
Pseudomonas aeruginosa injection decreases drainage in lateral neck dissection for metastatic thyroid cancer
Introduction
Papillary thyroid carcinoma (PTC), which accounts for 85−90% of thyroid malignant tumors has jumped to top 5 of most common cancer in female, with its consistent increase in incident rate around the world in recent decades (1). Due to its severe threat to peoples’ health and livelihood, how to improve the diagnosis and treatment as well as prognosis of PTC has become the hot topic in the area of thyroid diseases. The prognosis of PTC is exciting after resection surgery and iodine 131 ablation. Lateral neck dissection (LND) is commonly performed following total thyroidectomy (TT) and central neck dissection (CND) for lateral neck metastasis in papillary thyroid cancer (PTC) patients (2). For this procedure, a drainage tube under negative pressure is routinely put into the cavity to keep the lateral neck dry, due to a large traumatic cavity that is left after operation. The tube keeps the cavity dry by sucking lymph and tissue fluid until the daily output decreases to <30 mL (3). The duration of hospitalization stay generally depends on when the tube is removed. Since chyle leakage and hemorrhage occur at a relatively low rate (5–8% vs. 0.1–2.1%), the hospitalization stay is determined by the volume of the drainage (4-6).
Pseudomonas aeruginosa injection (PAI) (Beijing Wanter Bio-pharmaceutical Company, Beijing, China) is made from the inactive P. aeruginosa mannose-sensitive hemagglutinin strain (PA-MSHA) diluted by phosphate buffer solution.PA-MSHA was first isolated by Mu et al. in 1985 (7). In the early days, the PAI was made from PA-MSHA. Later on, a reduced live vaccine, which was generated with fimbria through gene engineering, came into use (8). Fimbriae are glycoprotein-like ligands with strong adhesive capabilities, whose ends can specifically bind with mannose. Fimbriae can prevent the receptor from binding to the ligand which are related to tumor growth and metastasis, thus affecting antitumor growth and metastasis. PAI has been approved by the Chinese Food and Drug Administration (CFDA) and has been used as an adjuvant drug for the treatment of malignant tumors (9).
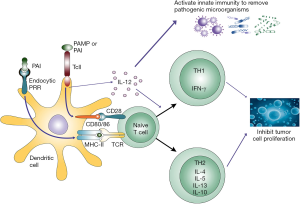
PA-MSHA can activate Toll-like receptors and then stimulate immune response, which inhibits tumor cell proliferation and has a significant anti-infection effect (10). Recent studies have suggested that the PA-MSHA can effectively activate the Toll-like receptor of immune cells, which induce antigen presentation cell (APC) maturation, and in turn trigger natural killer (NK) cell and T cell differentiation and maturation, thereby killing the tumor cells (11,12) (Figure 1). Zhu et al. find that PA-MSHA has the direct anticancer cytotoxic effect through down regulating the PI3K-AKT-mTOR signaling pathway in bladder cancer cell (13). Cheng et al. find that PA-MSHA induct apoptosis in pancreatic cancer cells by inhibiting of EGFR signaling pathway and activating of the caspase pathway (14). In the process, sterile inflammation activated by PA-MSHA can reinforce wound adhesion and promote healing (15). Furthermore, it appears that regional aseptic inflammation can induce wound adhesion, thus promoting the closure of the small lymphatics. In China, the drug has been sprayed on the surface of wound cavities to reduce the postoperative drainage volume after pelvic lymph node dissection when treating cervical cancer. Both Song et al. and Ma et al. reported that retrograded injecting the PAI into the armpit were helpful for treating subcutaneous hydrops after radical mastectomy (16,17). Also PAI has shown to have high accuracy in treating malignant pleural effusion and hydropericardium (18,19). In our center, PAI has also been used for managing chylous leakage after LND for thyroid cancer by retrograde injection from drainage tube (20) or ultrasound-guided percutaneous injection (21). Genpeng et al. reported the incidence of chylous leakage decreased after intraoperative prophylactic use of PAI (22).
Although PAI has proven to be effective in treating postoperative chyle leakage after LND, there are no studies demonstrating its positive function in reducing the drainage volume after LND—an outcome which could shorten hospital stay. Therefore, the aim of this study was to assess whether PAI can effectively reduce drainage after LND.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/gs-20-731).
