
The clinical importance of multifocality on tumor recurrence in papillary thyroid carcinoma
Introduction
Multifocal papillary thyroid carcinoma (PTC) is defined as there are two or more. Multifocality is not a prognostic factor affecting TNM staging. It, however, is controversial to conclude multifocality is not a risk factor.
It is not sure that multifocality in PTC is multicentricity, which means independently arising PTCs. Multifocal PTC could be attributed to multicentricity or intrathyroidal spread of a single PTC (1,2); the latter might have a worse prognosis. The reasons multifocality is considered an important prognostic factor are as follow: (I) multifocality is associated with a cervical lymph node (CLN) metastasis (3,4), (II) multifocality is related to risk for recurrence (5), (III) multifocality is associated with BRAFV600E mutation (6). However, there are studies that multifocality is not related to increased recurrent or metastatic disease (7,8).
This study aimed to evaluate if multifocality in PTC is associated with a poor prognostic factor such as CLN metastasis, distant metastasis, or tumor recurrence.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/gs-20-603).
Methods
Patients & variables
We enrolled PTC patients sequentially who underwent thyroidectomy with or without CLN dissection and/or subsequent 131I remnant ablation treatment (RIA-T) at Sanggye Paik Hospital, Seoul, Korea, from January 2000 through December 2010. Lobectomy was performed if tumor size is less than 1 cm and no clinical extrathyroid extension on the pre-operative imaging such as neck ultrasonography or neck computed tomography. CLN dissection was performed if macroscopic CLN metastasis was present on the pre-operative imaging such as neck ultrasonography or neck computed tomography or during surgery. We reviewed retrospectively detailed histological reports. They included maximal tumor diameter, extrathyroid extension (no/microscopic/macroscopic), bilaterality (no/yes), multifocality (no/yes), and CLN metastasis (N0/N1a/N1b/Nx using TMN staging system by the American Joint Committee on Cancer, 7th ed.). We analyzed the demographics (age and gender) and clinical outcomes (distant metastasis and recurrence). We excluded cases to include missing data.
When recurrence in clinical or biochemical data was suggested, we performed radiologic studies, including neck ultrasonography. Recurrence was confirmed by cytological or histopathological examination. Patients with distant metastasis at the time of initial diagnosis were excluded from the analysis of recurrence.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Inje University Sanggye Paik Hospital (No. SGPAIK 2020-09-019) and individual consent for this retrospective analysis was waived.
Statistics
We presented categorical variables as numbers and percentages and compared using chi-square or Fisher’s exact test. We presented continuous variables as mean ± SD and range. We assessed the relationship between multifocality and other possible prognostic factors using binary logistic regression analysis. We compared recurrence by the Kaplan-Meier method (the log-rank test). The endpoint for the analysis of disease-free survival was a recurrence. We analyzed a prognostic factor for recurrence using Cox’s proportional hazard model (the stepwise forward method). P value of <0.05 was considered significant. We performed all statistical analyses using SPSS (version 25.0; IBM Corp., Armonk, NY, USA).
Results
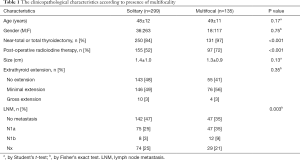
Clinicopathological characteristics (Table 1)
Full table
We enrolled a total of 434 PTC patients (380 women and 54 men; mean age, 48 years). The median follow-up period was 122 (range, 1–240) months. A total of 434 patients with PTC, who underwent thyroidectomy with or without CLN dissection, were identified at Sanggye Paik Hospital. Of 434 patients, 135 patients (31%) had multifocal tumors.
Of a total of 381 patients who underwent near-total or total thyroidectomy, 131 patients (34%) had multifocal tumors. Of a total of 53 patients with PTC, who underwent thyroid lobectomy, four patients (7.5%) had multifocal tumors.
Mean age, gender, tumor size, and extrathyroid extension were not significantly different between single and multifocal groups. Compared with patients with single PTC, a multifocal PTC group demonstrated a higher ratio of near-total or total thyroidectomy (P<0.001) and RAI-T (P<0.001), and higher CLN metastasis (P=0.003).
Recurrence, disease-free survival (Figure 1)
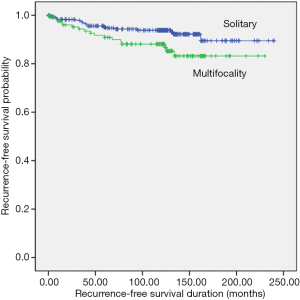
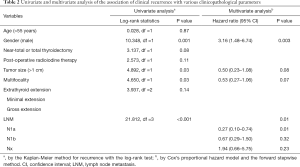
Of a total of 434 patients, 36 (8%) had a recurrence. Multifocality was significantly associated with tumor recurrence during the follow-up period (median 122 months): 13% [17 patients; lymph node (LN), 16 patients; contralateral lobe, 1 patient; median 40 months] of the multifocal group compared with 6% (19 patients; LN, 14 patients; contralateral lobe, 5 patients; median 45 months) of the single group (P=0.03 by log-rank test; Figure 1). However, this association disappeared on multivariate analysis, adjusting for conventional clinicopathological predictors of recurrence (Table 2).
