Prediction of ipsilateral and contralateral central lymph node metastasis in unilateral papillary thyroid carcinoma: a retrospective study
Introduction
Papillary thyroid carcinoma (PTC) is the most common histologic type of differentiated thyroid cancer, which is characterized by early lymph node (LN) metastasis (1). Cervical LN metastasis is frequently observed in PTC patients with an average incidence of 60% (2). The most common sites of metastases are the central lymph nodes (CLNs) of the neck (level VI), followed by ipsilateral lateral LNs (3). Therapeutic central compartment neck dissection is well accepted to perform for patients with known LN metastasis diagnosed by physical examination or preoperative ultrasonograph (US) scanning. However, even for clinically node-negative neck PTC, occult CLN metastasis was found common in postoperatively pathological examination (4-6). It has been known that LN metastasis increases the rate of loco-regional recurrence and mortality of PTC patients. Therefore, the 2009 guidelines of American Thyroid Association (ATA) recommended that prophylactic central lymph node dissection (CLND) may be considered in patients with high-risk thyroid cancer (T3 or T4 classification) (7). However, prophylactic CLND in PTC cases with clinically node-negative neck remains controversial as the lack of convincing evidence of its survival benefits. In addition, recent studies, including a prospective randomized controlled study, showed that the morbidity rate of complications such as hypoparathyroidism or recurrent laryngeal nerve injury was significantly higher in the PTC patients who underwent CLND (8-11). Therefore, the identification of predictive factors of CLN metastasis can help surgeons manage individualized therapy, which is crucial to avoid unnecessary CLND and to minimize postoperative complications. However, predictive factors for CLN metastasis in unilateral PTC cases are not well defined.
The aims of this study were to evaluate the rate of LN metastasis to the ipsilateral and contralateral central neck compartment as well as to determine the predictive factors of ipsilateral and contralateral CLN metastasis in unilateral PTC.
Materials and methods
Study design
We conducted a retrospective study of unilateral PTC patients who underwent total thyroidectomy and bilateral CLND in West China Hospital, Sichuan University from September 2011 to October 2013. All patients were diagnosed with PTC by preoperative fine-needle aspiration biopsy or by intraoperatively on frozen section. Preoperative US and computerized tomography (CT) scan were performed to identify patients with unilateral PTC and no suspicious LN in the neck. No patient previously underwent any cervical surgery, external radiotherapy, or radioactive iodine treatment. Patients with other types of thyroid malignancy or undergoing unilateral CLND were excluded. Patients were also excluded if they had PTC in isthmus (N=9) or bilateral lobes (N=52). A total of 218 patients were finally enrolled into our study. Bilateral CLND is defined as the removal of CLNs [including pretracheal, paratracheal (ipsilateral and contralateral), prelaryngeal and perithyroidal groups] as well as nodes along the recurrent laryngeal nerves (10,12). Dissections were carried out in accordance to anatomical parameters established by the ATA (7). Specimens were separated and marked according to location within the central compartment and sent for histopathologic examination. The electronic clinical and pathological records collected included sex, age, tumor size, perithyroidal invasion, chronic lymphatic thyroiditis and central compartment LN involvement. Moreover, the number of total and positive LNs in each central region was also determined. This study was approved by the Institutional Review Board of Sichuan University, China, and all patients provided informed consents.
All patients were preoperatively examined by the fiberoptic laryngoscopy to evaluate the mobility of vocal cord and reevaluated after surgery. Vocal cord palsy as confirmed by laryngoscopy was considered permanent if it lasted for more than 6 months. While temporary recurrent laryngeal nerve injury was defined as vocal cord palsy persisting for less than 6 months. Postoperative hypoparathyroidism was also evaluated. Patients who developed hypocalcemia were administered oral calcium and vitamin D supplements, and those who developed significant symptoms were administered intravenous calcium gluconate. Temporary hypoparathyroidism was defined as the level of parathyroid hormone <1.60 pmol/L postoperatively. Permanent hypoparathyroidism was defined as the level of parathyroid hormone <1.60 pmol/L persisting more than 6 months after surgery.