Methods
Study design
PTC patients with lymph node metastasis (LNM) who underwent TT with CND and LND performed by a single surgeon at the Thyroid Surgery Department of the Chengdu Shangjin Nan Fu Hospital, West China Hospital, S.C.U., China between March 1, 2016 and September 30, 2017 were enrolled in the current study. The clinical data of all patients were retrospectively analyzed. The Ethics Committee of the Chengdu Shangjin Nan Fu Hospital, West China Hospital, S.C.U., China approved the present study. All procedures performed in this study including human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from all the individuals prior to their participation. The patients who previously underwent neck surgery or had PTC metastasis over the ipsilateral neck area were excluded from the study. As this study focused on the drainage after operation, the patients who were diagnosed with chyle leakage or postoperative hemorrhage were also excluded from the study. The inclusion criteria was as follows: (I) 18 to 70 y of age; (II) PTC with proven lateral lymph node metastasis; (III) acceptance of TT with CND and LND performed by a single surgeon, and (IV) written informed consent. The exclusion criteria was as follows: (I) a history of surgery in the lateral neck compartment; (II) the PTC metastasis over the ipsilateral neck area; (III) the patient occurred postoperative complications such as chylous fistula, bleeding and seroma.
Intervention
In all patients that underwent preoperative ultrasonography and computed tomography (CT), the location and size of the thyroid tumor and the potential LNMs were evaluated. Then, following fine-needle aspiration biopsy, a further investigation was made to establish a definite diagnosis after the positive pathological results were obtained. All patients with ipsilateral LNM graded between levels II to V, underwent TT with CND and LND. After the bleeding was completely stopped and no leakage of the thoracic duck or its branches was confirmed, 2 mL of PAI (bacteria count 1.2×1010/L; Wanter Bio-pharmaceutical Company, Beijing, China) were sprayed evenly onto the surface of the dissected lateral neck area in PAI-group patients, while no treatment in control group. Before the PAI was sprayed, the wound was sucked to maintain dryness (Figure 2). For each patient, two closed suction drains with negative pressure were placed into the dissection area; one was placed into the cervical area and another into the lateral area.

Outcome assessment
The patients were divided into two groups: the PAI group and the non-PAI group. Moreover, we compared the clinicopathologic features of the two groups, including the gender, age, BMI, tumor size, main tumor location, multiplicity, bilaterality, thyroiditis, capsular invasion, number of lymph node metastases, total number of harvested lymph nodes, median volume of peak 24-hour drainage, median volume of total drainage, postoperative hospital stay, and complications. The two drains were sequentially removed when the amount of the drainage decreased to <30 mL a day respectively, which was checked by the ward nurse every morning. The postoperative hemorrhage was diagnosed when sudden swelling of the neck occurred or bleeding more than 50 mL/h lasted for more than 3 hours. For patients with airway compression, the observation was terminated, and the patient underwent further neck re-exploration. Chyle leakage was diagnosed by finding milky liquid leakage confirmed by laboratory tests that revealed a triglyceride concentration of >100 mg/dL or higher compared to serum concentration (23). Patients were followed up at 1, 3, 6, and 12 months after surgery at our outpatient ward. Thyroid function and the parathyroid function were evaluated, with the ultrasonography being performed at 3, 6, and 12 months after surgery.
Statistical method
Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) version 18.0 for Windows (IBM Corp., Armonk, NY, USA). Descriptive data are presented as count and percentage, mean and standard deviation, or median and range. Methods, including student’s t-test, the Wilcoxon rank-sum test, the chi-square test, and Fisher’s exact test, were employed to compare the data between the two groups. A P value <0.05 was considered statistically significant.
Results
Protocol violations
During the study period, 93 patients with PTC met the inclusion criteria. 6 patients had previously undergone partial thyroidectomy, 1 patient from the non-PAI group developed chylous fistula, and 1 patient from the PAI group developed seroma. Ultimately, 44 patients used PAI as PAI group and remaining 41 patients as control group were included in the study.
