
Minimally invasive video-assisted thyroidectomy (MIVAT)
Introduction
Minimally invasive video-assisted thyroidectomy (MIVAT) was first described in 1999 (1) and it has become a widespread technique performed worldwide (2). Although initially limited to benign thyroid nodules, MIVAT was progressively adopted for all types of thyroid diseases, even low- and intermediate-risk differentiated thyroid tumor, while remaining within the selection criteria. MIVAT is a procedure performed partly under endoscopic view (with the benefit of a magnified vision) and partly under direct vision. Magnified vision enables an easier identification of the noble structures allocated in the narrow space of the neck (recurrent laryngeal nerve, external branch of superior laryngeal nerve, parathyroid gland) (3). Further, advantages of this technique are represented by a small cervical incision (about 1.5 cm), faster recovery, better voice quality and decreased post-operative pain which translate in superior patient satisfaction. On the other hand, several studies assessed that MIVAT is comparable to the standard open thyroidectomy (SOT) in terms of oncologic radicality, time, costs and complications rate (4,5).
Methods
The authors conducted a retrospective analysis about patients who underwent MIVAT between 1998 and 2019 in the Endocrine Surgery Unit of the University Hospital in Pisa.
Data were collected and scrutinized. Written informed consent was obtained from the patients or from their relatives, according to the ethical guidelines.
Surgical technique
The access to the thyroid anatomical space used in MIVAT was initially described when proposing the first gasless procedure to operate on parathyroid adenomas and, once standardized, it did not change basically (6). The operation starts with an incision of about 1.5 cm above the sternal notch. Using two retractors the alba line is exposed and opened for 2–3 cm. The endoscopic phase of the surgery begins with the introducing of a 5-mm 30° degrees endoscope. We proceed with the dissection of the thyroid lobe from the pre-thyroid muscles using an atraumatic endoscopic spatula. The thyroid lobe is then pulled caudally and the upper pedicle is isolated by blunt dissection. Follow the cutting of the upper pedicle using an ultrasound dissector. We prefer the last generation Sonicision for its limited size (5 mm) and high power of coagulation. The thyroid lobe is pulled medially and the recurrent laryngeal nerve is identified using the Tuberculum of Zuckerkandl as landmark. Visualization and preservation of the two parathyroid glands and the noble structures located in the neck is easy due to the magnified vision; our attitude is to follow and dissect the nerve high until the point where it bends medially to reach the larynx. At this point, the thyroid lobe can be retrieved through the small cervical incision and the following steps are basically the same as in SOT, starting from the division of the isthmus in a downward direction. The last step is the transection of the lobe at the Berry ligament level. In this phase of the operation, we prefer to use clips rather than energy devices to close the small vessels that are generally very near to the recurrent laryngeal nerve. We never put any drain in the neck. The wound is close just approaching each other the strap muscles in the midline and then a short subcuticular running suture is performed. For the skin, sealant glue is used in order to have the best cosmetic result in terms of scar.
Indications and contraindications
Surgeons must be aware that MIVAT cannot be viable for any patient. The indications are reserved to a minority of cases: in our experience, around 20% of all cases. In the United States though the number can increase up to 30% according to some papers reporting on the experience in this country (4,7).
In our experience, the following indications have to be mostly supported by a good ultrasound evaluation before choosing the endoscopic approach in order to select really adequate candidates for MIVAT:
- Nodule size not exceeding 35 mm in its largest diameter.
- Total thyroid volume not exceeding 25 cc as measured by ultrasound.
- The presence of enlarged lymph nodes in the central compartment of the neck is not necessarily a contraindication since MIVAT proved to be fit even for VIth level lymphadenectomy; on the other hand, the presence of metastatic or suspicious lymph-nodes in the lateral neck compartment represents an absolute contraindication in our center.
- Caution must be taken towards some small low risk thyroid cancers when located very posteriorly because they could have an extracapsular infiltration: this situation could represent a reason for a prompt conversion to SOT.
- Pre-operative ultrasound could raise the suspicion of a thyroiditis: in this case a dosage of antibodies could either confirm or exclude the presence of this generally auto-immune disease. It is important to stress again that thyroiditis can make quite complicate a correct dissection by the surgeon.
For the evaluation of these factors, we tend to consider a good and accurate pre-operative ultrasound as an element of paramount importance.
Results
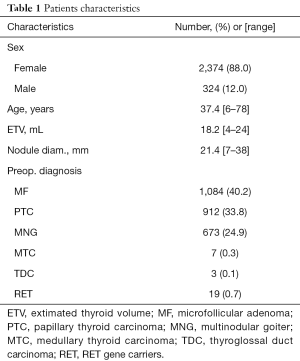
From 1998 to 2019 a total of 2,698 patients underwent MIVAT in the Endocrine Surgery Unit of the University Hospital in Pisa; 2,374 patients (88%) were female, whereas 324 patients (12%) were male, with a mean age of 37.4 years. Mean estimated thyroid volume (calculated preoperatively at US) was 18.2 mL and the mean diameter of the largest nodule of each goiter was 21.4 mm. Total thyroidectomy was performed in 1,862 cases (69%) and hemithyroidectomy was performed in 763 cases (28.2%). A small number of patients (31, 1.2%) underwent total thyroidectomy and lymphadenectomy of the central neck compartment, whereas in 42 cases (1.6%) parathyroidectomy was performed together with total thyroidectomy for simultaneous primary hyperparathyroidism (PHPT).
