
Ratio of CA19-9 level to total bilirubin as a novel prognostic indicator in patients with pancreatic head carcinoma following curative resection
Introduction
Pancreatic carcinoma represents one of the most common malignant tumors in the digestive system. Due to the high degree of malignancy of the tumor itself, it is prone to local vascular invasion and distant metastasis, the overall surgical resection rate is less than 20% and the five-year survival rate is less than 10% (1). According to the global cancer statistics in 2018, pancreatic cancer currently ranks 14th in the incidence of malignant tumors but 6th in mortality (2). At present, radical resection is still the best treatment for pancreatic cancer (3), therefore, it is of great significance to correctly judge the long-term prognosis of patients with pancreatic cancer before operation for the formulation of a reasonable and effective treatment plan.
Koprowski et al. (4) obtained a monoclonal antibody numbered 1116NS19-9 from human colon cancer cell lines by cell hybridization in 1979. The antibody could react with a class of tumor-associated carbohydrate antigens, which were also named carbohydrate antigen 19-9. CA19-9 is abnormally increased in patients with malignant tumors such as pancreatic cancer, cholangiocarcinoma and gallbladder cancer, a large number of studies have confirmed that CA19-9 is significantly associated with the diagnosis and prognosis of pancreatic cancer, as well as postoperative recurrence (5,6). However, CA19-9 is not specific to tumor cells and can also be synthesized in normal human pancreas, bile duct, stomach, colon and other epithelial cells (7), therefore, low concentration of CA19-9 can also be detected in normal human blood (8). Nevertheless, when biliary obstruction occurs, CA19-9 secreted by bile duct epithelial cells cannot be excreted into the intestinal tract normally, while CA19-9 secreted by pancreatic epithelial cells may also flow back into the biliary tract, in addition, biliary inflammation caused by obstructive jaundice stimulates bile duct epithelial cell proliferation, which can lead to the increase of CA19-9 in blood (9). Therefore, in some patients with benign biliary obstructive diseases and biliary inflammatory diseases, increased CA19-9 concentration can also be found, leading to decreased sensitivity (10). As for patients with pancreatic head cancer (PHC), some patients have biliary obstruction caused by tumor compression or invasion, in that case, the concentration of CA19-9 will also be affected, resulting in a decline in their predictive ability.
In this study, carbohydrate antigen 19-9 level to total bilirubin (CA19-9/TB) is used to reduce the influence of obstructive jaundice on the concentration of CA19-9, thereby determining the correlation between CA19-9/TB and tumor recurrence or long-term prognosis of patients with PHC.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/gs-20-720).
Methods
Ethics approval and consent to participate:
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee of Beijing Chaoyang Hospital (No.2020-D.-309-3). Participant informed consent was exempted because of the retrospective study design, and the study design was approved by the appropriate ethics review board.
Patient selection
Our study retrospectively analyzed the data of PHC patients who underwent surgical treatment at our institution (Beijing ChaoYang Hospital, Capital Medical University, Beijing, China) between January 2010 and December 2019 and screened out 339 eligible patients for further analysis according to the inclusion and exclusion criteria (Figure 1).
Eligibility criteria: (I) patients with PHC who underwent PD from January 2010 to December 2019; (II) no restriction was imposed on age and gender; (III) underwent en bloc resection during surgery; (IV) histopathological diagnosis of pancreatic ductal adenocarcinoma; (V) the informed consent of the patient and his/her family was obtained.
Exclusion criteria: (I) history of previous anti-cancer therapies and other malignancies; (II) surgical rule violation; (III) unresectable condition or metastasis found during surgery; (IV) data on all clinical and laboratory characteristics and treatments are incomplete, as well as outcomes and follow-up.
Patients’ characteristics
A total of 339 patients with PHC were enrolled, including 192 males and 147 females, male: female = 1.3:1, aged 63.0±10.1 years old. The initial symptoms mainly included abdominal pain (n=146), jaundice (n=134), atypical gastrointestinal symptoms (n=19) and another 40 patients were found during physical examination. Of all the patients, 117 (34.5%) had a history of diabetes. Among the 134 patients with jaundice symptoms, 56 patients received preoperative jaundice reduction treatment, including 19 cases of ERCP and 37 cases of PTBD.
