A multiple logistic regression analysis of complications following microsurgical breast reconstruction
Introduction
High-risk patients are considered to be some of the most challenging to reconstructive surgeons. These patients are defined as those with co-morbidities such as obesity, tobacco use, and poorly controlled diabetes mellitus as well as prior reconstructive failures and previous radiation therapy. In these high risk patients, complications are often increased and because of that, reconstructive algorithms may require modification. Traditional methods of reconstruction may not provide predictable outcomes and therefore alternative options should be considered.
Breast reconstruction following mastectomy ranks among the most common of all reconstructive procedures performed. With changing demographics and cancer treatment algorithms such as radiation therapy, breast reconstruction has become more challenging. Obesity has become an epidemic problem in the USA and with it comes a multitude of other problems such as diabetes mellitus and hypertension. Tobacco use remains a social botheration and poses additional challenges to the reconstructive surgeon. The indications for radiation therapy continue to increase and the number of women who are plagued by the vascular and soft tissue effects of radiation therapy is not trivial.
Microvascular breast reconstruction has been a significant advancement in overcoming many of the limitations of traditional breast reconstruction especially in the high-risk patient. Although we practice in an era of high flap success rates following microsurgical breast reconstruction, complications can still occur. Several studies have evaluated the impact of risk factors on microvascular outcomes in the setting of a particular type of patient or with a particular type of flap. However, few studies that have evaluated a consecutive series of high-risk patients will all types of microvascular breast reconstruction. With that in mind, it was the intent of this study to gain a better understanding of the relationship between risk factors and complications in order to provide useful information for patients and surgeons considering free flap breast reconstruction in high-risk patients.
Methods
A retrospective review of all patients who underwent microsurgical breast reconstruction by the senior author (M.Y.N) from July 2005-July 2010 was performed. Patient records were analyzed for risk factors (age, BMI, smoking history, medical history, adjunct therapies, timing of reconstruction, type of reconstruction), and complications (hematoma, seroma, infection, wound dehiscence, pulmonary embolism (PE), deep venous thrombosis (DVT), pneumonia, fat necrosis, leech use, partial flap loss, total flap loss). The specific risk factors studied are listed in Table 1.

Full table
Statistical analysis
The LOGISTIC Procedure of the SAS System (SAS 9.2, Carry, North Carolina) was used to relate the complications (dependent variables) and risk factors (independent variables). We used the STEPWISE option of the LOGISTIC procedure to select the explanatory variables with significant effects. The FREQ procedure of the SAS System was used to generate contingency tables and exact P values if a cell within a contingency table was smaller than 5.
Results
A total of 352 patients underwent 490 microvascular breast reconstructions during the study period. Average patient age was 49.6 years (range, 27-74 years) and average BMI was 27.7 (range, 19.0-47.0). Risk factors and reconstruction data are shown in Table 1. Of 490 reconstructions, 380 were performed in non-smokers, while 25 were performed in active smokers and 85 in former smokers. Twenty four reconstructions were performed in patients with diabetes mellitus, 86 in patients with hypertension, and five in patients with coronary artery disease. Ten reconstructions were performed in patients with connective tissue diseases and 3 in patients on chronic steroids. American Society of Anesthesiologist score (ASA) class distribution included 309 reconstructions that were class 1, 174 that were class 2, and 7 that were class 3. One hundred eighty two reconstructions were performed after chemotherapy and 37 reconstructions were performed prior to chemotherapy. One hundred fifty one reconstructions were performed in the setting of prior irradiation and nine reconstructions were radiated post-operatively. Two hundred forty nine reconstructions were performed in the immediate setting and 241 were performed in a delayed fashion. There were 214 unilateral reconstructions and 138 bilateral reconstructions, 244 left-sided reconstructions and 246 right-sided reconstructions. Distribution of flap type was: 6 MS-0 free TRAM flaps, 42 MS-1 free TRAM flaps, 102 MS-2 free TRAM flaps, 321 deep inferior epigastric perforator flap (DIEP) flaps (223 single perforator, 86 two-perforator, 12 three-plus perforator), and 19 superior gluteal artery perforator flap (SGAP) flaps.
