction (explained below under “Timing of Reconstruction”) can be used to balance aesthetic outcomes with the ability to provide optimal radiotherapy (67).
Chemotherapy
Neoadjuvant chemotherapy does not seem to be a predictor of flap loss, microvascular complications (18), or reoperation rate (69). Similarly, fascial healing at the donor site does not appear to be adversely affected (18). However, it has been associated with an increase in overall complications (70), early complications, in the form of wound healing difficulties, and late complications, such as fat necrosis (18). The timing of chemotherapy does not seem to have a significant effect on surgical outcomes (30).
Smoking
The effect of smoking on wound healing and blood supply is known to be harmful. In autologous breast reconstruction, studies have confirmed the deleterious relationship between smoking and post-operative complications (17,19), however the specific complications demonstrated have been variable. Smoking has been associated with an increased risk of wound infection (19), mastectomy flap necrosis (19,71,72), abdominal flap necrosis (19,71,72), abdominal hernia (71), and fat necrosis (19). On the other hand, some studies have not demonstrated an association between smoking and complications (4,18). Regardless, many reconstructive surgeons insist their patients quit smoking before proceeding with an autologous reconstruction.
Obesity/BMI
Patients with a higher BMI are prone to complications (9). Risks increase with the patient’s BMI, and obese patients have a greater risk of overall complications when compared to normal weight and overweight patients (73). This increased risk has partly been attributed to intraoperative technical difficulty, as obesity is associated with longer operative times in abdominally based autologous reconstruction (74). Increased health care resource consumption and greater hospital costs also appear to be consequences of the increased perioperative risk in these patients (74).
Overall, minor, early, and late complications are shown to be greater in the obese patient, with a 1.5- to 2-fold increase in flap complications (16) and a 3-fold increase in donor site complications (18). While the majority of overweight and even obese patients can complete autologous breast reconstruction successfully, they should be appropriately counselled that both the risk of failure, and complication rates are higher than normal weight patients (16,18). On the other hand, a retrospective analysis comparing implant reconstruction versus abdominal-based free flap reconstruction concluded that obese patients, particularly morbidly obese patients, experience lower failure rate with autologous reconstruction rather than implant reconstruction (75).
Age
In general, increasing age is associated with poorer outcomes following surgical procedures. Limited data exists on the relationship between age and outcomes in autologous breast reconstruction. Older patients are more likely to stay in hospital longer than younger patients (76) after autologous breast reconstruction. Rates of post-operative complications, including flap thrombosis (77), do not appear to be significantly different in elderly patients (76). Autologous breast reconstruction can be performed safely in the elderly (76), and age by itself should probably not be viewed as a risk factor for complications. However, older patients are more likely to have other medical comorbidities, and therefore this should be taken into account.
Other medical comorbidities
Hypertension
Hypertension is a risk factor for complications in the setting of autologous breast reconstruction. Hypertension is associated with both minor and major surgical complications (21), and with both breast and abdominal (donor) complications (17). It is also an independent predictor of unplanned readmission after autologous reconstruction, with the risk of readmission quantified as being at least 2 times greater than in a patient without hypertension (78).
Diabetes mellitus
The predisposition of diabetics to infection (79) and microvascular and macrovascular disease (79) are valid reasons to expect an increased rate of complications in these patients. Diabetes has been correlated with both minor surgical complications and post-operative medical complications (21). However, in other studies, diabetes mellitus has demonstrated trends toward association with complications but no statistically significant associations (17,18). Nevertheless, it is sensible for a breast reconstruction patient to attempt glycemic control in the perioperative period.
Mastectomy type: nipple sparing, skin sparing, skin reducing
A high quality autologous reconstruction can be obtained using either a NSM or SSM technique (80). With the preservation of the original skin envelope, inframammary fold, and the NAC in a NSM, the flap can be used to recreate the volume and shape of the original breast. SSM and immediate autologous reconstruction is an oncologically safe procedure (81). For patients undergoing NSMs, aesthetic results are significantly better when compared to SSM (82). However, in NSMs, anastomosis of the pedicle to the internal mammary artery can be difficult due to limited exposure (83), and traction during the operation can increase the chance of partial or complete nipple areola necrosis. While cancer recurrence in the NAC remains a concern, autologous reconstruction after NSM is a reasonable option in the appropriate patient (84).