Patients grouping and definition
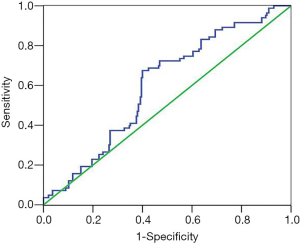
The ROC curve was drawn based on the ratio of CA19-9/TB and the 1-year survival of the patients (Figure 2), from which the optimal cut-off value of CA19-9/TB was determined to be 7.7 [area under curve (AUC), 0.599, 95% CI: 0.533–0.666], at this time, the sensitivity of predicting 1-year survival is 67.5%, and the specificity is 60.0%, and the patients were divided into low-ratio group (Group 1, n=182) and high-ratio group (Group 2, n=157) according to the best cut-off value. The results of CA19-9 and TB test were taken from the patient’s last blood sample before operation, and for the patients treated with reducing jaundice, our center will recheck CA19-9 and TB the day before operation.
Follow-up strategy
Postoperative follow-up was performed by the combination of outpatient reexamination and telephone follow-up. all patients were followed up 1 and 3 months after PD, once every three months for the first 2 years and thereafter every six months interval or until tumor recurrence or death. For the all follow-up visits, blood examination was routinely taken, liver function tests and serum tumor markers including CA19-9, and an abdominal ultrasound was performed. Contrast-enhanced CT or MRI was performed once every six months or earlier if tumor recurrence or metastasis was suspected. Further investigation was carried out when clinically indicated, such as positron emission tomography CT (PET-CT). OS was defined as from the dates of surgery to the dates of death or the dates of last follow-up. DFS was calculated from the dates of operation to the dates of last follow-up (for the patients without recurrence) or from the interval between the dates of surgery and the first recurrence.
Statistical analysis
The measurement data are expressed by mean ± standard deviation in accordance with normal distribution and by median (quartile spacing) in non-normal distribution. According to the comparison of the measurement data between the two groups, the t-test was used for the normal distribution and the rank sum test was used for the non-normal distribution. Chi-square test was used to compare the counting data between the two groups. If the theoretical frequency was less than 1, the Fisher exact probability method was used. The survival curve was calculated by Kaplan-Meier method, and the difference of survival rate between the two groups was compared by Log-rank test. All data were analyzed by SPSS22.0 software.
Results
Perioperative condition
All patients successfully completed the operation and removed the tumor, among them, 122 cases were accompanied with portal vein invasion, 12 cases underwent direct suture after wedge resection of the invaded vessels, 85 cases underwent allogeneic vascular replacement and 25 cases underwent end-to-end anastomosis after resection of the invaded vessels. Blood transfusion was performed in 120 patients (35.4%) and intraoperative blood loss of 500 (400, 800) mL, the operation time was 9.9±2.9 hours.
Postpathological examination confirmed that all patients were pancreatic ductal adenocarcinoma, including 23 cases (6.8%) of highly differentiated tumors, 229 cases (67.6%) of moderately differentiated tumors and 87 cases (25.7%) of poorly differentiated tumors. The size of tumor was 3.8±1.7 cm, and 222 patients (65.5%) with positive lymph nodes. Radical resection (R0) was achieved in 314 cases (92.6%), apart from them, pancreatic cutting margin appeared positive in 9 cases, pancreatic circumferential edge revealed positive in 9 cases, pancreatic uncinate process margin represented positive in 4 cases, and portal sulcus margin showed positive in 3 cases.
Postoperative complications
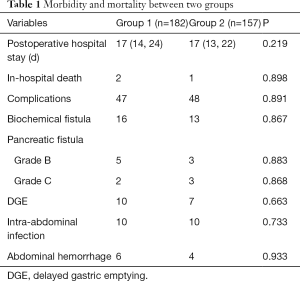
As for the postoperative morbidity, which appeared in 95 cases, with a occurrence rate of 28.0%. Including 29 (8.6%) cases of biochemical fistula, 8 (2.4%) cases of level B pancreatic fistula, 5 (1.5%) cases of level C pancreatic fistula, abdominal infection in 20 cases (5.9%), DGE (disturbance of gastric emptying) in 17 cases (5.0%), 10 (2.9%) cases of abdominal hemorrhage and so on. As we summarize in Table 1.
Full table
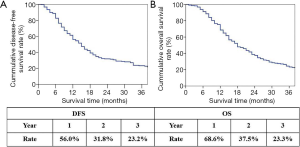
Survival data and recurrence
Our follow-up finished in June 2020 and the medium follow-up period was 51 months, during which 191(56.3%) of all the included patients received postoperative adjuvant chemotherapy for 1 to 8 cycle. The overall median DFS (disease-free survival) time and the median overall survival (OS) time were shown in Figure 3A and Figure 3B respectively.