Clinical characteristics
A total of 85 patients, including 21 men and 64 women (ratio 1:3.0) with a mean age of 36.8±13.6 years (range, 13–76 years), a mean body weight of 59.3±10.4 kg, and a mean BMI 22.5±3.4 kg/m2 were included in the study. The mean diameter of the main foci was 2.2±0.9 cm, with 33 that were laid on the left lobe and 52 on the right (ratio 1:1.6). In total, 54 patients (63.5%) and 44 patients (51.8%) were diagnosed with multifocal tumors and bilateral tumors, respectively. In addition, 31 patients (36.5%) were diagnosed with thyroiditis according to a rise in thyroid peroxidase antibody (TPOAb) level, and extrathyroidal invasion, including strap muscle invasion, was observed in 65 patients (76.5%). Lymph nodes metastasis and total lymph nodes were 9.9±5.6 and 41.4±14.9, respectively. The median volume of peak 24-hour drainage and total drainage were 122 mL (range, 60–301 mL) and 329 mL (range, 127–916 mL), respectively (Table 1).
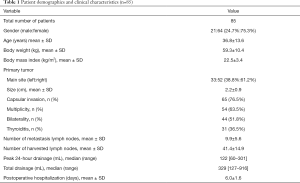
Full table
Outcome assessment
PAI was splashed onto the dissected lateral neck area of 44 out of 85 patients (51.8%) while it was not used in the other 41 patients (48.2%). There were no significant differences between the two groups in terms of age, gender, BMI, pathologic features, the number of the lymph nodes metastases, and the total harvested lymph nodes. The median volumes of peak 24-hour drainage which appeared during the first day after operation had few differences [112 (range, 60–203) vs. 124 (range, 76–301) mL; P=0.147]. Nonetheless, from the second day on, the volume was smaller in patients using PAI than in those who were not treated with PAI. Accordingly, the median volume of the total drainage was significantly smaller in patients treated with PAI compared to those who were not treated with PAI [295 (range, 127–585) vs. 356 (range, 146–916) mL; P<0.05]. Postoperative fever, which was defined as fever over 37.5 °C was observed in 23 cases (51.1%) in the PAI group and in 4 cases (9.8%) in the non-PAI group (P<0.001). Since the temperature was not higher than 39.0 °C, the patients were treated with non-steroidal anti-inflammatory drugs (NSAIDs) without antibiotics. The mean postoperative hospitalization stay at hospital was significantly shorter in patients with PAI compared to those without (5.5±1.8 vs. 6.6±1.3 days; P<0.05) (Table 2).
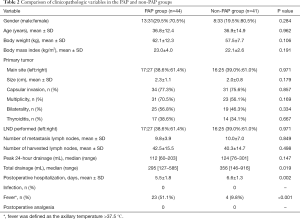
Full table
Post-operation recurrence
In both groups, ultrasonography revealed no tumor recurrence on the 12th month after operation. Also, none of the patients had permanent recurrent laryngeal nerve paralysis (RLNP).
Discussion
At our department, LND is considered to be a routine operation for treatment of PTC with clinical N1b (24). The drainage tube is placed into the cavity for suction with the aim of observing possible hematoma or lymphorrhagia formation, and is usually removed in 5 to 7 days after operation when the drainage drops below 30 mL per day (25). Since postoperative bleeding occurs at relatively low rate, the displacement of the drainage tube determines the duration of hospital stay.
Wei et al. have reported that retrograded injection of PAI into the suction drainage from the cavity of the stump can cure chylous fistula after LND. In their study, all 18 patients with chylous fistula following LND were rapidly cured by PAI without extra complications (26). In another study, PAI was sparged onto the pelvic cavity after radical trachelectomy and pelvic lymphadenectomy. The volume of drainage in the group treated with PAI was lower than that of the control group (27). PAI also reduces malignant pleural effusion and refractory pericardial effusion, and can even reduce lymphorrhagia after Whipple procedure (28).
In this study, the drainage volume on day 1 after operation showed no significant difference; however, it was lower in the PAI group compared to the non-PAI group from the day 2 onwards. The decline of drainage was often accompanied with the higher temperature in the PAI group. Possibly, the inflammation caused by PA-MSHA stimulated an increased formation of collagen in the wound which then promoted wound healing. When enough collagen is formed, it blocks the lymph-vessel, and the drainage volume declines on day 2. Consequently, the drain tube can be removed 1–2 days in advance, thus shortening the length of hospital stay.