Prior abdominal surgery
When planning to use an abdominal flap for autologous reconstruction, the finding of an abdominal scar on physical exam could potentially alter the approach to breast reconstruction due to concerns of flap loss and/or donor site complication. Prior abdominal surgery in patients undergoing TRAM based breast reconstruction is associated with minor, major, and overall complication rates (18). Most of the major complications involve partial flap loss (18). Donor site complication rates, including hernia/laxity and wound healing, are also found to be greater. Careful patient selection is especially important in these patients, as smokers with a subcostal scar have been found to have a greater than 6-fold increase in donor site complications (85).
Surgical factors influencing complications and outcomes
Free flap choice
The pedicled TRAM is most common method for autologous breast reconstruction in the United States (1,86,87). Common free tissue transfer options for reconstruction use tissue from the abdomen in the form of either a TRAM, DIEP, or superficial inferior epigastric artery (SIEA) flap. Autologous reconstruction can also be performed using tissue from the thigh or buttock in the form of transverse upper gracilis (TUG), superior gluteal artery perforator (SGAP), inferior gluteal artery perforator (IGAP), or profunda artery perforator (PAP) flaps. The distinct advantage of an autologous reconstruction is the ability to replace “like with like”, and provide the patient with a lifelong, natural feeling breast.
When comparing outcomes of pedicled TRAM reconstructions to free flap reconstructions, the incidence of complications (overall, flap-related and nonflap-related) was greater in free flaps in a review of over 2,000 flaps (88). However, after regression modelling these differences did not appear to be significant. The pedicled TRAM tends to be associated with more fat necrosis than free abdominal flaps (89,90) and with an increased risk of partial and total flap loss in obese patients (91). To decrease these types of complications, especially in “high risk” patients, a vascular delay procedure can be used, where the inferior vascular pedicle is ligated 2 to 3 weeks before reconstruction (92).
The criticism of the free TRAM flap has been related to morbidity from sacrificing the rectus muscle at the donor site (93,94). Patients reconstructed with a free TRAM flap have decreased abdominal strength and have twice the risk of an abdominal bulge or hernia compared to DIEP reconstructions (95). The DIEP flap is thought to offer patients decreased donor site morbidity. Although many studies are able to demonstrate the advantage of the DIEP with respect to the donor site objectively, changes in the ability to perform activities of daily living do not appear to be significantly different from TRAM patients (96). In a systematic review of studies comparing DIEP and free TRAM flaps, DIEP flaps were found to have a higher rate of flap-related complications, and a 2-fold increase in the risk of fat necrosis and flap loss compared to free TRAM flaps (95). Therefore the reconstructive advantage of the DIEP flap has remained uncertain, in general seems to be less reliable than the free TRAM flap, and has gained only cautious acceptance among many reconstructive surgeons (95).
The major benefit of the SIEA flap is the ability to harvest abdominal tissue without violating the abdominal wall fascia, therefore leaving both the fascia and rectus muscle intact and minimizing donor site morbidity (97). On the other hand, the flap has a smaller pedicle length and diameter (98), and flap size is limited to only half of the abdominal skin island for reconstruction (1). When compared to free TRAM and DIEP flaps, use of the SIEA flap has also been found to be a risk factor for flap thrombosis (77), and is associated with an increased risk of fat necrosis (1). The significantly higher rate of thrombotic complications associated with the SIEA flap limits the indications for this type of reconstruction.
Autologous reconstruction using tissue from the thigh or buttock (TUG, SGAP, IGAP, PAP) is less common, typically only indicated in patients who require a small to medium size breast reconstruction, have either abdominal scarring or limited abdominal tissue, and excess tissue in the thigh/buttock region. The literature describing outcomes and complications using autologous thigh/buttock flaps is in its infancy compared to abdominal based flaps.
Timing of reconstruction
Similar to alloplastic reconstruction, autologous reconstruction can be performed either immediately or in a delayed fashion with respect to the mastectomy. Immediate reconstruction potentially exposes the patient to fewer operations, can save resource costs (99,100), and gives the patient the best chance at a good aesthetic result (101). In delayed reconstruction, mastectomy skin flaps are often scarred and less compliant (1), and a higher rate of free flap thrombosis has been found to occur (77). However similar rates of both major and minor complications have been reported between patients undergoing either immediate or delayed reconstruction with a TRAM free-flap (102).