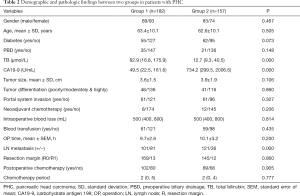
Comparison of perioperative and long-term prognostic data in different groups
The comparison of perioperative general data between Group 1 and Group 2 was shown in Table 2, which can be seen that Group 1 had lower CA19-9, higher TB and lymph node metastasis rate (P<0.05). The postoperative complications between Group 1 and Group 2 were compared and shown in Table 3. from which we can find that there was no significant difference in postoperative mortality and incidence of morbidity between the two groups (P>0.05).
Full table
Full table
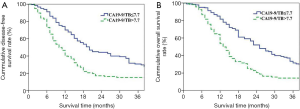
The median DFS of patients in Group 1 and Group 2 was 20 and 10 months, respectively, and the 1year, 2year and 3-year DFS rates were 70.1%, 44.3%, 30.8% and 39.9%, 17.1%, 13.6%, respectively (P=0.000, Figure 4A). The median OS of patients in Group 1 and Group 2 was 25 months and 13 months, respectively, and the 1year, 2year and 3year OS rates were 81.5%, 52.1%, 31.5% and 53.7%, 20.5%, 14.2%, respectively (P=0.000, Figure 4B).
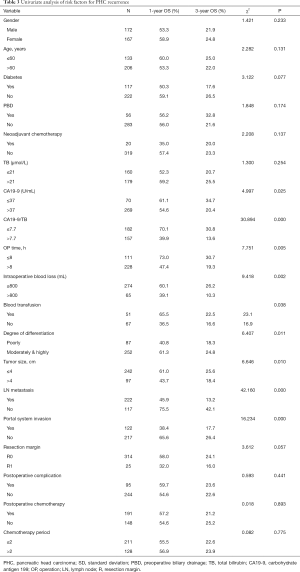
Analysis of risk factors influencing postoperative tumor recurrence in patients with PHC
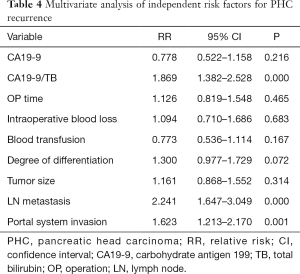
Postoperative tumor recurrence in patients with PHC was taken as a dependent variable and preoperative data, intraoperative data, pathological data and postoperative data of patients as an independent variable for univariate analysis (Table 3). Univariate analysis showed that CA19-9, CA19-9/TB, operation time, blood loss, blood transfusion, degree of tumor differentiation, tumor size, lymph node metastasis, and portal system invasion might be the risk factors for tumor recurrence in patients with PHC, and multivariate analysis showed that CA19-9/TB (RR =1.869, 95% CI: 1.382–2.528), portal system invasion (RR =1.623, 95% CI: 1.213–2.170) and lymph node metastasis (RR =2.241, 95% CI: 1.647–3.049) were independent risk factors for postoperative tumor recurrence in patients with PHC (Table 4).
Full table
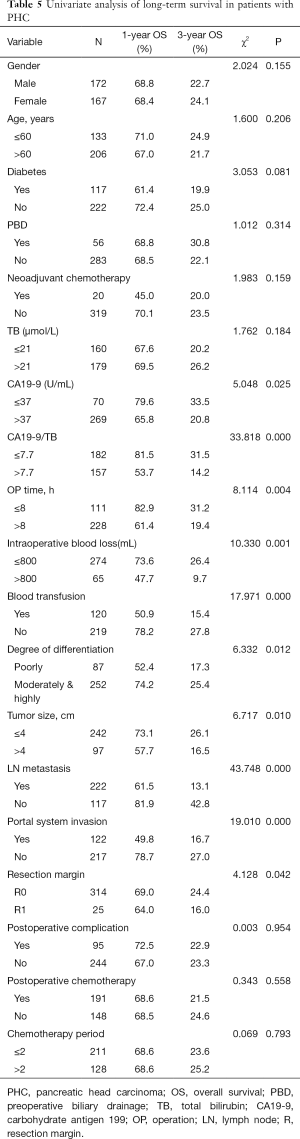
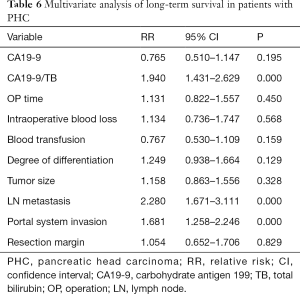
Analysis of risk factors influencing postoperative long-term survival in patients with PHC
Postoperative long-term survival in patients with PHC was taken as a dependent variable and preoperative data, intraoperative data, pathological data and postoperative data of patients as an independent variable for univariate analysis (Table 5). Univariate analysis showed that CA19-9, CA19-9/TB, operation time, blood loss, blood transfusion, degree of tumor differentiation, tumor size, lymph node metastasis, portal system invasion and resection edge might be the risk factors affecting long-term survival after operation, and multivariate analysis showed that CA19-9/TB (RR =1.869, 95% CI: 1.382–2.528), portal system invasion (RR =1.623, 95% CI: 1.213–2.170) and lymph node metastasis (RR =2.241, 95% CI: 1.647–3.049) were independent risk factors for long-term survival in patients with PHC (Table 6).