Previous reports have shown that subcutaneous injecting PAI can cause local skin allergy and fever without other major complications. Chen et al. report some patients developed fever and neck pain after retrograde injecting PAI into wound cavity from drainage tube. These minor complications were easy to control. No serious complication was observed in the period of the study (29). In this study, sterile inflammation of the neck led to low-grade fever, pain and local swelling, however there was no damage to accessory nerves, phrenic nerves, vagus nerves, or the brachial plexus, and no increased risk of bleeding. Instead, the neck swelling exerted higher pressure around the lymphatic channel and capillary, which helps decrease the neck cavity effusion. The temperature was usually below 39.0 degrees, but it only last for 1 or 2 days. The symptom can be alleviated with 1–2 doses of antipyretic. Although the PAI group had a higher incidence of inflammation, the algesia was well tolerated by all patients, and so none were treated with painkillers. Therefore, we believe that the intraoperative topical use of PAI can reduce the cervical drainage volume and thus shorten the length of hospital stay without incurring major complications but further study is required.
Some limitations to the present study should also be noted. These include its small sample size and short follow-up time. Despite this, the obtained results are robust enough to demonstrate the safety and efficacy of using PAI in reducing the drainage volume after LND. Due to the limited follow-up time, we were not able to assess whether PAI could reduce the relapse rate, even though PAI was originally designed as an anticancer drug. Therefore, further studies with long-term follow-up are required to determine whether the recurrence rate is different.
Conclusions
The application of PAI to the LND cavity for PTC patients with lateral LNM is safe and effective approach for reducing drainage volume of the wound cavity during LND. Further studies are necessary to provide additional support for our observations and conclusions and to observe the anticancer effect of PAI in PTC.
Acknowledgments
The authors wish to thank Dr. Junhe Gou for his help in collecting the patient’s clinicopathological data.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/gs-20-731
Data Sharing Statement: Available at http://dx.doi.org/10.21037/gs-20-731
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/gs-20-731). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The Ethics Committee of the Chengdu Shangjin Nan Fu Hospital, West China Hospital, S.C.U., China approved the present study. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from all the individuals prior to their participation.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Siegel RL, Miller KD, Jemal A. 2017 Cancer statistics. CA Cancer J Clin 2017;67:7e30.
- Li F, Wu Y, Chen L, et al. Evaluation of clinical risk factors for predicting insidious right central and posterior right recurrent laryngeal nerve lymph node metastasis in papillary thyroid microcarcinoma patients (cN0): experience of a single center. Ann Transl Med. 2019;7:8. [Crossref] [PubMed]
- Amir I, Morar P, Belloso A. Postoperative drainage in head and neck surgery. Ann R Coll Surg Engl 2010;92:651-4. [Crossref] [PubMed]
- Delaney SW, Shi H, Shokrani A, et al. Management of Chyle Leak after Head and Neck Surgery: Review of Current Treatment Strategies. Int J Otolaryngol 2017;2017:8362874. [Crossref] [PubMed]
- Miccoli P, Materazzi G, Macerola E, et al. Tailored surgery according to molecular analysis in differentiated thyroid carcinomas. Gland Surg 2018;7:S30-3. [Crossref] [PubMed]
- Farooq MS, Nouraei R, Kaddour H, et al. Patterns, timing and consequences of post-thyroidectomy haemorrhage. Ann R Coll Surg Engl 2017;99:60-2. [Crossref] [PubMed]
- Mu XY. The first breeding of Pseudomonas aeruginosa mannose sensitive hemagglutinin strain. Journal of Dalian Medical College 1985;1:1-3.
- Fass R, van de Walle M, Shiloach A, et al. Use of high density cultures of Escherichia coli for high level production of recombinant Pseudomonas aeruginosa exotoxin A. Appl Microbiol Biotechnol 1991;36:65-9. [Crossref] [PubMed]
- Lv F, Cao J, Liu Z, et al. Phase II study of Pseudomonas aeruginosa-Mannose-Sensitive hemagglutinin in combination with capecitabine for Her-2-negative metastatic breast cancer pretreated with anthracycline and taxane. PLoS One 2015;13;10:e0118607.