The preoperative diagnosis was in 1,084 patients (40.2%) an indeterminate nodule Thy3, whereas in 912 cases (33.8%) the diagnosis was a low- or intermediate-risk differentiated thyroid carcinoma. In 7 cases (0.3%) the procedure was performed for medullary thyroid carcinoma and in only 3 cases (0.1%) for carcinoma of the thyroglossal duct. Nineteen patients (0.7%) deserve a special mention since they were RET gene mutation carriers and underwent MIVAT for a prophylactic purpose. In 673 cases (24.9%) the indication was a small multinodular goiter, of which 166 cases (6.2%) with associated hyperthyroidism (Table 1).
Full table
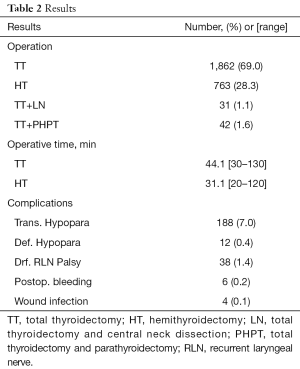
Mean operative time was 44.1 minutes (ranging from 30 to 130 minutes) for total thyroidectomy and 31.1 minutes (ranging from 20 to 120 minutes) for hemithyroidectomy. Conversion occurred in 43 cases (1.6%), mainly at the beginning of the experience. In 188 cases (7%) a postoperative transient hypoparathyroidism was reported, whereas definitive hypoparathyroidism was reported in 12 cases (0.4%). Thirty-eight patients (1.4%) suffered from a definitive postoperative recurrent laryngeal nerve palsy. No definitive bilateral recurrent laryngeal nerve palsy occurred. Six patients (0.2%) required re-intervention because of postoperative bleeding and four patients (0.1%) reported a wound infection (Table 2).
Full table
Discussion
It is widely reported in literature that MIVAT is a safe and effective procedure for thyroidectomy in selected cases. Although initially used only for benign nodules, indications spread during years and nowadays it is broadly demonstrated that MIVAT can be performed safety in selected patients with Grave’s disease or malignant nodules, in particular for low- and intermediate-risk differentiated thyroid carcinoma (8). In our casuistry, low- or intermediate-risk differentiated thyroid carcinomas plays, along with indeterminate nodules, a main role (33.8% and 40%, respectively). It is well known that, in selected cases, the oncologic outcomes of MIVAT is comparable to SOT; in our previous published study, we demonstrate that in patients with a low- or intermediate-risk differentiated thyroid carcinoma post-operative thyroglobulin serum levels shows optimal results. Further, even for patients carriers of gene RET mutation who underwent prophylactic thyroidectomy with MIVAT technique, post-operative calcitonin serum levels confirm excellent results (5).
In spite of having been described 20 years ago, this procedure still remains one of the favorite endoscopic procedures to remove the thyroid gland (7). An imposing number of different approaches which can avoid or reduce the extension of a neck scar were described in the meanwhile, often expressing different habits and expectations by both surgeons and patients in different geographical and cultural backgrounds (9). Anyway, several critical limitations inherent of these techniques restrict their spreading, such as poor results, technical limits, invasiveness, length of recovery, lack of standardization, rejection for scientific communities, costs, whereas MIVAT still keep being a safe and effective procedure for thyroidectomy, in selected cases (2,9).
Among the advantage of MIVAT, literature is almost unanimous in claiming that this technique leads to a better cosmetic result and to a reduced post-operative pain with consequent reduction of analgesic drugs administration (10-12). On the other hand, regarding complications, several studies dealing with MIVAT reported data comparable to SOT, strengthening the idea that this is a safe technique (13,14). In our casuistry, transient hypoparathyroidism was reported in 7% of cases, whereas definitive hypoparathyroidism in 0.4%; definitive unilateral recurrent laryngeal nerve palsy was 1.4%, whereas no definitive bilateral recurrent laryngeal nerve palsy occurred. Although the narrow space and the few degrees of freedom, these outcomes can be achieved thanks to the magnified vision of the endoscope which allows an easy identification of parathyroid glands and recurrent laryngeal nerves (3). Conversion rate it is reported to be very low (15), and so it is shown in our casuistry (1.4%): these cases are mainly referred to the beginning of our experience.
