International oncoplastic breast surgery training
During the past twenty years until recently, medical technology and public awareness on health are emerging developed. Consequently, breast cancer among women can be more early detected with a far more increasing in number of patients around the world.
In developing countries with national screening program, over 50% of breast cancer patients are found in stage 0 and stage I which are basically curable in majority of cases. These breast cancer survivors are seeking their quality of lives after treatment.
In accordance with new technology for earlier breast cancer detection, new procedures are developed to handle those asymptomatic diseases both in diagnostic and therapeutic purposes, such as, stereotactic or ultrasound guided biopsy, needle localization and surgical removal of diseases, etc.
To fulfill the quality of life among survivors, two surgical options are usually advised; that is mastectomy or breast conservation surgery (BCS). In some institutes, BCS are carried out more than 75% of cases. Oncoplastic breast surgery plays more roles to restore the breast shape and symmetry. In addition, wider margins on lumpectomy can be performed without compromising breast deformity (1).
For those who still need mastectomy, immediate total breast reconstruction with autologous tissue flap transfer or implantation or combination of both can be offered (2,3).
Axillary management is still a part of definitive surgery for breast cancer; sentinel lymph node biopsy is routinely performed as initial assessment followed by axillary clearance for positive metastasis (4). The outcome of this approach is promising and could spare more than half of cases from a routine axillary clearance. It reduces the subsequent arm lymphedema in a number of cases as well as shoulder dysfunction from surgery.
With the advance in DNA and gene mutation detection, potentially developed hereditary breast cancer among risk population can be accurately predicted (5,6). As the Angelina Jolie effect, risk reduction surgery in these specific individuals is becoming more popularized. The nipple sparing mastectomy with immediate reconstruction could reduce the individual risk of cancer in over 90% without or minimal impact on the quality of life (7).
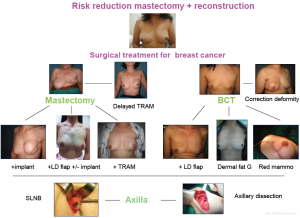
Surgical options both on ablative and reconstructive purpose procedures are more widely performed in different techniques, making the breast cancer surgery becoming an individualized or tailoring surgery (8). Surgeons should instruct the patients on surgical options that are appropriate to their tumor characteristics on presentation, facility of the hospital and surgeon, and patient preference (Figure 1). Multidisciplinary team approach in breast cancer is becoming a standard practice. Surgeons play a major role in local disease control. However, we need to understand and keen on other basic principles in oncology, nature of disease, and be competent on breast imaging and diagnostic procedures as well as radiation therapy and systemic therapy, etc.
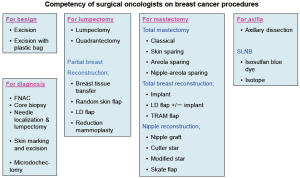
Training in oncoplastic breast surgery will improve the quality of breast cancer patient care. All specialties are keen and well trained with more collaboration. Tumor registration, risk management and quality improvement are all be included as part of the curriculum for better outcome and learning. Apart from competency in surgical procedures (Figure 2), the objectives for trainees will include:
- To understand the principle of oncology and nature of breast cancer;
- To make clinical decision for breast cancer in standard and up to date fashion;
- To participate all varieties of surgical procedure for breast cancer;
- To be familiar with multidisciplinary approach such as radiographic diagnosis, radiation therapy, systemic therapy, cancer epidemiology, patients and family support.
Over the years I have been visited many countries in the regions. The experience has been truly educational and perspective widening. It made me realize that there are huge gaps in our community, not only in economic status but also in the quality and accessibility of health care, especially in surgical problems. There are lots of surgical diseases that are still quite a major problem in one place while quite rare in others. Even in some organ specific cancers, such as breast cancer; the incidence and clinical presentations and cure rates are somewhat totally different, not to mention the facility, technology, quality of service and culture of patient safety, all of which are incomparable in some regions.
Disparities in surgical care are still a major problem. Early detection of breast cancer and public education is a priority concern and should be considered in parallel to the training program. International program should be established to assist other countries with less opportunity. If we consider surgery as being something without boundary, it is about time for us to join hands and solve all these matters together.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Clough KB, Cuminet J, Fitoussi A, et al. Cosmetic sequelae after conservative treatment for breast cancer: classification and results of surgical correction. Ann Plast Surg 1998;41:471-81. [PubMed]
- Bostwick J III. Plastic and reconstructive breast surgery Vol II. St. Louis: Quality Medical Publishing, Inc., 1990.
- Hartrampf CR. Hartrampf’s breast reconstruction with living tissue. Virginia: A Hampton Press publishing, 1991.
- Giuliano AE, Kirgan DM, Guenther JM, et al. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg 1994;220:391-8; discussion 398-401. [PubMed]
- Crook T, Crossland S, Crompton MR, et al. p53 mutations in BRCA1-associated familial breast cancer. Lancet 1997;350:638-9. [PubMed]
- Scully R, Chen J, Plug A, et al. Association of BRCA1 with Rad51 in mitotic and meiotic cells. Cell 1997;88:265-75. [PubMed]
- Hartmann LC, Schaid DJ, Woods JE, et al. Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer. N Engl J Med 1999;340:77-84. [PubMed]
- Carlson G. Tailored Surgery for Early Breast Cancer: Surgical Techniques. In: Martine JP, Hung MC, Solin LJ, et al. eds. Breast Cancer and Molecular Medicine. Berlin Heidelberg: Springer-Verlag, 2006:159-81.