
Preoperative endoscopic retrograde biliary drainage increases postoperative complications after pancreaticoduodenectomy compared to endoscopic nasobiliary drainage
IntroductionOther Section
Pancreaticoduodenectomy (PD) is curative treatment for periampullary and pancreatic disease (1). Obstructive jaundice is the most common symptom in patients with periampullary cancer. It can exacerbate the risk of infectious complications and mortality post PD (2). Thus, preoperative biliary drainage was introduced to reduce the negative effects of obstructive jaundice in patients with periampullary neoplasms (3). Preoperative biliary drainage by percutaneous transhepatic biliary drainage (PTBD) or endoscopic biliary drainage (EBD) is performed to improve liver functions, including immunity and coagulation, that affect perioperative recovery in jaundiced patients (4). EBD has been shown to be superior to PTBD. PTBD is more invasive. In addition, PTBD has a higher rate of catheter tract metastases and complications (5). EBD can be performed through endoscopic retrograde biliary drainage (ERBD) or endoscopic nasobiliary drainage (ENBD). ENBD decompresses biliary obstruction by draining bile outside the body, avoiding regurgitation of the intestinal contents. The common drawback of ENBD is the loss of body fluid which may affect the recovery of hepatic function and immunity (6). ERBD normalizes bile flow in digestive tract which is important for improving metabolic and immune function and preventing bacterial translocation (7). Some studies have suggested that ENBD may be superior to ERBD in terms of perioperative morbidity (8,9). In that study, ERBD had a significantly higher risk for dysfunction than ENBD. In addition, pancreatic fistula rate was significantly lower in the ENBD group than in the ERBD group. However, there are few reports detailing the postoperative outcomes of ENBD and ERBD; and hence there is no clear consensus about which drainage is more suitable. Therefore, the purpose of this study was to compare the postoperative outcomes of ENBD and ERBD performed prior to PD. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/gs-20-711).
MethodsOther Section
Study design
Data from the medical records of 3 hospitals, Chuncheon, Kangdong, and Kangnam Sacred Heart hospitals, were collected retrospectively. From January 2007 to April 2019, PD was performed in 230 patients, among whom, 88 patients had undergone EBD. Endoscopists perform ENBD or ERBD based on personal opinion, hospital stay duration, economic costs, bile duct stenosis and equipment conditions. These 88 patients were divided into two groups according to the method of preoperative biliary drainage: ENBD versus ERBD. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board (IRB No. 2019-09-004-002) and individual consent for this retrospective analysis was waived.
Clinicopathological characteristics
Patient demographics included age, gender, preoperative symptoms, body mass index (BMI), comorbidities, history of abdominal surgery, American Society of Anesthesiologists (ASA) score, and preoperative serum bilirubin level. Intraoperative variables including operating time, blood loss, and blood transfusion were evaluated. Size of the tumor, margin status, and pathologic diagnosis were analyzed. Postoperative complications such as postpancreatectomy hemorrhage (PPH), delayed gastric emptying (DGE), and postoperative pancreatic fistula (POPF) were evaluated. POPF was defined by the International Study Group on Pancreatic Fistula definition (10). DGE was defined by the International Study Group on Pancreatic Surgery criteria (11). PPH was defined by the International Study Group on Pancreatic Surgery definition (12). The Clavien-Dindo classification was used to classify postoperative complications (13).
Statistical analysis
Categorical variables are presented as percentages. Continuous variables are presented as medians and ranges. Analysis was performed using the Student t-test or Mann-Whitney test for continuous variables and the Chi-squared test or Fisher’s exact test for categorical variables. The risk factors were evaluated by univariate and multivariate analyses with odds ratios and 95% confidence intervals using logistic regression. Statistical significance was defined as value of P<0.05.
ResultsOther Section
Clinicopathological characteristics
In the study, 88 patients underwent EBD prior to PD, of whom 42 (48.7%) underwent ERBD and 46 (52.3%) underwent ENBD. The characteristics of the 88 patients are summarized in Table 1. There were no significant differences between the two groups.
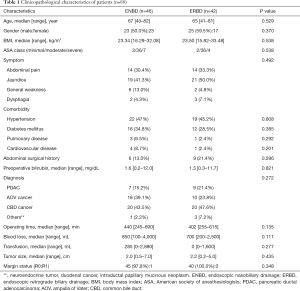
Full table
Postoperative outcomes
The overall complication rates in the ENBD group were significantly lower than in the ERBD group (26.1% vs. 57.1%, P=0.003). POPF rates (11.1% vs. 38.1%, P=0.003) and PPH rates (2.2% vs. 14.3%, P=0.036) in the ENBD group were lower than in the ERBD group. The median postoperative hospital stay in the ENBD and ERBD groups were 20 and 24 days, respectively (P=0.198). The 30-day mortality rates (2.2% vs. 2.4%; P=0.948) and the 90-day mortality rates (2.2% vs. 7.1%; P=0.264) in the ENBD and ERBD groups were similar (Table 2).