- Zhang J, Xu K, Ambati B, et al. Toll-like receptor 5-mediated corneal epithelial inflammatory responses to Pseudomonas aeruginosa flagellin. Invest Ophthalmol Vis Sci 2003;44:4247-54. [Crossref] [PubMed]
- Zhang M, Luo F, Zhang Y, et al. Pseudomonas aeruginosa mannose-sensitive hemagglutinin promotes T-cell response via toll-like receptor 4-mediated dendritic cells to slow tumor progression in mice. J Pharmacol Exp Ther 2014;349:279-87. [Crossref] [PubMed]
- Zhang YY, Wang HT, Li YQ, et al. The Pseudomonas aeruginosa Mannose Sensitive Hamemagglutination Strain (PA-MSHA) Induces a Th1-Polarizing Phenotype by Promoting Human Dendritic Cells Maturation. Indian J Microbiol 2014;54:163-9. [Crossref] [PubMed]
- Zhu YP, Bian XJ, Ye DW, et al. Pseudomonas aeruginosa-mannose-sensitive hemagglutinin inhibits proliferation and induces apoptosis in a caspase-dependent manner in human bladder cancer cell lines. Oncol Lett 2013;5:1357-62. [Crossref] [PubMed]
- Cheng X, Wang B, Jin Z, et al. Pseudomonas aeruginosa-mannose-sensitive hemagglutinin inhibits pancreatic cancer cell proliferation and induces apoptosis via the EGFR pathway and caspase signaling. Oncotarget 2016;7:77916-25. [Crossref] [PubMed]
- Liu XF, Wang L, Qu Y, et al. Effect of the PA-MSHA vaccine on septic serum-induced inflammatory response. Mol Med Rep 2013;7:1350-4. [Crossref] [PubMed]
- Song AL, Cao N. Clinical study of PAI in the treatment of subcutaneous hydrops after radical mastectomy. Medical Journal of Liaoning 2012;26:57-60.
- Ma FY, Wang LQ, Wang CL, et al. Clinical application of PAI in treatment of subcutaneous hydrops after radical mastectomy. Chinese Journal of Cancer Prevention and Treatment 2009;14:1111-2, 1119.
- Xie F, Zhang JH. Clinical analysis of Pseudomonas aeruginosa injection in the treatment of malignant pleural effusion. Chinese Journal of Clinical Pulmonary Medicine 2016;03:528-30.
- Zhu YF, Wei JZ, Gu YF. Clinical observation of 23 cases of malignant pericardial effusion treated by intracavitary injection of Pseudomonas aeruginosa injection. Chinese Journal of Modern Oncology Medicine 2011;12:2458-9.
- Wei T, Zhu XX, Chen R, et al. Clinical analysis of Pseudomonas aeruginosa Injection in treating chylous fistula after lateral neck dissection in thyroid cancer. Chinese Journal of Bases and Clinics in General Surgery 2013;20:325-7.
- Chen Q, Chen Y, Su A, et al. Ultrasound-guided percutaneous injection of Pseudomonas aeruginosa-mannose sensitive hemagglutinin for treatment of chyle fistula following neck dissection. Medicine (Baltimore) 2020;99:e18816. [PubMed]
- Genpeng L, Jinen S, Tao W, et al. Intraoperative application of inactivated Pseudomonas aeruginosa in patients undergoing lateral neck dissection for metastatic thyroid cancer: A randomized, parallel group, placebo-controlled trial. Surgery 2020;168:340-6. [PubMed]
- Campisi CC, Boccardo F, Piazza C, et al. Evolution of chylous fistula management after neck dissection. Curr Opin Otolaryngol Head Neck Surg 2013;21:150-6. [Crossref] [PubMed]
- Ito Y, Fukushima M, Tomoda C, et al. Prognosis of patients with papillary thyroid carcinoma having clinically apparent metastasis to the lateral compartment. Endocr J 2009;56:759-66. [Crossref] [PubMed]
- Woods RS, Woods JF, Duignan ES. Systematic review and meta-analysis of wound drains after thyroid surgery. Br J Surg 2014;101:446-56. [Crossref] [PubMed]
- Wei T, Liu F, Li ZH, et al. Novel management of intractable cervical chylous fistula with local application of pseudomonas aeruginosa injection. Otolaryngol Head Neck Surg 2015;153:561-5. [Crossref] [PubMed]
- Zi D, He LP, Yang YJ, et al. Effect on postoperative lymphatic drainage by local spraying and subcutaneous injection of PAP in patients with cervical cancer. Medical Journal of Shandong 2011;51:80-1.
- Wang B, Wu YS, Zhang M. Clinical analysis of PAI in treatment of lymphatic leakage after Whipple procedure. Chinese Journal of Modern Drug Application 2015;9:150-1.
- Chen Q, Zhou XH, Ma Y, et al. Pseudomonas aeruginosa-mannose sensitive hemagglutinin injection therapy for the treatment of chyle fistula following neck dissection. Head and Neck 2020;42:725-31. [Crossref] [PubMed]
(English Language Editor: J. Gray)


