
Thyroidectomy with energy-based devices: surgical outcomes and complications—comparison between Harmonic Focus, LigaSure Small Jaw and Thunderbeat Open Fine Jaw
Introduction
Thyroidectomy is the most performed operation in endocrine surgery. It is widely utilized for the treatment of both benign and malignant thyroid diseases.
Being the thyroid gland a highly vascularized organ, achieving a meticulous hemostasis is essential to avoid serious complications. In this kind of surgery morbidity is mainly represented by lesions of the recurrent laryngeal nerves, hypoparathyroidism and postsurgical cervical hematoma (1-9). An exhaustive hemostasis allows to prevent bleeding in the operating field, allowing an adequate view of the anatomic structures, thus significantly reducing the occurrence of complications. Minimization of morbidity and improvement of surgical outcomes are important not only for the well-being of patients but also for cost-effectiveness.
Traditionally, clamp-and-tie technique, with or without monopolar or bipolar electrocautery, has been used for achieving hemostasis. Subsequently, for the realization of the same purpose, innovative energy-based devices, using different forms of energy, have been introduced. Currently, these instruments are widely used in this kind of surgery. In particular, the most used devices are Harmonic Focus (HF; Ethicon, Johnson and Johnson, Cincinnati, OH, USA), LigaSure Small Jaw (LSJ; Medtronic, Covidien Products, Minneapolis, MN, USA) and Thunderbeat Open Fine Jaw (TB; Olympus, Japan) (1).
HF, using ultrasonic energy, is able to coagulate and dissect tissues at the same time. Ultrasonic waves are generated by electromagnetic energy from a generator which undergoes piezoelectric transduction within the hand piece. The blade of this device vibrates at 55 kHz, producing mechanical energy that breaks hydrogen bonds. This instrument is hand-activated, with cutting and sealing of blood vessels obtained by placing the curved blade in contact with the tissue and applying pressure (1).
LSJ, using advanced bipolar energy, achieves hemostasis by melting elastin and collagen in the vessel wall, reforming them into a permanent plastic-like autologous seal. This device has an activation button with tactile feedback and a 16.5 mm long curved tip which can seal vessels up to 7 mm in diameter. It is capable of cutting with an integrated mechanism. This instrument is suitable both for blunt dissection and for grasping and dividing tissue (1).
TB integrates ultrasonic energy with advanced bipolar. It is composed of an upper bipolar jaw and a lower ultrasonic and bipolar probe which allow to obtain two functional modes: “seal and cut” for vessel sealing and coagulation with simultaneous cutting, “seal” for coagulation alone (1).
The aim of the present study was to compare HF, LSJ and TB in terms of surgical outcomes and complications.
Methods
This is a retrospective study on patients who underwent thyroidectomy in our Unit of General and Endocrine Surgery (University of Cagliari) between January 2012 and June 2018.
Patients were identified from a prospectively maintained institutional database; those with incomplete data were excluded from the study.
Only conventional open total thyroidectomies performed with HF, LSJ and TB by the two most skilled endocrine surgeons of our Unit were considered. Patients simultaneously submitted to lateral and/or central neck dissection, parathyroidectomy or parathyroid autotransplantation were excluded from this study.
Patients were divided into three groups according to the type of energy-device used: those undergoing thyroidectomy with HF were included in Group A, those with LSJ in Group B and those with TB in Group C.
Demographic data (sex, age), histopathological findings, surgical outcomes (operative time, postoperative stay) and complications (recurrent laryngeal nerve injury, hypoparathyroidism, postsurgical cervical hematoma, wound infection) were recorded.
All operations were performed under general anesthesia. Recurrent laryngeal nerves and parathyroid glands were systematically searched and identified. Intraoperative nerve monitoring (IONM) was routinely used in order to facilitate nerve identification and to confirm its functional integrity. One or two closed suction drains were placed below the strap muscles. The cervical linea alba and platysma were sutured with absorbable sutures and skin was closed by a continuous intradermal suture. The duration of the surgical procedure was estimated in minutes from skin incision to skin closure.