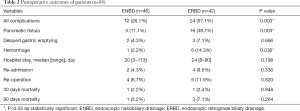
Full table
Risk factors for POPF and PPH
There were significant differences in the incidence of POPF and PPH between the ERBD group and ENBD group. Specific risk factors for POPF and PPH were analyzed. The results of univariate and multivariate analyses for POPF are shown in Table 3. On univariate analysis, ERBD, diabetes mellitus and a large volume of blood transfusion (>500 mL) were associated with POPF. On multivariate analysis, ERBD (OR =6.599; 95% CI, 1.825–23.859; P=0.004) and a large volume of blood transfusion (>500 mL) (OR =4.567; 95% CI, 1.336–15.614; P=0.015) were independent risk factors for POPF. Similarly, the results of univariate and multivariate analyses for PPH are shown in Table 4. The univariate analysis showed that ERBD, long operating time (>433 min) and a large volume of blood loss (>1,000 mL) were associated with PPH. The independent risk factors for PPH identified by multivariate analysis were ERBD (OR =13.797; 95% CI, 1.458–130.568; P=0.022) and a long operating time (>433 min) (OR =16.161; 95% CI, 1.719–152.498; P=0.015).
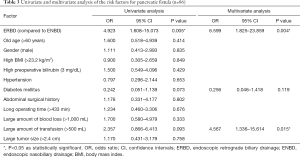
Full table
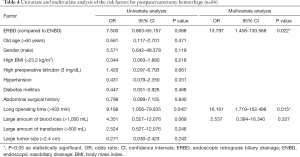
Full table
DiscussionOther Section
Surgical outcomes following PD have largely improved due to advances in perioperative management and medical knowledge (14). Nevertheless, surgical outcomes are determined not only by tumor characteristics, but also by associated jaundice due to biliary obstruction, patient characteristics, and comorbidities. Consequently, efforts to optimize the perioperative management could translate into significant benefit for patients undergoing PD, whose frequency is increasing (15).
Although meta-analyses and randomized controlled trials failed to prove the effectiveness of routine preoperative biliary drainage, it is still performed widely. The rationale behind this is that if bile duct obstruction is not adequately resolved, patients may not be able to receive further treatment (16). To enhance the therapeutic efficacy of treating biliary obstruction, surgeons have been primarily concerned with identifying ways to achieve the most effective drainage. ERBD is an internal drainage that involves placement of a plastic stent. During EBD, ERBD is preferred over ENBD with regard to comfort (17). ENBD is an external procedure that decompresses the obstructed bile ducts by draining out the bile, cytological examination of which can be used to confirm malignancy, in addition to cholangiography to evaluate longitudinal tumor spreading (18).
After EBD, cholangitis is one of the most common complications (8). Some studies reported that ENBD decreased the incidence of cholangitis before surgery compared to ERBD (19,20), and this might be because ENBD is an external drainage procedure. In addition to this, ERBD has been associated with a higher rate of cholangitis also due to tube occlusion (19). Similarly, stent dysfunction has been reported to occur more frequently in the ERBD group than in the ENBD group as, in ERBD, there is a risk of clogging of the stent or dislodgement, which may result in cholangitis (21). Gastrointestinal bacteria pass from ERBD to the sphincter of Oddi and reflux into the bile duct, whereas ENBD contains external drainage with less bile or gastrointestinal reflux (22). Thus, the placement of a stent can cause inflammation, while the manipulation of the papillae and the duct can cause cholangitis (23). Cholangitis is one of the factors that make PD challenging. With severe cholangitis, dissection is difficult and the risk of unnecessary injury increases, which can lead to complications.
POPF is one of the most dreaded complications after PD (24). Several studies have shown that preoperative biliary drainage can increase the complications from PD, including POPFs, which result from procedure related cholangitis and biliary bacterial translocation after drainage (25,26). Pancreatic secretions should be activated by bacterial phospholipase and lipopolysaccharide (27). Furthermore biliary tract infection is a significant risk factor for POPF (28). Our study illustrated that ERBD is a significant risk factor contributing to POPF development.