Full table
Full table
Discussion
The poor long-term prognosis of PHC is mainly due to the early recurrence after tumor resection, some studies (11,12) have asserted that tumor size, degree of differentiation, lymph node metastasis and other indicators are closely related to postoperative recurrence and long-term prognosis of PHC. However, compared with these postoperative clinicopathological results, clinical indicators that can be obtained immediately before surgery are more needed to judge the long-term prognosis of patients, so as to formulate a more reasonable treatment plan.
At present, CA19-9 is still an important serological marker for clinical diagnosis and prognosis of pancreatic cancer (13). O’Brien et al. (14). showed that at 95% specificity, CA19-9 (>37 U/mL) had a sensitivity of 68% up to 1 year, and 53% up to 2 years before diagnosis. Therefore, it is considered that CA19-9 can be used in the early diagnosis of pancreatic cancer. Sugiura et al. (15) reviewed the data of 154 patients with PD and found that preoperative CA19-9 was an independent risk factor for long-term prognosis in patients with pancreatic cancer, and the median survival time of patients in the low-level group was significantly better than those in the high-level group (31 vs. 16 months). Boeck et al. (6) through a systematic review of the literature, it is concluded that CA19-9 is an important serological marker for judging the prognosis and monitoring of patients with pancreatic cancer, and its decreasing level can also reflect the effect of treatment to some extent.
Meanwhile, some scholars have pointed out that the sensitivity of CA19-9 in the diagnosis of pancreatic cancer is more than 80%, but for patients with jaundice symptoms, the accuracy of judging benign or malignant diseases is significantly reduced. Mann et al. (16) reviewed 164 patients with abnormally elevated levels of CA19-9, and found that for patients with jaundice, the sensitivity of CA19-9 in the diagnosis of malignant tumors was only 48.4%, and the level of CA19-9 was positively correlated with the level of bilirubin. Patients with PHC will gradually oppress or invade the bile duct and cause obstructive jaundice with the enlargement of the tumor due to the special location of the tumor, resulting in a mismatched increase in the concentration of CA19-9. In our study, the proportion of patients with CA19-9 >37 U/mL was as high as 79.4%, and the prognosis was significantly worse than that of patients with CA19-9 ≤37 U/mL (P=0.025). However, CA19-9 was not an independent risk factor for prognosis after multivariate analysis, we consider that this is mainly related to the relatively large number of patients (52.8%) with TB >21 mol/L. The overall concentration of CA19-9 is slightly higher due to bile excretion disorder, so it does not really reflect the prognosis of patients.
Ong et al. (17) analyzed 83 patients who were misdiagnosed as malignant tumor with the increase of CA19-9 index, and found that the increase of bilirubin was an independent risk factor leading to the increase of CA19-9 index (P=0.028). It is suggested that CA19-9 should be adjusted according to the index of bilirubin, but no feasible adjustment scheme is given. Studies such as Kang (18) have shown that the ratio of CA19-9 to total bilirubin can be used to predict the recurrence of resectable pancreatic cancer, but the enrolled patients also included 24.6% of patients suffered from pancreatic body and tail cancer with no jaundice symptoms, so the homogeneity of the study is poor. La Greca (19) and other studies have shown that the ratio of CA19-9 to total bilirubin can be used to distinguish between benign and malignant causes of obstructive jaundice, which can improve the specificity of diagnosis. However, the malignant tumor patients enrolled in that study included pancreatic cancer, cholangiocarcinoma, gallbladder cancer, ampullary cancer and so on as well, so the value of the study is limited. Bolm et al. (20) asserted that CA19-9 can be corrected by the ratio of CA19-9 to bilirubin, and the adjusted CA19-9/TB was more realistic for the relative level of CA19-9 in patients with distal cholangiocarcinoma, thus improving the sensitivity of CA19-9 in judging the long-term prognosis of patients with distal cholangiocarcinoma. Our results confirm that CA19-9/TB is an independent risk factor for postoperative tumor recurrence and long-term survival of PHC. The lower the CA19-9/TB, the better the long-term prognosis of patients.