Statistical analysis
Statistical analysis was performed using SPSS version 19.0 software. Univariate analysis (Pearson χ2 test or Fisher exact test) and multivariate analysis were used to evaluate relationships between CLN metastasis and demographic factors such as age, sex and the clinicopathologic factors. A P value <0.05 was considered to be statistically significant.
Results
Patient characteristics and pathology
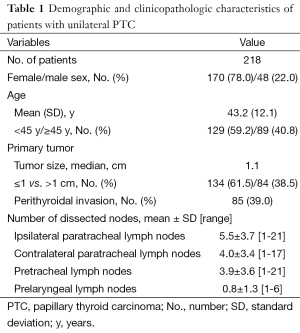
In our study, 170 women (78.0%) and 48 men (22.0%) were enrolled, and the mean age was 43.2±12.1 years, with a range of 10-78 years. Of these patients, 59.2% (129/218) were <45 years of age, and 40.8% (89/218) were ≥45 years of age. The median size of primary tumor was 1.1 cm (range, 0.1-4.0 cm), 134 patients (61.5%) had a primary tumor ≤1 cm, and 84 (38.5%) had a primary tumor >1 cm.
Among 218 patients, 104 patients (47.7%) had ipsilateral CLN metastasis, 29 (13.3%) had bilateral CLN metastasis, 31 (14.2%) had prelaryngeal LN metastasis, and 100 (45.9%) had pretracheal LN metastasis. The mean ± SD numbers of total and positive LNs collected during CLND were 5.5±3.7 (range, 1-21) and 1.3±2.2 (range, 0-8) in the ipsilateral paratracheal region, 4.0±3.4 (range, 1-17) and 0.3±0.8 (range, 0-6) in the contralateral paratracheal region, 0.8±1.3 (range, 1-6) and 0.2±0.6 (range, 0-3) in the prelaryngeal region, and 3.9±3.6 (range, 1-21) and 1.1±2.0 (range, 0-20) in the pretracheal region, respectively (Table 1).
Full table
Univariate and multivariate analyses of risk factors
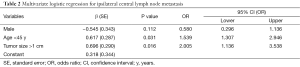
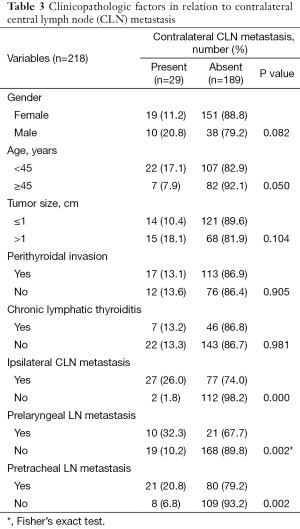
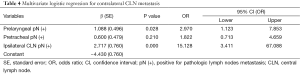
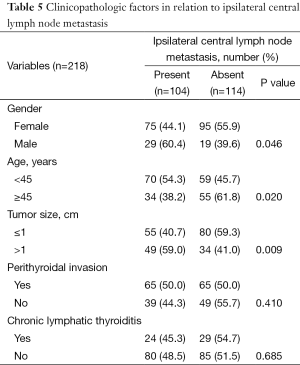
In univariate analysis, ipsilateral CLN metastasis was more prevalent in patients who were male, <45 years of age, or had a tumor >1 cm (P<0.05). Multivariate analysis revealed that tumor size >1 cm (P=0.016; OR, 2.005) and age <45 years old (P=0.031; OR, 1.539) were the predictive factors of ipsilateral CLN metastasis (Table 2). The rate of contralateral CLN metastasis was 13.3%. Contralateral CLN metastasis was significantly associated with prelaryngeal LN metastasis (P=0.002), pretracheal LN metastasis (P=0.002), and ipsilateral CLN metastasis (P<0.001) by univariate analysis (Table 3). Table 4 shows the results of multivariate analysis. Prelaryngeal LN metastasis (P=0.028; OR, 2.970) and ipsilateral CLN metastasis (P<0.001; OR, 15.128) were the independent predictive factors of contralateral CLN metastasis. Perithyroidal invasion and chronic lymphatic thyroiditis were not significantly related to the presence ipsilateral or contralateral CLN metastasis (Tables 3,5).