With respect to the costs, MIVAT is superimposable to standard open thyroidectomy (16,17). Indeed, basically most of surgical instrument used are the same both for MIVAT than for SOT, and, nowadays, every operating theater is provided by a laparoscopic column and a 30° endoscope (15). Further, this technique was surrounded by lot of doubts regarding operative time and learning curve: the concerns were overcame thanks a lot of studies which demonstrate that MIVAT is easier and faster to learn compare to other endoscopic procedures and that operative time was not statistically different to that of SOT after an adequate training (5,13). We believe that, for surgeons skilled in neck surgery, MIVAT can be learned quite quickly with an adequate enrollment of patients.
Conclusions
From our multi-years’ experience which spreads over 20 years, we can reaffirm the concept that MIVAT is a safe procedure which is not burdened by an increase complications rate (compared with any other approach, both traditional and endoscopic) or additional costs. Furthermore, this technique offers advantages in terms of cosmetic results and post-operative pain. To date, the indications and above all contraindications for this operation (but also for other endoscopic approaches) remained the same throughout the last 20 years, and this witnesses the robustness of the anatomical and physiopathological fundamentals of this surgery. MIVAT represents a valid option to SOT also in cases of low- and intermediate-risk differentiated thyroid carcinomas with excellent oncologic outcomes.
It is true that it still needs a consistent learning curve but it is our opinion that any endocrine surgeon quite confident with neck anatomy and with the use of the endoscope can approach it safely.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the XXXXXXXXX (No. XXXX). Written informed consent was obtained from the patients or from their relatives, according to the ethical guidelines.
References
- Miccoli P, Berti P, Conte M, et al. Minimally invasive surgery for thyroid small nodules: preliminary report. J Endocrinol Invest 1999;22:849-51. [Crossref] [PubMed]
- Scerrino G, Melfa G, Raspanti C, et al. Minimally Invasive Video-Assisted Thyroidectomy: Analysis of Complications From a Systematic Review. Surg Innov 2019;26:381-7. [Crossref] [PubMed]
- Berti P, Materazzi G, Conte M, et al. Visualization of the external branch of the superior laryngeal nerve during video-assisted thyroidectomy. J Am Coll Surg 2002;195:573-4. [Crossref] [PubMed]
- Lai SY, Walvekar RR, Ferris RL. Minimally invasive video-assisted thyroidectomy: expanded indications and oncologic completeness. Head Neck 2008;30:1403-7. [Crossref] [PubMed]
- Miccoli P, Biricotti M, Matteucci V, et al. Minimally invasive video-assisted thyroidectomy: reflections after more than 2400 cases performed. Surg Endosc 2016;30:2489-95. [Crossref] [PubMed]
- Miccoli P, Bendinelli C, Conte M, et al. Endoscopic parathyroidectomy by a gasless approach. J Laparoendosc Adv Surg Tech A 1998;8:189-94. [Crossref] [PubMed]
- Terris DJ, Angelos P, Steward DL, Simental AA. Minimally invasive video-assisted thyroidectomy: a multi-institutional North American experience. Arch Otolaryngol Head Neck Surg 2008;134:81-4. [Crossref] [PubMed]
- Kania R, Kania R, Hammami H, et al. Minimally invasive video-assisted thyroidectomy: tips and pearls for the surgical technique. Ann Otol Rhinol Laryngol 2014;123:409-14. [Crossref] [PubMed]
- Dionigi G. Evidence-based review series on endoscopic thyroidectomy: real progress and future trends. World J Surg 2009;33:365-6. [Crossref] [PubMed]
- Miccoli P, Rago R, Massi M, et al. Standard versus video-assisted thyroidectomy: objective postoperative pain evaluation. Surg Endosc 2010;24:2415-7. [Crossref] [PubMed]
- Lombardi CP, Carnassale G, D'Amore A, et al. Morbidity from minimally invasive video-assisted thyroidectomy: a general review. Gland Surg 2017;6:488-91. [Crossref] [PubMed]
- Dralle H, Machens A, Thanh PN. Minimally invasive compared with conventional thyroidectomy for nodular goitre. Best Pract Res Clin Endocrinol Metab 2014;28:589-99. [Crossref] [PubMed]
- Capponi MG, Bellotti C, Lotti M, et al. Minimally invasive video-assisted thyroidectomy: Ascending the learning curve. J Minim Access Surg 2015;11:119-22. [Crossref] [PubMed]
- Pons Y, Vérillaud B, Blancal JP, et al. Minimally invasive video-assisted thyroidectomy: Learning curve in terms of mean operative time and conversion and complication rates. Head Neck 2013;35:1078-82. [Crossref] [PubMed]
- Bellotti C, Capponi MG, Cinquepalmi M, et al. MIVAT: the last 2 years experience, tips and techniques after more than 10 years. Surg Endosc 2018;32:2340-4. [Crossref] [PubMed]
- Byrd JK, Nguyen SA, Ketcham A, et al. Minimally invasive video-assisted thyroidectomy versus conventional thyroidectomy: a cost-effective analysis. Otolaryngol Head Neck Surg 2010;143:789-94. [Crossref] [PubMed]
- Del Rio P, Viani L, Montana CM, et al. Minimally invasive thyroidectomy: a ten years experience. Gland Surg 2016;5:295-9. [Crossref] [PubMed]