The requirement of post-mastectomy radiotherapy has been considered to be a relative contraindication to immediate reconstruction (103). An alternative strategy, known as “delayed-immediate” autologous reconstruction, has been used (104). This is a two stage approach in which a filled tissue expander is placed after mastectomy. If radiotherapy is not required, definitive autologous reconstruction is performed. If radiotherapy is required, the expander is deflated, radiotherapy is administered, the expander is re-inflated, and autologous reconstruction performed (104). When compared to “delayed” reconstruction, “delayed-immediate” has been shown to have similar flap-related complication rates, decreased rates of revision surgery (105), and a better aesthetic outcome (106).
Fat grafting
Fat grafting can be used to address step-off deformities (between the chest wall and the flap), intrinsic deformities (e.g., from fat necrosis) and extrinsic deformities (e.g., from radiation or scar contracture) (6). Fat grafting can also be used to help augment size in a volume-deficient reconstruction, therefore allowing certain patients with barely enough soft tissue for a microvascular free flap to undergo autologous reconstruction (107). In a review of mostly autologous reconstructed patients, aesthetic outcomes were significantly improved with fat grafting, though half of the patients required more than one procedure, and complications occurred in approximately 6% of procedures (6).
Volume of autologous breast reconstruction practice
High volume autologous breast reconstruction centers tend to have lower complication rates when compared to low and medium volume centers (where high volume was “greater than 44 procedures per year”) (108). Both surgery-specific and systemic complications were inversely related to volume of reconstruction at the center (108). When examining microsurgical cases, low-volume centers had a 2-fold increase in surgery-specific complications when compared to high-volume centers (108).
Summary
Alloplastic breast reconstruction outcomes can be negatively affected by certain patient factors. Pre- or post-mastectomy radiotherapy, smoking, increased BMI, hypertension, and prior breast conserving therapy are all associated with an increase in complications and/or inferior outcomes. Silicone gel implants provide a softer, more natural feeling breast and these patients appear to have greater satisfaction than those with saline implants. Patient satisfaction and aesthetic outcomes are not different between reconstructions that use either round or anatomically shaped implants. Immediate reconstruction, and the use of fat grafting techniques are likely to improve aesthetic outcomes.
Autologous breast reconstruction outcomes are affected in a deleterious manner by radiation, increased BMI, certain previous abdominal surgery, delayed reconstruction, smoking, hypertension, and most likely diabetes. When these risk factors are present, a free microvascular reconstructive technique is preferred over a pedicled flap for patients undergoing autologous reconstruction. Reduced donor site morbidity can be seen in DIEP flap reconstruction, compared to TRAM flap, but is more obvious in bilateral reconstructions. The use of the SIEA flap in breast reconstruction is limited due to the higher rate of vessel thrombosis. Other types of free flaps, TUG, SGAP, IGAP and PAP flaps, tend to be options when abdominal tissue is not available. Fat grafting can be used to improve aesthetic outcomes, and high volume centers are associated with fewer complications, especially in free flap reconstruction.
Offering patients an opportunity for breast reconstruction is an important component of the treatment for breast cancer. There are many options for both alloplastic and autologous reconstruction. Ultimately, patient and surgical risk factors should be considered in concert with the patient’s wishes when deciding upon a reconstructive strategy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Serletti JM, Fosnot J, Nelson JA, et al. Breast reconstruction after breast cancer. Plast Reconstr Surg 2011;127:124e-35e. [PubMed]
- Alderman A, Gutowski K, Ahuja A, et al. ASPS Clinical Practice Guideline Summary on Breast Reconstruction with Expanders and Implants. Plast Reconstr Surg 2014;134:648e-55e. [PubMed]