Full table
Full table
Full table
Full table
Postoperative complications
Eighty-nine of the 218 patients (40.8%) developed transient hypocalcemia requiring calcium supplementation. Of these patients, 2 (0.9%) had permanent hypoparathyroidism. Vocal cord palsy was observed in eight patients. Two patients underwent intentional unilateral recurrent laryngeal nerve resection due to direct tumor invasion. The remaining six patients recovered from hoarseness and showed normal cord mobility within 6 months after surgery.
Discussion
This retrospective study systematically examined the pattern of CLN metastasis in 218 patients with diagnosed with unilateral cN0 PTC. The presence of metastatic LNs at all specific subsites of the central compartment was accurately assessed by standard histologic examination of dissected neck specimens. We found that the rate of occult CLN metastasis was high, 64.7%, in patients with unilateral cN0 PTC and ipsilateral CLN metastasis was the most frequent involved region in central neck compartment. The pattern of CLN metastasis from PTC was similar to those observed in previous studies (5,6).
The incidence of occult nodal metastasis of PTC in central compartment has been reported to vary between 30% and 90% (2). Eun et al. (6) reported that the rate of CLN metastasis is 36.4% in PTC cases with clinically node-negative neck. Another report showed that CLN metastasis associated with PTC is present in 52.3% (79/151) of cases (5). These results including ours indicate that LNs in the central compartment generally are most commonly involved in metastasis, and it is necessary to perform routine CLND in primary surgery. However, to date, prophylactic CLND in clinically node-negative PTC patients are still a matter of debate. Some authors recommend routine CLND to prevent long-term recurrence and decrease postoperative thyroglobulin (Tg) levels, citing the high risk of cervical LN metastasis in PTC (13-15). Furthermore, several prospective studies have demonstrated that prophylactic CLND is able to improve accuracy in staging and selecting patients for Radioiodine (RAI) and with a lower risk complication when compared to that with reoperative surgery (14,16,17). While others suggest that this procedure increases the risk of postoperative complications, such as hypothyroidism or the recurrent laryngeal nerves injury, without any demonstrable long-term survival benefits (9,18,19).
High percentage of occult CLN metastasis was also reported in papillary thyroid microcarcinoma (PTMC) in previous studies (20,21) and it is widely accepted that tumor size is closely related with CLN metastasis. Previous studies have reported that tumor size of greater than 1 cm was associated with a higher rate of ipsilateral CLN metastasis, and our result was consistent with the results (5,22). Although some LN metastasis may be treated with radioactive iodine, the addition of nodal dissection could reduce the need for reoperation in the central compartment and with lower postoperative Tg levels (23). LN metastasis in PTC may associate with various factors such as gender, primary tumor size, capsular invasion, extracapsular extension, multifocality, and BRAF-mutated gene expression (1,4,6,22). On multivariate analysis in our study, tumor size >1 cm was an independent predictive factor of ipsilateral CLN metastasis in cases of PTC, which was similar to previous studies (4,6,22). These results including ours indicate that the rate of ipsilateral CLN metastasis is significantly higher in cases of tumor with a maximal diameter of greater than 1 cm, and prophylactic ipsilateral CLND with thyroidectomy should be considered as an option when managing these patients. Although several studies (4,6) found no correlation between age and ipsilateral CLN metastasis, Lee et al. (5) found a higher prevalence of ipsilateral CLN metastasis in patients with age <45 years old. Similarly, our study also showed that age <45 years old was the predictive factor of ipsilateral CLN metastasis.