On the other hand, our study also shows that CA19-9/TB is correlated with lymph node metastasis to some extent. The lower CA19-9/TB is, the higher lymph node metastasis rate is. However, CA19-9/TB was not correlated with tumor size or vascular invasion. Meanwhile, lymph node metastasis has also been proved to be an independent risk factor for long-term survival of patients with PHC. We assume that CA19-9/TB, like lymph node metastasis, reflects the aggressiveness and metastasis of tumor to a certain extent, but is not associated with local tumor enlargement or direct invasion.
In addition, we insist that portal vein invasion is an independent risk factor for long-term prognosis of PHC as well, which is consistent with most international studies at present (21-23). Ramacciato et al. (24) reviewed the data of 406 patients undergoing pancreatic cancer surgery in 8 pancreatic centers in Italy. Multivariate analysis confirmed that portal vein invasion was an independent risk factor for poor prognosis. The median survival time and 5-year survival rate in the non-vascular invasion group were significantly better than those in the vascular invasion group (33 vs. 20 months; 31.7% vs. 15.5%). We highly suspect that this is mainly related to the higher incidence of hematogenous metastasis after tumor invasion of portal system.
The deficiencies of this study are as follows: on the one hand, it is a single-center retrospective study, on the other hand, it is not clear how the proportion of CA19-9 and bilirubin increases, nor can it confirm whether CA19-9 will decrease in proportion to bilirubin after relief of biliary obstruction. However, as far as the current research is concerned, CA19-9/TB is better than CA19-9 in predicting postoperative tumor recurrence and long-term survival of PHC. Although our results showed that the CA19-9/TB ratio plays an independently role in predicting the long-term prognosis of patients with PHC, on the one hand, it needs to be verified by a large sample of data. On the other hand, the prognosis of patients with PHC is also related to the biological characteristics of the tumor, the degree of invasion, the choice of treatment and so on. Therefore, the ratio can be used as a reference before treatment selection, however, it can not be used alone to determine the choice of treatment. Perhaps in the near future, a more reasonable proportion relationship can be calculated by the mathematical model for the correction of CA19-9, which can be used to guide the determination of treatment plan for patients with PHC and the detection of tumor recurrence after operation.
Conclusions
To sum up, compared with CA19-9 alone, CA19-9/TB is more valuable in judging postoperative tumor recurrence and long-term survival of PHC. The lower the ratio, the better the long-term prognosis.
Acknowledgments
Funding: This study was supported by Beijing Municipal Science & Technology Commission, China (Grant No. Z181100001718164) and Capital’s Funds for Health Improvement and Research, Beijing, China (CFH 2020-2-2036).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/gs-20-720
Data Sharing Statement: Available at http://dx.doi.org/10.21037/gs-20-720
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/gs-20-720). The authors have no conflicts of interest to declare
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee of Beijing Chaoyang Hospital (No.2020-D.-309-3). Participant informed consent was exempted because of the retrospective study design.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 2018;68:7-30. [Crossref] [PubMed]
- Zhu H, Li T, Du Y, et al. Pancreatic cancer: challenges and opportunities. BMC Med 2018;16:214. [Crossref] [PubMed]
- Koprowski H, Steplewski Z, Mitchell K, et al. Colorectal carcinoma antigens detected by hybridoma antibodies. Somatic Cell Genet 1979;5:957-71. [Crossref] [PubMed]
- Bergquist JR, Puig CA, Shubert CR, et al. Carbohydrate Antigen 19-9 Elevation in Anatomically Resectable, Early Stage Pancreatic Cancer Is Independently Associated with Decreased Overall Survival and an Indication for Neoadjuvant Therapy: A National Cancer Database Study. J Am Coll Surg 2016;223:52-65. [Crossref] [PubMed]