Serum calcium and PTH levels were assayed pre- and postoperatively. Postsurgical hypoparathyroidism was defined as PTH <10 pg/mL following the operation (normal range, 10–65 pg/mL). Permanent hypoparathyroidism was defined as PTH concentrations below the normal range for more than 12 months. In case of suspected recurrent laryngeal nerve injury, a fibrolaryngoscopy was performed to assess vocal cord mobility.
Statistical analyses were performed with MedCalc® 18.0.2. Chi-squared test was used for categorical variables and one-way ANOVA test for continuous variables. In case of statistically significant difference with one-way ANOVA test (P value less than the selected significance level), as post-hoc test for all pairwise comparisons, Scheffé’s test was used. P values <0.05 were considered statistically significant.
Results
A total of 2,096 patients underwent thyroidectomy in our Unit within the period considered. Among these, 1,165 met the established inclusion criteria: 1,012 were included in Group A, 96 in Group B and 57 in Group C. Demographic data and histopathological findings were comparable between the three groups, as shown in Table 1.
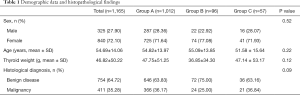
Full table
Surgical outcomes and complications are reported in Table 2.
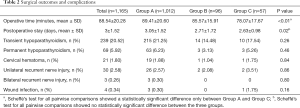
Full table
In Group A, the mean operative time was 89.41±20.60 minutes while the mean postoperative stay was 3.05±1.52 days. About complications, there were 19 (1.88%) cervical hematomas, 26 (2.57%) unilateral recurrent laryngeal nerve lesions, 3 (0.30%) bilateral recurrent laryngeal nerve lesions, 3 (0.30%) wound infections, 215 (21.25%) cases of transient hypoparathyroidism and 63 (6.23%) cases of permanent hypoparathyroidism.
In Group B, the mean operative time was 85.57±15.91 minutes while the mean postoperative stay was 2.71±1.72 days. About complications, there were 1 (1.04%) cervical hematoma, 2 (2.08%) unilateral recurrent laryngeal nerve lesions, 14 (14.48%) cases of transient hypoparathyroidism and 3 (3.13%) cases of permanent hypoparathyroidism. No bilateral recurrent laryngeal nerve injury or wound infection was observed.
In Group C, the mean operative time was 78.07±17.67 minutes while the mean postoperative stay was 2.63±0.98 days. About complications, there were 1 (1.75%) cervical hematoma, 2 (3.51%) unilateral recurrent laryngeal nerve lesions, 1 (1.75%) wound infection, 10 (17.54%) cases of transient hypoparathyroidism and 3 (5.26%) cases of permanent hypoparathyroidism. No bilateral recurrent laryngeal nerve lesion was observed.
The comparison between mean postoperative stays resulted in a statistically significant result (P<0.02). However, the post-hoc test for all pairwise comparisons showed no statistically significant difference between the three groups. Thus, ultimately, the first result was not considered relevant.
The comparison between mean operative times resulted in a statistically significant result (P<0.01). However, the post-hoc test for all pairwise comparisons showed a statistically significant difference only between Group A and Group C. Thus, ultimately, the mean operative time in Group C was significantly shorter than in Group A.
About complications, no statistically significant difference was found between the three groups.
Discussion
Historically, since the earliest surgical attempts, hemostasis has been considered the key point in thyroid surgery. Robert Liston, in 1846, stated that “there was a grave risk of death from haemorrhage during thyroid operations and that it was a proceeding by no means to be thought of”. Shortly after, in 1848, John Dieffenbach described thyroid surgery as “one of the most thankless, most perilous undertakings which, if not altogether prohibited, should at least be restricted”. Thyroid surgery was also condemned by the French Academy of Medicine in 1850. Later, Gross, in 1866, noted that “no sensible man will…attempt to extirpate a goiter of the thyroid gland…every step he takes will be environed with difficulty and every stroke of his knife followed by a torrent of blood and lucky will it be for him if his victims live long. enough to enable him to finish his horrid butchery…”. In the early 1900s, thyroid surgery was profoundly revolutionized by Emil Theodor Kocher. He was the first to use a precise surgical technique and a meticulous hemostasis which have allowed to drastically reduce morbidity and mortality. Currently, a safe and effective hemostasis can be obtained by means of innovative energy-based devices, using different forms of energy (ultrasound, advanced bipolar or both together).