Tumor with perithyroidal invasion has been repeated demonstrated closely related to increased rates of central compartmental LN metastases in PTC, which was also independent predictor of both pathological and clinical outcomes. However, Eun et al. (6) have found no correlation between perithyroidal invasion and CLN metastasis in a prospective multicenter study of 140 patients. Perithyroidal invasion was also not significantly associated with CLN metastasis in our study. The different result we observed may have been due to the rate of perithyroidal invasion in our study was lower than previous studies (45.8-54.3%) (22,24).
The rate of contralateral CLN metastasis was 13.3% (29/218). Of these patients, 2 (6.90%) had isolated contralateral CLN metastasis without ipsilateral CLN involvement in our study. Multivariate analysis in our study showed that ipsilateral CLN metastasis was an independent predictor of contralateral CLN metastasis, which was consistent with previous reports (5,22,25). Additionally, we also found the rate of contralateral CLN metastasis was significantly higher in cases with histologically proven metastasis to the prelaryngeal LN (P=0.028). It is accepted that prelaryngeal LN positivity was associated with further nodal metastasis to the central and lateral neck compartments and with heavier nodal burden (26-29). As our study reported, the incidence of ipsilateral CLN metastasis was high, while that of contralateral CLN metastasis was relatively low, with most metastases observed in patients with tumors size >1 cm. This may guide the extent of prophylactic CLND in the management of patients with unilateral PTC. Although the ATA guidelines do not recommend elective central neck dissection in patients with small, noninvasive cN0 PTCs or in most patients with follicular cancer, our findings indicate that patients with larger tumor size (>1 cm) should undergo unilateral or bilateral CLND with thyroidectomy in the initial surgery and for most patients with tumor size >1 cm, total thyroidectomy and ipsilateral CLND should be sufficient (7).
Hypocalcemia was more commonly seen in PTC patients with thyroidectomy and CLND than with thyroidectomy alone. In our study, transient hypoparathyroidism was found in 40.8% (89/218), which was similar to those observed in previous studies (26.6-49.5%) (6,24,30). Considering the mentioned morbidities in preceding paragraphs, preoperative identification of patients with PTC at greater risk of metastases to the central compartment would be valuable. Sometimes LN metastasis in the central compartment cannot be detected by palpation and does not appear abnormal in preoperative imaging. Preoperative US have been reported as a rapid, low-cost, noninvasive, and reliable method for detecting neck metastasis of head and neck cancer, but with a limitation because of low sensitivity (31-33). To evaluate the status of CLN metastasis accurately, intraoperative palpation or inspection has emerged as an alternative approach to preoperative imaging. Intraoperative frozen biopsy appears to be a supplementary, safe and efficacious tool to guide the use and determine the extent of CLND (15,34). Based on the results of this study, therapeutic bilateral CLND may be considered in patients with a tumor size >1 cm and especially, if there exists prelaryngeal LN and ipsilateral CLN metastasis on frozen section analysis.
Our findings indicate that CLN metastasis is common in PTC patients with clinically node negative neck and prophylactic ipsilateral CLND may be an optional procedure and should be considered for patients with a tumor size >1 cm. However, we cannot determine the cause-and-effect relationship between the risk and variables due to our study was conducted with a retrospective design. Furthermore, owing to the short duration of follow-up, tumor recurrence and survival after central compartment dissection were not well studied. Further investigation with a long follow-up time is necessary to determine whether the studied parameters are associated with prognosis.