Full table
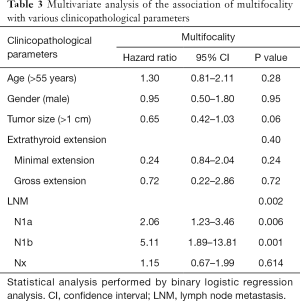
Multivariate analysis of the association of multifocality with various clinicopathological parameters (Table 3)
Full table
We analyzed associations between multifocality and clinic-pathological parameters used for predicting recurrences, such as age, gender, tumor size, extrathyroid extension, and CLN metastasis using multivariate analysis. The association between multifocality and CLN metastasis remained significant with multivariate analysis after adjusting for clinicopathological parameters (P<0.001).
Discussion
In this study, we evaluated if multifocality in PTC is associated with a poor prognostic factor such as CLN metastasis, distant metastasis, or tumor recurrence. This study showed that multifocality was associated with CLN metastasis and tumor recurrence in patients with PTC. However, the association between multifocality and tumor recurrence disappeared on multivariate analysis, adjusting for poor prognostic factors.
Multifocality has a significant association with CLN metastasis after adjusting for poor prognostic factors. In logistic regression analysis, multifocality was associated with central LN (N1a) metastasis (hazard ratio, 2.06) and lateral LN (N1b) metastasis (hazard ratio, 5.11). In other studies, multifocality is associated with central or lateral CLN metastasis (9,10). CLN metastasis is known for poor prognosis, mostly lateral CLN metastasis, more aggressive (11). However, pre-operative neck ultrasonotraphy was reported to have low sensitivity for central lymph node metastasis (LNM) (12) and lateral LNM (13). If multifocalicy of PTC is present, close monitoring of CLN metastasis is needed.
Multifocality has a significant association with CLN metastasis, why cannot it affect recurrence?
First, the degree of multifocality might be different. Although it is defined as multifocality when there are two or more PTCs, the number of tumors was very variable in this study, such as 2, 3, 4, 5, 7, and many multiple tumors. Kim et al. reported that multifocality and the number of tumor lesions were an independent risk factor for recurrence (5). In this study, however, there were rarely many multiple tumors, so the analysis of tumor recurrence based on the number of tumors did not produce significant results (data not shown). The concept of total tumor diameter (TTM) may also be used to overcome this limit. In papillary thyroid microcarcinoma (PTMC), Zhao et al. reported multifocal PTMC with TTM as the sum of the maximal diameter of each tumor >1 cm had a similar risk of LNM, so, they recommended routine central neck dissection in this subgroup (14). But this study did not analyze TTM.
Second, multifocality might be mixed with intraglandular metastases and multicentricity. Either intraglandular metastases from a single PTC or independent neoplastic clones are proven as to how multifocal PTC form (1,2). A lymphatic drainage system can cause intra-thyroidal metastatic spreading. It contains a communicating network of intralobular lymphatic vessels in both lobes and the isthmus enclosed in a capsule (2). A study in the Korean population showed at least 39.5% of the multifocal PTC could be caused to independently arising PTCs rather than to intra-thyroidal spread of single PTC (15). That is, in about 40% of multifocal PTC, multifocality could not be a worse prognostic factor. However, we did not study the origin of multifocal PTC (intrathyroidal spread of single PTC vs. multicentricity).
Third, it may be because almost all patients with multifocal PTCs underwent total thyroidectomy and/or RAI-T. In this study, 97% of total patients with multifocal PTCs underwent more than subtotal thyroidectomy compared to 84% of those with solitary PTCs. Only 3% of total patients with multifocal PTCs underwent lobectomy, and only one patient developed recurrence in the contralateral lobe. However, Harries et al. showed that unifocal PTC and multifocal PTC patients had similar rates of recurrence of the contralateral lobe, regional recurrence, and overall survival with a median follow-up of 58 months (16). RAI-T also did not decrease the risk of recurrence in PTC (17).
Fourth, multifocality may be a factor that has nothing to do with a worse prognosis. Poor prognosis may be more strictly related to other carcinogenic genes involved and underlying molecular mechanisms of tumor development and progression. Or it may take too much time to find out the risk of multifocality because PTC has an excellent prognosis. However, this also means that if it occurs at a very young age, it may be a factor that may affect relapse after decades.
This study has some limitations. First, the subject of this study is the heterogeneous population. We analyzed patients with near-total or total thyroidectomy or lobectomy. However, there was no different recurrent rate between a total thyroidectomy group and a lobectomy group (data not sown). Second, Nx accounted for a considerable percentage. LN dissection was performed if macroscopic CLN metastasis was present on the pre-operative imaging such as neck ultrasonography or neck computed tomography or during surgery. LN dissection only based on a macroscopic involvement can be an important bias. However, microscopic subclinical CLN metastases have a much smaller risk of recurrence than clinical macroscopic CLN metastases (18). Even if Nx is a high percentage, it is considered that the likelihood of having an overall prognosis is minimal.