- Cordeiro PG. Breast reconstruction after surgery for breast cancer. N Engl J Med 2008;359:1590-601. [PubMed]
- Alderman AK, Wilkins EG, Kim HM, et al. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg 2002;109:2265-74. [PubMed]
- Fernández-Delgado J, Lopez-Pedraza MJ, Blasco JA, et al. Satisfaction with and psychological impact of immediate and deferred breast reconstruction. Ann Oncol 2008;19:1430-4. [PubMed]
- de Blacam C, Momoh AO, Colakoglu S, et al. Evaluation of clinical outcomes and aesthetic results after autologous fat grafting for contour deformities of the reconstructed breast. Plast Reconstr Surg 2011;128:411e-8e. [PubMed]
- McCarthy CM, Klassen AF, Cano SJ, et al. Patient satisfaction with postmastectomy breast reconstruction: a comparison of saline and silicone implants. Cancer 2010;116:5584-91. [PubMed]
- Macadam SA, Ho AL, Cook EF, et al. Patient satisfaction and health-related quality of life following breast reconstruction: patient-reported outcomes among saline and silicone implant recipients. Plast Reconstr Surg 2010;125:761-71. [PubMed]
- Antony AK, McCarthy CM, Cordeiro PG, et al. Acellular human dermis implantation in 153 immediate two-stage tissue expander breast reconstructions: determining the incidence and significant predictors of complications. Plast Reconstr Surg 2010;125:1606-14. [PubMed]
- Salzberg CA, Ashikari AY, Koch RM, et al. An 8-year experience of direct-to-implant immediate breast reconstruction using human acellular dermal matrix (AlloDerm). Plast Reconstr Surg 2011;127:514-24. [PubMed]
- Spear SL, Majidian A. Immediate breast reconstruction in two stages using textured, integrated-valve tissue expanders and breast implants: a retrospective review of 171 consecutive breast reconstructions from 1989 to 1996. Plast Reconstr Surg 1998;101:53-63. [PubMed]
- Cordeiro PG, McCarthy CM. A single surgeon's 12-year experience with tissue expander/implant breast reconstruction: part I. A prospective analysis of early complications. Plast Reconstr Surg 2006;118:825-31. [PubMed]
- McCarthy CM, Mehrara BJ, Riedel E, et al. Predicting complications following expander/implant breast reconstruction: an outcomes analysis based on preoperative clinical risk. Plast Reconstr Surg 2008;121:1886-92. [PubMed]
- Colwell AS, Tessler O, Lin AM, et al. Breast reconstruction following nipple-sparing mastectomy: predictors of complications, reconstruction outcomes, and 5-year trends. Plast Reconstr Surg 2014;133:496-506. [PubMed]
- Blondeel PN. One hundred free DIEP flap breast reconstructions: a personal experience. Br J Plast Surg 1999;52:104-11. [PubMed]
- Chang DW, Wang B, Robb GL, et al. Effect of obesity on flap and donor-site complications in free transverse rectus abdominis myocutaneous flap breast reconstruction. Plast Reconstr Surg 2000;105:1640-8. [PubMed]
- Gill PS, Hunt JP, Guerra AB, et al. A 10-year retrospective review of 758 DIEP flaps for breast reconstruction. Plast Reconstr Surg 2004;113:1153-60. [PubMed]
- Mehrara BJ, Santoro TD, Arcilla E, et al. Complications after microvascular breast reconstruction: experience with 1195 flaps. Plast Reconstr Surg 2006;118:1100-9; discussion 1110-1. [PubMed]
- Selber JC, Kurichi JE, Vega SJ, et al. Risk factors and complications in free TRAM flap breast reconstruction. Ann Plast Surg 2006;56:492-7. [PubMed]
- Damen TH, Morritt AN, Zhong T, et al. Improving outcomes in microsurgical breast reconstruction: lessons learnt from 406 consecutive DIEP/TRAM flaps performed by a single surgeon. J Plast Reconstr Aesthet Surg 2013;66:1032-8. [PubMed]
- Fischer JP, Sieber B, Nelson JA, et al. Comprehensive outcome and cost analysis of free tissue transfer for breast reconstruction: an experience with 1303 flaps. Plast Reconstr Surg 2013;131:195-203. [PubMed]
- Ascherman JA, Hanasono MM, Newman MI, et al. Implant reconstruction in breast cancer patients treated with radiation therapy. Plast Reconstr Surg 2006;117:359-65. [PubMed]
- Cordeiro PG, Pusic AL, Disa JJ, et al. Irradiation after immediate tissue expander/implant breast reconstruction: outcomes, complications, aesthetic results, and satisfaction among 156 patients. Plast Reconstr Surg 2004;113:877-81. [PubMed]