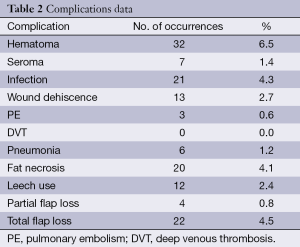
Complications data is listed in Table 2. Complication rates were as follows: hematoma, 6.5%; seroma, 1.4%; infection, 4.3%; wound dehiscence, 2.7%; PE, 0.6%; DVT (without PE), 0%; pneumonia, 1.2%; fat necrosis, 4.1%; leech use, 2.4%; partial flap loss, 0.8%; total flap loss, 4.5%. Donor site complications were not examined in this study. All complications reported were related to the breast/chest.
Full table
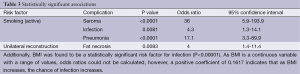
The findings of our statistical analysis are shown in Table 3. Active smoking was found to be a statistically significant risk factor for seroma [P<0.0001; odds ratio (OR) =36; 95% confidence interval (CI), 5.9-193.9], infection (P=0.0081; OR =4.3; 95% CI, 1.3-14.1), and pneumonia (P<0.0001; OR =17.1; 95% CI, 3.3-89.9). Unilateral reconstruction was found to be a statistically significant factor for fat necrosis (P=0.0083; OR =4; 95% CI, 1.4-11.4). Additionally, BMI was found to be a statistically significant risk factor for infection (P<0.00001). As BMI is a continuous variable with a range of values, OR could not be calculated, however, a positive coefficient of 0.1617 indicates that as BMI increases, the chance of infection increases. No other risk factors or reconstructive parameters analyzed were found to have statistically significant associations with any of the complications reviewed.
Full table
Discussion
Despite advancements in microsurgical technique, post-operative complications remain an issue in high-risk patient populations (Figures 1,2,3). In an effort to better understand how certain risk factors impact reconstructive outcomes, microsurgeons have studied these relationships. Our goal was to add to the data on this subject by analyzing the risk factors and complications based on the experience of a single surgeon at a single institution.
Similar to other studies, this study demonstrated that tobacco use and obesity were significant risk factors for postoperative complications. Specifically, active tobacco use was found to increase the risk of flap seroma, infection, and pneumonia. Other groups have identified the impact of smoking on complications in free flap breast reconstruction as well. In a study of 936 free TRAMs in 718 patients, Chang et al. found that smokers had significantly higher rates of abdominal flap necrosis, hernia, and mastectomy flap necrosis compared to former and non-smokers (1). Booi et al. found a statistically significant increase in free TRAM flap complications is smokers compared to non-smokers (P<0.000), and using Laser Doppler flow measurements found that in patients with high flap weights (>800 g), smoking leads to decreased microcirculatory flow, particularly in zone 4 (2). Padubidri et al. identified a 20% rate of fat necrosis in smokers undergoing free TRAM breast reconstruction compared to 10% in non-smokers, however, this was not statistically significant (3). In a study of 569 free TRAMs in 500 patients, Selber et al. found smoking to be a significant risk factor for fat necrosis, wound infection, mastectomy flap necrosis, and abdominal flap necrosis (4). Seidenstuecker et al. identified smoking as a significant risk factor for donor site complications (P=0.007) (5). Looking at 10-year experience of 758 microvascular breast reconstructions led by Allen, an overall complication rate of 30.2% was noted, with higher incidences of breast complications in smokers (P=0.0043), particularly fat necrosis (P=0.0226) (6).
As with smoking, the relationship between obesity and complications has also been well described. We found that as BMI increased, the risk of infection increased. Chang et al. found obese and overweight patients undergoing free TRAM reconstructions had significantly higher total flap loss, flap hematoma, flap seroma, mastectomy skin flap necrosis, donor-site infection, donor-site seroma, and hernia compared with non-obese patients (7). In a study of 612 abdominal flap reconstructions, Jandali et al. found that the morbidly obese (BMI >40) had significantly higher rate of total flap loss (P=0.02), total major postoperative complications (P=0.05), and delayed wound healing of the abdominal incision (P=0.006). Additionally, they identified a linear trend between increasing BMI and increased wound healing complications (8). Selber et al. discovered that obese patients were more likely to have higher rates of mastectomy flap necrosis (P=0.01) and hematoma (P=0.01) (4). In a retrospective review of 1,195 microvascular breast reconstructions in 952 patients, Mehrara et al. found that obesity was a major predictor of complications with obese patients having a statistically significant increased risk of arterial thrombosis (P=0.06; OR =1.7), partial flap loss (P=0.03; OR =2.6), and donor-site complications (P=0.01; OR =3). They also found an association between obesity and fat necrosis (9).