PPH is the most lethal complication of PD, related mortality being as high as 20% to 50% and its incidence ranging from 3% to 20% (29). In the present study, the incidence of PPH in the ENBD group was lower than in the ERBD group. ERBD may impact operative procedures during surgery, particularly during the dissection of the porta hepatis, because of periportal inflammation (15), which may explain the higher PPH rate in the ERBD group. Additionally, increased periportal inflammation corresponds to a higher risk of vascular wall damage during the dissection, which may increase the risk of PPH due to a pseudoaneurysm. Therefore, we find that ERBD does not appear to be the ideal choice in patients who are undergoing PD in terms of patient safety, due to a greater risk of complications.
This study has several limitations. First, this was a retrospective study and not a prospective randomized trial. There is significant potential for selection bias as there was no defined algorithm for selecting the biliary drainage method. Second, the scope of this study is limited due to disease heterogeneity. The degrees of combined inflammation vary with the specific diagnosis of disease. Third, because this is a multicenter study, technique and instrumentation varied from center to center.
In conclusion, our study provides further evidence that patients undergoing ERBD before PD are more likely to suffer POPF or PPH. Hence, ENBD may be preferred in order to minimize risk of POPF and PPH in patients with biliary obstruction, prior to PD. A well-designed randomized controlled trial is needed to produce more evidence of high quality.
AcknowledgmentsOther Section
Funding: None.
FootnoteOther Section
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/gs-20-711
Data Sharing Statement: Available at http://dx.doi.org/10.21037/gs-20-711
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/gs-20-711). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board (IRB No. 2019-09-004-002) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- Duan X, Jiang B, Zhou L, et al. Laparoscopic Pancreaticoduodenectomy: A Single Team Preliminary Experience. Surg Laparosc Endosc Percutan Tech 2017;27:356-60. [Crossref] [PubMed]
- Wu JM, Ho TW, Yen HH, et al. Endoscopic Retrograde Biliary Drainage Causes Intra-Abdominal Abscess in Pancreaticoduodenectomy Patients: An Important But Neglected Risk Factor. Ann Surg Oncol 2019;26:1086-92. [Crossref] [PubMed]
- Shin SH, Han IW, Ryu Y, et al. Optimal Timing of Pancreaticoduodenectomy Following Preoperative Biliary Drainage Considering Major Morbidity and Postoperative Survival. J Hepatobiliary Pancreat Sci 2019;26:449-58. [Crossref] [PubMed]
- Yang F, Jin C, Zou C, et al. Delaying surgery after preoperative biliary drainage does not increase surgical morbidity after pancreaticoduodenectomy. Surgery 2019;166:1004-10. [Crossref] [PubMed]
- Inamdar S, Slattery E, Ramandeep B, et al. Comparison of adverse events for endoscopic vs percutaneous biliary drainage in the treatment of malignant biliary tract obstruction in an inpatient national cohort. JAMA Oncol 2016;2:112-7. [Crossref] [PubMed]
- Kamiya S, Nagino M, Kanazawa H, et al. The value of bile replacement during external biliary drainage: an analysis of intestinal permeability, integrity, and microflora. Ann Surg 2004;239:510-7. [Crossref] [PubMed]
- Parks RW, Clements WD, Smye MG, et al. Intestinal barrier dysfuction in clinical and experimental obstructive jaundice and its reversal by internal biliary drainage. Br J Surg 1996;83:1345-9. [Crossref] [PubMed]
- Sasahira N, Hamada T, Togawa O, et al. Multicenter study of endoscopic preoperative biliary drainage for malignant distal biliary obstruction. World J Gastroenterol 2016;22:3793-802. [Crossref] [PubMed]
- Lin H, Li S, Liu X. The Safety and Efficacy of Nasobiliary Drainage Versus Biliary Stenting in Malignant Biliary Obstruction: A Systematic Review and Meta-Analysis. Medicine (Baltimore) 2016;95:e5253 [Crossref] [PubMed]
- Bassi C, Marchegiani G, Dervenis C, et al. The 2016 Update of the International Study Group (ISGPS) Definition and Grading of Postoperative Pancreatic Fistula: 11 Years After. Surgery 2017;161:584-91. [Crossref] [PubMed]