Conclusions
The most common pattern of CLN metastasis in unilateral PTC patients with clinically node-negative neck was ipsilateral CLN metastasis. Tumor size >1 cm was an independent predictive factor of ipsilateral CLN metastasis and prelaryngeal LN metastasis and ipsilateral CLN metastasis were the independent predictive factors of contralateral CLN metastasis. Prophylactic ipsilateral CLND may be an optional procedure and should be considered for patients with a tumor size >1 cm. Therapeutic bilateral CLND should be considered in patients with a tumor size >1 cm and especially, if there exists prelaryngeal LN or ipsilateral CLN metastasis on frozen section analysis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Nam IC, Park JO, Joo YH, et al. Pattern and predictive factors of regional lymph node metastasis in papillary thyroid carcinoma: a prospective study. Head Neck 2013;35:40-5. [PubMed]
- Rotstein L. The role of lymphadenectomy in the management of papillary carcinoma of the thyroid. J Surg Oncol 2009;99:186-8. [PubMed]
- Machens A, Hinze R, Thomusch O, et al. Pattern of nodal metastasis for primary and reoperative thyroid cancer. World J Surg 2002;26:22-8. [PubMed]
- Joo JY, Park JY, Yoon YH, et al. Prediction of occult central lymph node metastasis in papillary thyroid carcinoma by preoperative BRAF analysis using fine-needle aspiration biopsy: a prospective study. J Clin Endocrinol Metab 2012;97:3996-4003. [PubMed]
- Lee KE, Chung IY, Kang E, et al. Ipsilateral and contralateral central lymph node metastasis in papillary thyroid cancer: patterns and predictive factors of nodal metastasis. Head Neck 2013;35:672-6. [PubMed]
- Eun YG, Lee YC, Kwon KH. Predictive factors of contralateral paratracheal lymph node metastasis in papillary thyroid cancer: prospective multicenter study. Otolaryngol Head Neck Surg 2014;150:210-5. [PubMed]
- American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer, Cooper DS, Doherty GM, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009;19:1167-214. [PubMed]
- Conzo G, Calò PG, Sinisi AA, et al. Impact of prophylactic central compartment neck dissection on locoregional recurrence of differentiated thyroid cancer in clinically node-negative patients: a retrospective study of a large clinical series. Surgery 2014;155:998-1005. [PubMed]
- Palestini N, Borasi A, Cestino L, et al. Is central neck dissection a safe procedure in the treatment of papillary thyroid cancer? Our experience. Langenbecks Arch Surg 2008;393:693-8. [PubMed]
- White ML, Gauger PG, Doherty GM. Central lymph node dissection in differentiated thyroid cancer. World J Surg 2007;31:895-904. [PubMed]
- Viola D, Materazzi G, Valerio L, et al. Prophylactic central compartment lymph node dissection in papillary thyroid carcinoma: clinical implications derived from the first prospective randomized controlled single institution study. J Clin Endocrinol Metab 2015;100:1316-24. [PubMed]
- American Thyroid Association Surgery Working Group, American Association of Endocrine Surgeons, American Academy of Otolaryngology-Head and Neck Surgery, et al. Consensus statement on the terminology and classification of central neck dissection for thyroid cancer. Thyroid 2009;19:1153-8. [PubMed]
- Nixon IJ, Ganly I, Patel SG, et al. Observation of clinically negative central compartment lymph nodes in papillary thyroid carcinoma. Surgery 2013;154:1166-72; discussion 1172-3. [PubMed]
- Raffaelli M, De Crea C, Sessa L, et al. Prospective evaluation of total thyroidectomy versus ipsilateral versus bilateral central neck dissection in patients with clinically node-negative papillary thyroid carcinoma. Surgery 2012;152:957-64. [PubMed]