Multiple studies have examined causes for fat necrosis in free flap breast reconstruction. Noted risk factors described, in addition to smoking and obesity, are flap type (10,11), number of perforators (6), and neoadjuvant chemotherapy (9). In our study, unilateral reconstructions were found to be a significant risk factor for the occurrence of fat necrosis compared to bilateral reconstructions. While this association has not been previously described in the literature, it makes good sense. The goal of unilateral reconstruction is to achieve symmetry with the contralateral breast. Sometimes this may require a contralateral reduction mammaplasty but more often than not, a larger flap is used to minimize the need for contralateral surgery. The inclusion of zone 3 of an abdominal flap in unilateral reconstructions, and perhaps even part of zone 4, can push the limits of flap perfusion compared to a hemi-abdominal flap in bilateral reconstructions that by definition include only zones 1 and 2. Careful intra-operative assessment of flap perfusion in unilateral reconstructions can minimize future fat necrosis. Laser-assisted indocyanine green imaging (fluorescent angiography) may be a useful adjunct in assessing flap perfusion, allowing poorly vascularized territories of the flap to be discarded intra-operatively, preventing the inclusion of poorly perfused tissue from evolving into fat necrosis or partial flap loss.
Conclusions
Tobacco use and obesity are well-described risk factors for complications following microvascular breast reconstructions. This study corroborates these findings from previous studies. Tobacco use was demonstrated to be a significant risk factor for infection, seroma, and pneumonia. Obesity was demonstrated to be a significant risk factor for infection. Unilateral reconstruction was demonstrated to pose additional risk for fat necrosis compared to bilateral reconstructions. Patients who choose to have microsurgical breast reconstruction should be informed of the complication profiles associated with certain risk factors. A better understanding of the relationships between these risk factors and complications will allow for better patient counseling, which can provide useful information during the consent process.
Acknowledgements
This study was presented at the 91st Annual Meeting of the American Association of Plastic Surgeons, San Francisco, CA, April 14-17, 2012.
Disclosure: The authors declare no conflict of interest.
References
- Chang DW, Reece GP, Wang B, et al. Effect of smoking on complications in patients undergoing free TRAM flap breast reconstruction. Plast Reconstr Surg 2000;105:2374-80. [PubMed]
- Booi DI, Debats IB, Boeckx WD, et al. Risk factors and blood flow in the free transverse rectus abdominis (TRAM) flap: smoking and high flap weight impair the free TRAM flap microcirculation. Ann Plast Surg 2007;59:364-71. [PubMed]
- Padubidri AN, Yetman R, Browne E, et al. Complications of postmastectomy breast reconstructions in smokers, ex-smokers, and nonsmokers. Plast Reconstr Surg 2001;107:342-9. [PubMed]
- Selber JC, Kurichi JE, Vega SJ, et al. Risk factors and complications in free TRAM flap breast reconstruction. Ann Plast Surg 2006;56:492-7. [PubMed]
- Seidenstuecker K, Munder B, Mahajan AL, et al. Morbidity of microsurgical breast reconstruction in patients with comorbid conditions. Plast Reconstr Surg 2011;127:1086-92. [PubMed]
- Gill PS, Hunt JP, Guerra AB, et al. A 10-year retrospective review of 758 DIEP flaps for breast reconstruction. Plast Reconstr Surg 2004;113:1153-60. [PubMed]
- Chang DW, Wang B, Robb GL, et al. Effect of obesity on flap and donor-site complications in free transverse rectus abdominis myocutaneous flap breast reconstruction. Plast Reconstr Surg 2000;105:1640-8. [PubMed]
- Jandali S, Nelson JA, Sonnad SS, et al. Breast reconstruction with free tissue transfer from the abdomen in the morbidly obese. Plast Reconstr Surg 2011;127:2206-13. [PubMed]
- Mehrara BJ, Santoro TD, Arcilla E, et al. Complications after microvascular breast reconstruction: experience with 1195 flaps. Plast Reconstr Surg 2006;118:1100-9. [PubMed]
- Sailon AM, Schachar JS, Levine JP. Free transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flaps for breast reconstruction: a systematic review of flap complication rates and donor-site morbidity. Ann Plast Surg 2009;62:560-3. [PubMed]
- Kroll SS. Fat necrosis in free transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flaps. Plast Reconstr Surg 2000;106:576-83. [PubMed]