- McCarthy CM, Pusic AL, Disa JJ, et al. Unilateral postoperative chest wall radiotherapy in bilateral tissue expander/implant reconstruction patients: a prospective outcomes analysis. Plast Reconstr Surg 2005;116:1642-7. [PubMed]
- Francis SH, Ruberg RL, Stevenson KB, et al. Independent risk factors for infection in tissue expander breast reconstruction. Plast Reconstr Surg 2009;124:1790-6. [PubMed]
- Ho A, Cordeiro P, Disa J, et al. Long-term outcomes in breast cancer patients undergoing immediate 2-stage expander/implant reconstruction and postmastectomy radiation. Cancer 2012;118:2552-9. [PubMed]
- Krueger EA, Wilkins EG, Strawderman M, et al. Complications and patient satisfaction following expander/implant breast reconstruction with and without radiotherapy. Int J Radiat Oncol Biol Phys 2001;49:713-21. [PubMed]
- Albornoz CR, Matros E, McCarthy CM, et al. Implant breast reconstruction and radiation: a multicenter analysis of long-term health-related quality of life and satisfaction. Ann Surg Oncol 2014;21:2159-64. [PubMed]
- Song J, Zhang X, Liu Q, et al. Impact of neoadjuvant chemotherapy on immediate breast reconstruction: a meta-analysis. PLoS One 2014;9:e98225. [PubMed]
- Warren Peled A, Itakura K, Foster RD, et al. Impact of chemotherapy on postoperative complications after mastectomy and immediate breast reconstruction. Arch Surg 2010;145:880-5. [PubMed]
- Gordon CR, Rojavin Y, Patel M, et al. A review on bevacizumab and surgical wound healing: an important warning to all surgeons. Ann Plast Surg 2009;62:707-9. [PubMed]
- Kansal KJ, Dominici LS, Tolaney SM, et al. Neoadjuvant bevacizumab: surgical complications of mastectomy with and without reconstruction. Breast Cancer Res Treat 2013;141:255-9. [PubMed]
- Goodwin SJ, McCarthy CM, Pusic AL, et al. Complications in smokers after postmastectomy tissue expander/implant breast reconstruction. Ann Plast Surg 2005;55:16-9; discussion 19-20. [PubMed]
- Wade TD, Zhu G, Martin NG. Body mass index and breast size in women: same or different genes? Twin Res Hum Genet 2010;13:450-4. [PubMed]
- Nahabedian MY, Tsangaris T, Momen B, et al. Infectious complications following breast reconstruction with expanders and implants. Plast Reconstr Surg 2003;112:467-76. [PubMed]
- Cordeiro PG, Snell L, Heerdt A, et al. Immediate tissue expander/implast breast reconstruction after salvage mastectomy for cancer recurrence following lumpectomy/irradiation. Plast Reconstr Surg 2012;129:341-50. [PubMed]
- Butler CE, Kronowitz SJ. Discussion. Immediate tissue expander/implant breast reconstruction after salvage mastectomy for cancer recurrence following lumpectomy/irradiation. Plast Reconstr Surg 2012;129:351-3. [PubMed]
- Chen CM, Disa JJ, Sacchini V, et al. Nipple-sparing mastectomy and immediate tissue expander/implant breast reconstruction. Plast Reconstr Surg 2009;124:1772-80. [PubMed]
- Gould DJ, Hunt KK, Liu J, et al. Impact of surgical techniques, biomaterials, and patient variables on rate of nipple necrosis after nipple-sparing mastectomy. Plast Reconstr Surg 2013;132:330e-8e. [PubMed]
- Didier F, Radice D, Gandini S, et al. Does nipple preservation in mastectomy improve satisfaction with cosmetic results, psychological adjustment, body image and sexuality? Breast Cancer Res Treat 2009;118:623-33. [PubMed]
- Nava MB, Catanuto G, Pennati A, et al. Conservative mastectomies. Aesthetic Plast Surg 2009;33:681-6. [PubMed]
- Macadam SA, Ho AL, Lennox PA, et al. Patient-reported satisfaction and health-related quality of life following breast reconstruction: a comparison of shaped cohesive gel and round cohesive gel implant recipients. Plast Reconstr Surg 2013;131:431-41. [PubMed]
- Gahm J, Edsander-Nord A, Jurell G, et al. No differences in aesthetic outcome or patient satisfaction between anatomically shaped and round expandable implants in bilateral breast reconstructions: a randomized study. Plast Reconstr Surg 2010;126:1419-27. [PubMed]
- Cordeiro PG, McCarthy CM. A single surgeon's 12-year experience with tissue expander/implant breast reconstruction: part II. An analysis of long-term complications, aesthetic outcomes, and patient satisfaction. Plast Reconstr Surg 2006;118:832-9. [PubMed]
- Karlson EW, Hankinson SE, Liang MH, et al. Association of silicone breast implants with immunologic abnormalities: a prospective study. Am J Med 1999;106:11-9. [PubMed]