- Wente MN, Bassi C, Dervenis C, et al. Delayed Gastric Emptying (DGE) After Pancreatic Surgery: A Suggested Definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 2007;142:761-8. [Crossref] [PubMed]
- Wente MN, Veit JA, Bassi C, et al. Postpancreatectomy Hemorrhage (PPH): An International Study Group of Pancreatic Surgery (ISGPS) Definition. Surgery 2007;142:20-5. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of Surgical Complications: A New Proposal With Evaluation in a Cohort of 6336 Patients and Results of a Survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Lee H, Han Y, Kim JR, et al. Preoperative Biliary Drainage Adversely Affects Surgical Outcomes in Periampullary Cancer: A Retrospective and Propensity Score-Matched Analysis. J Hepatobiliary Pancreat Sci 2018;25:206-13. [Crossref] [PubMed]
- Coates JM, Beal SH, Russo JE, et al. Negligible Effect of Selective Preoperative Biliary Drainage on Perioperative Resuscitation, Morbidity, and Mortality in Patients Undergoing Pancreaticoduodenectomy. Arch Surg 2009;144:841-7. [Crossref] [PubMed]
- Kawakubo K, Kawakami H, Kuwatani M, et al. Lower incidence of complications in endoscopic nasobiliary drainage for hilar cholangiocarcinoma. World J Gastrointest Endosc 2016;8:385-90. [Crossref] [PubMed]
- Kaneko T, Imaizumi H, Kida M, et al. Influence of cholangitis after preoperative endoscopic biliary drainage on postoperative pancreatic fistula in patients with middle and lower malignant biliary strictures. Dig Endosc 2018;30:90-7. [Crossref] [PubMed]
- Yagioka H, Hirano K, Isayama H, et al. Clinical Significance of Bile Cytology via an Endoscopic Nasobiliary Drainage Tube for Pathological Diagnosis of Malignant Biliary Strictures. J Hepatobiliary Pancreat Sci 2011;18:211-5. [Crossref] [PubMed]
- Kawakami H, Kuwatani M, Onodera M, et al. Endoscopic nasobiliary drainage is the most suitable preoperative biliary drainage method in the management of patients with hilar cholangiocarcinoma. J Gastroenterol 2011;46:242-8. [Crossref] [PubMed]
- Sugiyama H, Tsuyuguchi T, Sakai Y, et al. Preoperative Drainage for Distal Biliary Obstruction: Endoscopic Stenting or Nasobiliary Drainage? Hepatogastroenterology 2013;60:231-4. [PubMed]
- Fujii T, Yamada S, Suenaga M, et al. Preoperative Internal Biliary Drainage Increases the Risk of Bile Juice Infection and Pancreatic Fistula After Pancreatoduodenectomy: A Prospective Observational Study. Pancreas 2015;44:465-70. [Crossref] [PubMed]
- Zhang GQ, Li Y, Ren YP, et al. Outcomes of preoperative endoscopic nasobiliary drainage and endoscopic retrograde biliary drainage for malignant distal biliary obstruction prior to pancreaticoduodenectomy. World J Gastroenterol 2017;23:5386-94. [Crossref] [PubMed]
- Silviera ML, Seamon MJ, Porshinsky B, et al. Complications Related to Endoscopic Retrograde Cholangiopancreatography: A Comprehensive Clinical Review. J Gastrointestin Liver Dis 2009;18:73-82. [PubMed]
- Xiong JJ, Tan CL, Szatmary P, et al. Meta-analysis of Pancreaticogastrostomy Versus Pancreaticojejunostomy After Pancreaticoduodenectomy. Br J Surg 2014;101:1196-208. [Crossref] [PubMed]
- Ngu W, Jones M, Neal CP, et al. Preoperative Biliary Drainage for Distal Biliary Obstruction and Post-Operative Infectious Complications. ANZ J Surg 2013;83:280-6. [Crossref] [PubMed]
- Gavazzi F, Ridolfi C, Capretti G, et al. Role of preoperative biliary stents, bile contamination and antibiotic prophylaxis in surgical site infections after pancreaticoduodenectomy. BMC Gastroenterol 2016;16:43. [Crossref] [PubMed]
- Kawai M, Tani M, Terasawa H, et al. Early Removal of Prophylactic Drains Reduces the Risk of Intra-Abdominal Infections in Patients With Pancreatic Head Resection: Prospective Study for 104 Consecutive Patients. Ann Surg 2006;244:1-7. [Crossref] [PubMed]
- Kajiwara T, Sakamoto Y, Morofuji N, et al. An Analysis of Risk Factors for Pancreatic Fistula After Pancreaticoduodenectomy: Clinical Impact of Bile Juice Infection on Day 1. Langenbecks Arch Surg 2010;395:707-12. [Crossref] [PubMed]
- Lu JW, Ding HF, Wu XN, et al. Intra-abdominal Hemorrhage Following 739 Consecutive Pancreaticoduodenectomy: Risk Factors and Treatments. J Gastroenterol Hepatol 2019;34:1100-7. [Crossref] [PubMed]