In the literature, several reports comparing HF and/or LSJ with traditional techniques in thyroid surgery exist, however, there are far less studies comparing these two energy-based devices with each other (1,10-20). Moreover, about the use of TB in this kind of surgery, to our knowledge, currently, only one clinical study, which compares this instrument with HF, exists (some other study done on this device in the field of thyroid surgery was performed on porcine models) (21-23). Our study is the first to compare HF, LSJ and TB with each other.
In the literature, a significant reduction in operative times by using HF or LSJ rather than traditional techniques has been described, without increasing complications (1,11,12,15).
In studies comparing HF with LSJ and in that comparing HF with TB, operative times were comparable (10,16,20,21). Differently, in our study the mean operative time was significantly shorter in thyroidectomies performed with TB than in those performed with HF, while no statistically significant difference was found by comparing these two devices with LSJ.
Shorter operative times allow to increase the number of procedures in the same surgical session, optimizing the use of operating rooms and reducing surgery waiting lists. Moreover, the reduction of operative times, as for any surgical procedure, decreases anesthesia costs of every single operation. Ultimately, considering the economic aspect, this gain in terms of time leads to a reduction in the overall costs, thus justifying the cost of each individual device.
However, being patient safety the main purpose, it is important to underline that as regards complications, as also reported in other studies (10,13,14,17,19-21), the three devices were comparable.
This study has three main limitations. First of all, it is based on a retrospective analysis. The second limitation consists in the numerical discrepancy between the three groups, with particular reference to Group A, which is extremely greater than the other two groups. However, despite this condition, the statistical analysis resulted in a statistically significant result as regards operative times. The last limitation is represented by the inhomogeneous use of the three devices within the period considered. While the use of HF covers the whole period considered, that of LSJ and TB is restricted, respectively, to the first years (from 2012 to 2015) and the last years (from 2015 to 2018). In this regard, about operative times, it is important to underline that our result is partially due to the fact that thyroidectomies performed with TB cover only the last years considered in this study, thus benefiting from a greater experience and skill of the two endocrine surgeons.
Conclusions
HF, LSJ and TB have proved to be safe and effective. The postoperative stay and complications were comparable between the three groups. Considering the limits of our investigation, further studies, possibly prospective and with larger population, are needed to investigate the effect of TB on operative times.
Acknowledgments
This work was supported by the Open Access Publishing Fund of the University of Cagliari, with the funding of the Regione Autonoma della Sardegna—L.R. n. 7/2007.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/gs.2020.03.31). PGC serves as an unpaid editorial board member of Gland Surgery from June 2019 to May 2021. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the 1964 Helsinki declaration and its later amendments. Ethical approval was obtained from the local ethics committee (Independent Ethics Committee, University of Cagliari; ID/number: NP/2019/3369).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Materazzi G, Ambrosini CE, Fregoli L, et al. Prevention and management of bleeding in thyroid surgery. Gland Surg 2017;6:510-5. [Crossref] [PubMed]
- Erdas E, Medas F, Podda F, et al. The use of a biologic topical haemostatic agent (TachoSil(®)) for the prevention of postoperative bleeding in patients on antithrombotic therapy undergoing thyroid surgery: a randomised controlled pilot trial. Int J Surg 2015;20:95-100. [Crossref] [PubMed]