- Gdalevitch P, Ho A, Genoway K, et al. Direct-to-implant single-stage immediate breast reconstruction with acellular dermal matrix: predictors of failure. Plast Reconstr Surg 2014;133:738e-47e. [PubMed]
- Sbitany H, Serletti JM. Acellular dermis-assisted prosthetic breast reconstruction: a systematic and critical review of efficacy and associated morbidity. Plast Reconstr Surg 2011;128:1162-9. [PubMed]
- Stump A, Holton LH 3rd, Connor J, et al. The use of acellular dermal matrix to prevent capsule formation around implants in a primate model. Plast Reconstr Surg 2009;124:82-91. [PubMed]
- Basu CB, Leong M, Hicks MJ. Acellular cadaveric dermis decreases the inflammatory response in capsule formation in reconstructive breast surgery. Plast Reconstr Surg 2010;126:1842-7. [PubMed]
- McCarthy CM, Lee CN, Halvorson EG, et al. The use of acellular dermal matrices in two-stage expander/implant reconstruction: a multicenter, blinded, randomized controlled trial. Plast Reconstr Surg 2012;130:57S-66S. [PubMed]
- Kim JY, Davila AA, Persing S, et al. A meta-analysis of human acellular dermis and submuscular tissue expander breast reconstruction. Plast Reconstr Surg 2012;129:28-41. [PubMed]
- Brooke S, Mesa J, Uluer M, et al. Complications in tissue expander breast reconstruction: a comparison of AlloDerm, DermaMatrix, and FlexHD acellular inferior pole dermal slings. Ann Plast Surg 2012;69:347-9. [PubMed]
- Disa JJ, McCarthy CM, Mehrara BJ, et al. Immediate latissimus dorsi/prosthetic breast reconstruction following salvage mastectomy after failed lumpectomy/irradiation. Plast Reconstr Surg 2008;121:159e-64e. [PubMed]
- Chang DW, Barnea Y, Robb GL. Effects of an autologous flap combined with an implant for breast reconstruction: an evaluation of 1000 consecutive reconstructions of previously irradiated breasts. Plast Reconstr Surg 2008;122:356-62. [PubMed]
- Levine SM, Patel N, Disa JJ. Outcomes of delayed abdominal-based autologous reconstruction versus latissimus dorsi flap plus implant reconstruction in previously irradiated patients. Ann Plast Surg 2012;69:380-2. [PubMed]
- Pinsolle V, Grinfeder C, Mathoulin-Pelissier S, et al. Complications analysis of 266 immediate breast reconstructions. J Plast Reconstr Aesthet Surg 2006;59:1017-24. [PubMed]
- Serra-Renom JM, Munoz-Olmo JL, Serra-Mestre JM. Fat grafting in postmastectomy breast reconstruction with expanders and prostheses in patients who have received radiotherapy: formation of new subcutaneous tissue. Plast Reconstr Surg 2010;125:12-8. [PubMed]
- Ribuffo D, Atzeni M, Guerra M, et al. Treatment of irradiated expanders: protective lipofilling allows immediate prosthetic breast reconstruction in the setting of postoperative radiotherapy. Aesthetic Plast Surg 2013;37:1146-52. [PubMed]
- Spear SL, Wilson HB, Lockwood MD. Fat injection to correct contour deformities in the reconstructed breast. Plast Reconstr Surg 2005;116:1300-5. [PubMed]
- Gutowski KA. Current applications and safety of autologous fat grafts: a report of the ASPS fat graft task force. Plast Reconstr Surg 2009;124:272-80. [PubMed]
- Gfrerer L, Mattos D, Mastroianni M, et al. Assessment of patient factors, surgeons, and surgeon teams in immediate implant-based breast reconstruction outcomes. Plast Reconstr Surg 2015;135:245e-52e. [PubMed]
- Seth AK, Hirsch EM, Kim JY, et al. Two surgeons, one patient: the impact of surgeon-surgeon familiarity on patient outcomes following mastectomy with immediate reconstruction. Breast 2013;22:914-8. [PubMed]
- Spear SL, Ducic I, Low M, et al. The effect of radiation on pedicled TRAM flap breast reconstruction: outcomes and implications. Plast Reconstr Surg 2005;115:84-95. [PubMed]
- Carlson GW, Page AL, Peters K, et al. Effects of radiation therapy on pedicled transverse rectus abdominis myocutaneous flap breast reconstruction. Ann Plast Surg 2008;60:568-72. [PubMed]
- Berry T, Brooks S, Sydow N, et al. Complication rates of radiation on tissue expander and autologous tissue breast reconstruction. Ann Surg Oncol 2010;17 Suppl 3:202-10. [PubMed]
- Garvey PB, Clemens MW, Hoy AE, et al. Muscle-sparing TRAM flap does not protect breast reconstruction from postmastectomy radiation damage compared with the DIEP flap. Plast Reconstr Surg 2014;133:223-33. [PubMed]