However, this study has some strengths. First, this study is suitable to see the prognosis of PTC progressing slowly by following up for more than 10 years. Second, this data represents the real world by reflecting realistic surgery such as lobectomy, total thyroidectomy, and/or Nx.
Conclusions
In conclusion, multifocality could be associated with poor prognoses such as CLN metastasis and tumor recurrence. However, this association with multifocality and tumor recurrence disappeared on multivariate analysis. Therefore, we suggest that multifocality could belong to the low risk factor of PTC, but CLN metastasis should be closely monitored.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The author has completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/gs-20-603
Data Sharing Statement: Available at http://dx.doi.org/10.21037/gs-20-603
Peer Review File: Available at http://dx.doi.org/10.21037/gs-20-603
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/gs-20-603). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Inje University Sanggye Paik Hospital (No. SGPAIK 2020-09-019) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Giannini R, Ugolini C, Lupi C, et al. The heterogeneous distribution of BRAF mutation supports the independent clonal origin of distinct tumor foci in multifocal papillary thyroid carcinoma. J Clin Endocrinol Metab 2007;92:3511-6. [Crossref] [PubMed]
- Shattuck TM, Westra WH, Ladenson PW, et al. Independent clonal origins of distinct tumor foci in multifocal papillary thyroid carcinoma. N Engl J Med 2005;352:2406-12. [Crossref] [PubMed]
- Ricci JA, Alfonso AE. Multifocal micropapillary thyroid cancer: a new indication for total thyroidectomy? Am Surg 2012;78:1211-4. [Crossref] [PubMed]
- Pellegriti G, Scollo C, Lumera G, et al. Clinical behavior and outcome of papillary thyroid cancers smaller than 1.5 cm in diameter: study of 299 cases. J Clin Endocrinol Metab 2004;89:3713-20. [Crossref] [PubMed]
- Kim HJ, Sohn SY, Jang HW, et al. Multifocality, but not bilaterality, is a predictor of disease recurrence/persistence of papillary thyroid carcinoma. World J Surg 2013;37:376-84. [Crossref] [PubMed]
- Zhang Q, Liu SZ, Zhang Q, et al. Meta-analyses of association between BRAF(V600E) mutation and clinicopathological features of papillary thyroid carcinoma. Cell Physiol Biochem 2016;38:763-76. [Crossref] [PubMed]
- Ross DS, Litofsky D, Ain KB, et al. Recurrence after treatment of micropapillary thyroid cancer. Thyroid 2009;19:1043-8. [Crossref] [PubMed]
- Neuhold N, Schultheis A, Hermann M, et al. Incidental papillary microcarcinoma of the thyroid--further evidence of a very low malignant potential: a retrospective clinicopathological study with up to 30 years of follow-up. Ann Surg Oncol 2011;18:3430-6. [Crossref] [PubMed]
- Sheng L, Shi J, Han B, et al. Predicting factors for central or lateral lymph node metastasis in conventional papillary thyroid microcarcinoma. Am J Surg 2020;220:334-40. [Crossref] [PubMed]
- So YK, Kim MJ, Kim S, et al. Lateral lymph node metastasis in papillary thyroid carcinoma: a systematic review and meta-analysis for prevalence, risk factors, and location. Int J Surg 2018;50:94-103. [Crossref] [PubMed]
- Leboulleux S, Rubino C, Baudin E, et al. Prognostic factors for persistent or recurrent disease of papillary thyroid carcinoma with neck lymph node metastases and/or tumor extension beyond the thyroid capsule at initial diagnosis. J Clin Endocrinol Metab 2005;90:5723-9. [Crossref] [PubMed]
- Ito Y, Tomoda C, Uruno T, et al. Clinical significance of metastasis to the central compartment from papillary microcarcinoma of the thyroid. World J Surg. 2006;30:91-9. [Crossref] [PubMed]
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;26:1-133. [Crossref] [PubMed]
- Zhao Q, Ming J, Liu C, et al. Multifocality and total tumor diameter predict central neck lymph node metastases in papillary thyroid microcarcinoma. Ann Surg Oncol 2013;20:746-52. [Crossref] [PubMed]
- Park SY, Park YJ, Lee YJ, et al. Analysis of differential BRAF(V600E) mutational status in multifocal papillary thyroid carcinoma: evidence of independent clonal origin in distinct tumor foci. Cancer 2006;107:1831-8. [Crossref] [PubMed]
- Harries V, Wang LY, McGill M, et al. Should multifocality be an indication for completion thyroidectomy in papillary thyroid carcinoma? Surgery 2020;167:10-7. [Crossref] [PubMed]
- Kim SK, Woo JW, Lee JH, et al. Radioactive iodine ablation may not decrease the risk of recurrence in intermediate-risk papillary thyroid carcinoma. Endocr Relat Cancer 2016;23:367-76. [Crossref] [PubMed]
- Randolph GW, Duh QY, Heller KS, et al. The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid 2012;22:1144-52. [Crossref] [PubMed]