- Boeck S, Stieber P, Holdenrieder S, et al. Prognostic and therapeutic significance of carbohydrate antigen 19-9 as tumor marker in patients with pancreatic cancer. Oncology 2006;70:255-64. [Crossref] [PubMed]
- Lee SP, Sung IK, Kim JH, et al. Usefulness of Carbohydrate Antigen 19-9 Test in Healthy People and Necessity of Medical Follow-up in Individuals with Elevated Carbohydrate Antigen 19-9 Level. Korean J Fam Med 2019;40:314-22. [Crossref] [PubMed]
- Zhang GM, Bai SM, Zhang GM, et al. Reference intervals of carbohydrate antigen 19-9 in the apparently healthy adult population. J Clin Lab Anal 2018;32:e22380 [Crossref] [PubMed]
- Lin MS, Huang JX, Yu H. Elevated serum level of carbohydrate antigen 19-9 in benign biliary stricture diseases can reduce its value as a tumor marker. Int J Clin Exp Med 2014;7:744-50. [PubMed]
- Marrelli D, Caruso S, Pedrazzani C, et al. CA19-9 serum levels in obstructive jaundice: clinical value in benign and malignant conditions. Am J Surg 2009;198:333-9. [Crossref] [PubMed]
- Hlavsa J, Cecka F, Zaruba P, et al. Tumor grade as significant prognostic factor in pancreatic cancer: validation of a novel TNMG staging system. Neoplasma 2018;65:637-43. [Crossref] [PubMed]
- Barugola G, Partelli S, Crippa S, et al. Time trends in the treatment and prognosis of resectable pancreatic cancer in a large tertiary referral centre. HPB (Oxford) 2013;15:958-64. [Crossref] [PubMed]
- Le N, Sund M, Vinci A. GEMS collaborating group of Pancreas 2000. Prognostic and predictive markers in pancreatic adenocarcinoma. Dig Liver Dis 2016;48:223-30. [Crossref] [PubMed]
- O'Brien DP, Sandanayake NS, Jenkinson C, et al. Serum CA19-9 is significantly upregulated up to 2 years before diagnosis with pancreatic cancer: implications for early disease detection. Clin Cancer Res 2015;21:622-31. [Crossref] [PubMed]
- Sugiura T, Uesaka K, Kanemoto H, et al. Serum CA19-9 is a significant predictor among preoperative parameters for early recurrence after resection of pancreatic adenocarcinoma. J Gastrointest Surg 2012;16:977-85. [Crossref] [PubMed]
- Mann DV, Edwards R, Ho S, et al. Elevated tumour marker CA19-9: clinical interpretation and influence of obstructive jaundice. Eur J Surg Oncol 2000;26:474-9. [Crossref] [PubMed]
- Ong SL, Sachdeva A, Garcea G, et al. Elevation of carbohydrate antigen 19-9 in benign hepatobiliary conditions and its correlation with serum bilirubin concentration. Dig Dis Sci 2008;53:3213-7. [Crossref] [PubMed]
- Kang CM, Kim JY, Choi GH, et al. The use of adjusted preoperative CA19-9 to predict the recurrence of resectable pancreatic cancer. J Surg Res 2007;140:31-5. [Crossref] [PubMed]
- La Greca G, Sofia M, Lombardo R, et al. Adjusting CA19-9 values to predict malignancy in obstructive jaundice: influence of bilirubin and C-reactive protein. World J Gastroenterol 2012;18:4150-5. [Crossref] [PubMed]
- Bolm L, Petrova E, Weitz J, et al. Prognostic relevance of preoperative bilirubin-adjusted serum carbohydrate antigen 19-9 in a multicenter subset analysis of 179 patients with distal cholangiocarcinoma. HPB (Oxford) 2019;21:1513-9. [Crossref] [PubMed]
- Imamura T, Yamamoto Y, Sugiura T, et al. Prognostic role of the length of tumour-vein contact at the portal-superior mesenteric vein in patients having surgery for pancreatic cancer. Br J Surg 2019;106:1649-56. [Crossref] [PubMed]
- Morimoto D, Yamada S, Murotani K, et al. Prognostic Impact of Portal System Invasion in Pancreatic Cancer Based on Image Classification. Pancreas 2018;47:1350-6. [Crossref] [PubMed]
- Hirono S, Kawai M, Okada K, et al. Pancreatic neck cancer has specific and oncologic characteristics regarding portal vein invasion and lymph node metastasis. Surgery 2016;159:426-40. [Crossref] [PubMed]
- Ramacciato G, Nigri G, Petrucciani N, et al. Pancreatectomy with Mesenteric and Portal Vein Resection for Borderline Resectable Pancreatic Cancer: Multicenter Study of 406 Patients. Ann Surg Oncol 2016;23:2028-37. [Crossref] [PubMed]