- Kronowitz SJ, Robb GL. Radiation therapy and breast reconstruction: a critical review of the literature. Plast Reconstr Surg 2009;124:395-408. [PubMed]
- Motwani SB, Strom EA, Schechter NR, et al. The impact of immediate breast reconstruction on the technical delivery of postmastectomy radiotherapy. Int J Radiat Oncol Biol Phys 2006;66:76-82. [PubMed]
- Schaverien MV, Munnoch DA. Effect of neoadjuvant chemotherapy on outcomes of immediate free autologous breast reconstruction. Eur J Surg Oncol 2013;39:430-6. [PubMed]
- Deutsch MF, Smith M, Wang B, et al. Immediate breast reconstruction with the TRAM flap after neoadjuvant therapy. Ann Plast Surg 1999;42:240-4. [PubMed]
- Chang DW, Reece GP, Wang B, et al. Effect of smoking on complications in patients undergoing free TRAM flap breast reconstruction. Plast Reconstr Surg 2000;105:2374-80. [PubMed]
- Kroll SS. Necrosis of abdominoplasty and other secondary flaps after TRAM flap breast reconstruction. Plast Reconstr Surg 1994;94:637-43. [PubMed]
- Spear SL, Ducic I, Cuoco F, et al. Effect of obesity on flap and donor-site complications in pedicled TRAM flap breast reconstruction. Plast Reconstr Surg 2007;119:788-95. [PubMed]
- Fischer JP, Nelson JA, Sieber B, et al. Free tissue transfer in the obese patient: an outcome and cost analysis in 1258 consecutive abdominally based reconstructions. Plast Reconstr Surg 2013;131:681e-92e. [PubMed]
- Garvey PB, Villa MT, Rozanski AT, et al. The advantages of free abdominal-based flaps over implants for breast reconstruction in obese patients. Plast Reconstr Surg 2012;130:991-1000. [PubMed]
- Garvey PB, Buchel EW, Pockaj BA, et al. Outcomes after autologous breast reconstruction in elderly patients. Plastic Surgery 2004. Philadelphia, PA, USA, 2004.
- Masoomi H, Clark EG, Paydar KZ, et al. Predictive risk factors of free flap thrombosis in breast reconstruction surgery. Microsurgery 2014;34:589-94. [PubMed]
- Mlodinow AS, Ver Halen JP, Lim S, et al. Predictors of readmission after breast reconstruction: a multi-institutional analysis of 5012 patients. Ann Plast Surg 2013;71:335-41. [PubMed]
- Janis JE, Harrison B. Wound healing: part I. Basic science. Plast Reconstr Surg 2014;133:199e-207e. [PubMed]
- Gherardini G, Thomas R, Basoccu G, et al. Immediate breast reconstruction with the transverse rectus abdominis musculocutaneous flap after skin-sparing mastectomy. Int Surg 2001;86:246-51. [PubMed]
- Liang TJ, Wang BW, Liu SI, et al. Recurrence after skin-sparing mastectomy and immediate transverse rectus abdominis musculocutaneous flap reconstruction for invasive breast cancer. World J Surg Oncol 2013;11:194. [PubMed]
- Gerber B, Krause A, Reimer T, et al. Skin-sparing mastectomy with conservation of the nipple-areola complex and autologous reconstruction is an oncologically safe procedure. Ann Surg 2003;238:120-7. [PubMed]
- Munhoz AM, Montag E, Filassi JR, et al. Immediate nipple-areola-sparing mastectomy reconstruction: An update on oncological and reconstruction techniques. World J Clin Oncol 2014;5:478-94. [PubMed]
- Dao TN, Verheyden CN. TRAM flaps: a reconstructive option after bilateral nipple-sparing total mastectomy. Plast Reconstr Surg 2005;116:986-92. [PubMed]
- Losken A, Carlson GW, Jones GE, et al. Importance of right subcostal incisions in patients undergoing TRAM flap breast reconstruction. Ann Plast Surg 2002;49:115-9. [PubMed]
- Kulkarni AR, Sears ED, Atisha DM, et al. Use of autologous and microsurgical breast reconstruction by U.S. plastic surgeons. Plast Reconstr Surg 2013;132:534-41. [PubMed]
- Gurunluoglu R, Gurunluoglu A, Williams SA, et al. Current trends in breast reconstruction: survey of American Society of Plastic Surgeons 2010. Ann Plast Surg 2013;70:103-10. [PubMed]
- Gart MS, Smetona JT, Hanwright PJ, et al. Autologous options for postmastectomy breast reconstruction: a comparison of outcomes based on the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 2013;216:229-38. [PubMed]
- Andrades P, Fix RJ, Danilla S, et al. Ischemic complications in pedicle, free, and muscle sparing transverse rectus abdominis myocutaneous flaps for breast reconstruction. Ann Plast Surg 2008;60:562-7. [PubMed]
- Garvey PB, Buchel EW, Pockaj BA, et al. DIEP and pedicled TRAM flaps: a comparison of outcomes. Plast Reconstr Surg 2006;117:1711-9; discussion 1720-1.