- Sadowski BM, Snyder SK, Lairmore TC. Routine bilateral central lymph node clearance for papillary thyroid cancer. Surgery 2009;146:696-703; discussion 703-5. [PubMed]
- Raffaelli M, De Crea C, Sessa L, et al. Can intraoperative frozen section influence the extension of central neck dissection in cN0 papillary thyroid carcinoma? Langenbecks Arch Surg 2013;398:383-8. [PubMed]
- Carling T, Long WD 3rd, Udelsman R. Controversy surrounding the role for routine central lymph node dissection for differentiated thyroid cancer. Curr Opin Oncol 2010;22:30-4. [PubMed]
- Giordano D, Valcavi R, Thompson GB, et al. Complications of central neck dissection in patients with papillary thyroid carcinoma: results of a study on 1087 patients and review of the literature. Thyroid 2012;22:911-7. [PubMed]
- Chisholm EJ, Kulinskaya E, Tolley NS. Systematic review and meta-analysis of the adverse effects of thyroidectomy combined with central neck dissection as compared with thyroidectomy alone. Laryngoscope 2009;119:1135-9. [PubMed]
- Park JP, Roh JL, Lee JH, et al. Risk factors for central neck lymph node metastasis of clinically noninvasive, node-negative papillary thyroid microcarcinoma. Am J Surg 2014;208:412-8. [PubMed]
- Roh JL, Kim JM, Park CI. Central cervical nodal metastasis from papillary thyroid microcarcinoma: pattern and factors predictive of nodal metastasis. Ann Surg Oncol 2008;15:2482-6. [PubMed]
- Koo BS, Choi EC, Yoon YH, et al. Predictive factors for ipsilateral or contralateral central lymph node metastasis in unilateral papillary thyroid carcinoma. Ann Surg 2009;249:840-4. [PubMed]
- Popadich A, Levin O, Lee JC, et al. A multicenter cohort study of total thyroidectomy and routine central lymph node dissection for cN0 papillary thyroid cancer. Surgery 2011;150:1048-57. [PubMed]
- Kim WW, Park HY, Jung JH. Surgical extent of central lymph node dissection in clinically node-negative papillary thyroid cancer. Head Neck 2013;35:1616-20. [PubMed]
- Lim YC, Choi EC, Yoon YH, et al. Central lymph node metastases in unilateral papillary thyroid microcarcinoma. Br J Surg 2009;96:253-7. [PubMed]
- Oh EM, Chung YS, Lee YD. Clinical significance of Delphian lymph node metastasis in papillary thyroid carcinoma. World J Surg 2013;37:2594-9. [PubMed]
- Iyer NG, Kumar A, Nixon IJ, et al. Incidence and significance of Delphian node metastasis in papillary thyroid cancer. Ann Surg 2011;253:988-91. [PubMed]
- Kim WW, Yang SI, Kim JH, et al. Experience and analysis of Delphian lymph node metastasis in patients with papillary thyroid carcinoma. World J Surg Oncol 2012;10:226. [PubMed]
- Isaacs JD, McMullen TP, Sidhu SB, et al. Predictive value of the Delphian and level VI nodes in papillary thyroid cancer. ANZ J Surg 2010;80:834-8. [PubMed]
- Roh JL, Kim JM, Park CI. Central lymph node metastasis of unilateral papillary thyroid carcinoma: patterns and factors predictive of nodal metastasis, morbidity, and recurrence. Ann Surg Oncol 2011;18:2245-50. [PubMed]
- Kim SS, Lee BJ, Lee JC, et al. Preoperative ultrasonographic tumor characteristics as a predictive factor of tumor stage in papillary thyroid carcinoma. Head Neck 2011;33:1719-26. [PubMed]
- Wu LM, Gu HY, Qu XH, et al. The accuracy of ultrasonography in the preoperative diagnosis of cervical lymph node metastasis in patients with papillary thyroid carcinoma: A meta-analysis. Eur J Radiol 2012;81:1798-805. [PubMed]
- Lee DW, Ji YB, Sung ES, et al. Roles of ultrasonography and computed tomography in the surgical management of cervical lymph node metastases in papillary thyroid carcinoma. Eur J Surg Oncol 2013;39:191-6. [PubMed]
- Lim YS, Choi SW, Lee YS, et al. Frozen biopsy of central compartment in papillary thyroid cancer; quantitative nodal analysis. Head Neck 2013;35:1319-22. [PubMed]