- Gambardella C, Polistena A, Sanguinetti A, et al. Unintentional recurrent laryngeal nerve injuries following thyroidectomy: is it the surgeon who pays the bill? Int J Surg. 2017;41 Suppl 1:S55-9. [Crossref] [PubMed]
- Papale F, Cafiero G, Grimaldi A, et al. Galectin-3 expression in thyroid fine needle cytology (t-FNAC) uncertain cases: validation of molecular markers and technology innovation. J Cell Physiol 2013;228:968-74. [Crossref] [PubMed]
- Conzo G, Avenia N, Ansaldo GL, et al. Surgical treatment of thyroid follicular neoplasms: results of a retrospective analysis of a large clinical series. Endocrine 2017;55:530-8. [Crossref] [PubMed]
- Prinzi N, Baldini E, Sorrenti S, et al. Prevalence of breast cancer in thyroid diseases: results of a cross-sectional study of 3,921 patients. Breast Cancer Res Treat 2014;144:683-8. [Crossref] [PubMed]
- Calò PG, Pisano G, Piga G, et al. Postoperative hematomas after thyroid surgery. Incidence and risk factors in our experience. Ann Ital Chir 2010;81:343-7. [PubMed]
- Puzziello A, Rosato L, Innaro N, et al. Hypocalcemia following thyroid surgery: incidence and risk factors. A longitudinal multicenter study comprising 2,631 patients. Endocrine 2014;47:537-42. [Crossref] [PubMed]
- Calò PG, Erdas E, Medas F, et al. Late bleeding after total thyroidectomy: report of two cases occurring 13 days after operation. Clin Med Insights Case Rep 2013;6:165-70. [Crossref] [PubMed]
- Hwang SO, Jung JH, Park HY, et al. A prospective, randomized study between the Small Jaw® and the Harmonic Focus® in open thyroidectomy. Otolaryngol Head Neck Surg 2014;150:943-8. [Crossref] [PubMed]
- Calò PG, Pisano G, Medas F, et al. The use of the harmonic scalpel in thyroid surgery. Our experience. Ann Ital Chir 2012;83:7-12. [PubMed]
- Ramouz A, Rasihashemi SZ, Safaeiyan A, et al. Comparing postoperative complication of LigaSure Small Jaw instrument with clamp and tie method in thyroidectomy patients: a randomized controlled trial World J Surg Oncol 2018;16:154. [IRCT2014010516077N1]. [Crossref] [PubMed]
- Ruggiero R, Docimo G, Bosco A, et al. Update on sutureless thyroidectomy. G Chir 2018;39:45-50. [Crossref] [PubMed]
- Ruggiero R, Gubitosi A, Conzo G, et al. Sutureless thyroidectomy. Int J Surg 2014;12 Suppl 1:S189-93. [Crossref] [PubMed]
- Revelli L, Damiani G, Bianchi CB, et al. Complications in thyroid surgery. Harmonic Scalpel, Harmonic Focus versus Conventional Hemostasis: a meta-analysis. Int J Surg 2016;28 Suppl 1:S22-32. [Crossref] [PubMed]
- Hammad AY, Deniwar A, Al-Qurayshi Z, et al. A prospective study comparing the efficacy and surgical outcomes of Harmonic Focus Scalpel Versus LigaSure Small Jaw in thyroid and parathyroid surgery. Surg Innov 2016;23:486-9. [Crossref] [PubMed]
- Upadhyaya A, Hu T, Meng Z, et al. Harmonic versus LigaSure hemostasis technique in thyroid surgery: a meta-analysis. Biomed Rep 2016;5:221-7. [Crossref] [PubMed]
- Luo Y, Li X, Dong J, et al. A comparison of surgical outcomes and complications between hemostatic devices for thyroid surgery: a network meta-analysis. Eur Arch Otorhinolaryngol 2017;274:1269-78. [Crossref] [PubMed]
- Teksoz S, Bukey Y, Ozcan M, et al. Sutureless thyroidectomy with energy-based devices: Cerrahpasa experience. Updates Surg 2013;65:301-7. [Crossref] [PubMed]
- Dionigi G, Boni L, Rausei S, et al. The safety of energy-based devices in open thyroidectomy: a prospective, randomised study comparing the LigaSure™ (LF1212) and the Harmonic® FOCUS. Langenbecks Arch Surg 2012;397:817-23. [Crossref] [PubMed]
- Van Slycke S, Gillardin JP, Van Den Heede K, et al. Comparison of the harmonic focus and the thunderbeat for open thyroidectomy. Langenbecks Arch Surg 2016;401:851-9. [Crossref] [PubMed]
- Tamura A, Tsutsui H, Yano Y, et al. Thermal effects of the Thunderbeat™ device on the recurrent laryngeal nerve during thyroid surgery. Surg Today 2018;48:1076-80. [Crossref] [PubMed]
- Kwak HY, Dionigi G, Kim D, et al. Thermal injury of the recurrent laryngeal nerve by THUNDERBEAT during thyroid surgery: findings from continuous intraoperative neuromonitoring in a porcine model. J Surg Res 2016;200:177-82. [Crossref] [PubMed]