- Moran SL, Serletti JM. Outcome comparison between free and pedicled TRAM flap breast reconstruction in the obese patient. Plast Reconstr Surg 2001;108:1954-60; discussion 1961-2.
- Kanchwala SK, Bucky LP. Optimizing pedicled transverse rectus abdominis muscle flap breast reconstruction. Cancer J 2008;14:236-40. [PubMed]
- Blondeel N, Vanderstraeten GG, Monstrey SJ, et al. The donor site morbidity of free DIEP flaps and free TRAM flaps for breast reconstruction. Br J Plast Surg 1997;50:322-30. [PubMed]
- Chen CM, Halvorson EG, Disa JJ, et al. Immediate postoperative complications in DIEP versus free/muscle-sparing TRAM flaps. Plast Reconstr Surg 2007;120:1477-82. [PubMed]
- Man LX, Selber JC, Serletti JM. Abdominal wall following free TRAM or DIEP flap reconstruction: a meta-analysis and critical review. Plast Reconstr Surg 2009;124:752-64. [PubMed]
- Atisha D, Alderman AK. A systematic review of abdominal wall function following abdominal flaps for postmastectomy breast reconstruction. Ann Plast Surg 2009;63:222-30. [PubMed]
- Wu LC, Bajaj A, Chang DW, et al. Comparison of donor-site morbidity of SIEA, DIEP, and muscle-sparing TRAM flaps for breast reconstruction. Plast Reconstr Surg 2008;122:702-9. [PubMed]
- Chevray PM. Breast reconstruction with superficial inferior epigastric artery flaps: a prospective comparison with TRAM and DIEP flaps. Plast Reconstr Surg 2004;114:1077-83; discussion 1084-5. [PubMed]
- Khoo A, Kroll SS, Reece GP, et al. A comparison of resource costs of immediate and delayed breast reconstruction. Plast Reconstr Surg 1998;101:964-8; discussion 969-70. [PubMed]
- Neyt MJ, Blondeel PN, Morrison CM, et al. Comparing the cost of delayed and immediate autologous breast reconstruction in Belgium. Br J Plast Surg 2005;58:493-7. [PubMed]
- Chevray PM. Timing of breast reconstruction: immediate versus delayed. Cancer J 2008;14:223-9. [PubMed]
- DeBono R, Thompson A, Stevenson JH. Immediate versus delayed free TRAM breast reconstruction: an analysis of perioperative factors and complications. Br J Plast Surg 2002;55:111-6. [PubMed]
- Albornoz CR, Cordeiro PG, Farias-Eisner G, et al. Diminishing relative contraindications for immediate breast reconstruction. Plast Reconstr Surg 2014;134:363e-9e. [PubMed]
- Kronowitz SJ, Hunt KK, Kuerer HM, et al. Delayed-immediate breast reconstruction. Plast Reconstr Surg 2004;113:1617-28. [PubMed]
- Patel KM, Albino F, Fan KL, et al. Microvascular autologous breast reconstruction in the context of radiation therapy: comparing two reconstructive algorithms. Plast Reconstr Surg 2013;132:251-7. [PubMed]
- Albino FP, Patel KM, Smith JR, et al. Delayed versus Delayed-Immediate Autologous Breast Reconstruction: A Blinded Evaluation of Aesthetic Outcomes. Arch Plast Surg 2014;41:264-70. [PubMed]
- Weichman KE, Broer PN, Tanna N, et al. The role of autologous fat grafting in secondary microsurgical breast reconstruction. Ann Plast Surg 2013;71:24-30. [PubMed]
- Albornoz CR, Cordeiro PG, Hishon L, et al. A nationwide analysis of the relationship between hospital volume and outcome for autologous breast reconstruction. Plast Reconstr Surg 2013;132:192e-200e. [PubMed]


