A systematic review of patient reported outcome measures for women with macromastia who have undergone breast reduction surgery
Introduction
Reduction mammoplasty is one of the most common breast operations performed. The cosmetic and psychological impacts of macromastia include being unable to find fitting clothes and low self-esteem. The motivation for surgery is commonly for resolution of physical symptoms caused by the heaviness and size of breasts such as back, neck and shoulder pain, intertrigo and shoulder grooving by bra straps (1).
Patient reported outcome measure (PROM) questionnaires that assess patient perceptions of reduction mammaplasty surgery and satisfy accepted health measurement criteria are needed. They can provide quantitative data to support government funding for reduction mammoplasty, aid surgeons in seeking to improve outcomes in their own practice and evaluate techniques.
The primary aim of this systematic review was to assess whether reduction mammaplasty is associated with measurable patient benefit and the secondary aim was to find which PROM questionnaire best evaluates patient satisfaction.
Methods
This review adheres to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (2).
Search strategy
An electronic literature review was conducted using the PubMed, Cochrane, SCOPUS and Medline databases for publications dated from 1966 to July 2018. Initial searches using the following MeSH terms were used: (“breast reduction” OR “reduction mammaplasty”) AND (“treatment outcome” OR “personal satisfaction” OR “outcome assessment” OR “quality of life” OR “quality-of-life” OR “questionnaire” OR “outcome” OR “satisfaction” OR “instrument” OR “survey” OR “assessment”).
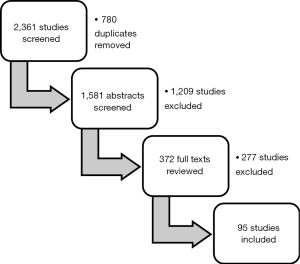
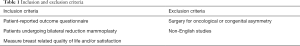
Once the search results were obtained, duplicate articles were removed. If authors/groups with multiple papers on the same topic existed, we then included the most recent study to avoid duplication of cases being analysed. A review of titles, abstracts and/or full article details were then reviewed by two authors (SL, RS) in order to determine article suitability, according to inclusion criteria. The predetermined inclusion criteria were articles which addressed bilateral reduction mammoplasty (not symmetrising or post-cancer) and reported patient satisfaction or quality of life based on outcome questionnaires (Table 1). The search results were further restricted to English language articles only. A graphic representation of the search strategy is summarized below (Figure 1).
Full table
Statistical analysis
Data was extracted from each study pertaining to demographics, questionnaire used, surgical technique and satisfaction including components of physical, psychological and functional outcomes.
Results
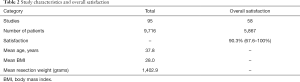
While the search yielded 2,361 studies, only 95 met the inclusion criteria (3-27), representing 9,716 patients (28-51) as summarized in Table 2 (52-76). Overall, the mean age was 37.8 years, body mass index (BMI) 28.0, and combined tissue resection mass was 1,402.9 g (77-96). Fifty-eight (4,5,9-31) studies listed overall satisfaction (33-39,41,42,44-47,49,51-57,59,60) as primary endpoint, including 5,867 patients (64-67,77,79,82,84,90,92). Grouped data found overall satisfaction to be 90.3% (range, 67.6–100%).
Full table
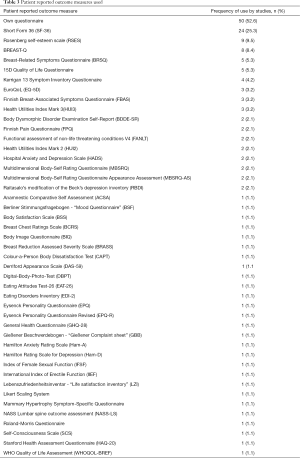
Unvalidated PROM questionnaires used most commonly were individually developed by research groups (52.6%). Of validated questionnaires used, most commonly was the Short Form 36 (SF-36) (25.3%) (6-8,20,23,24,31,33,34,42,43,48,50,55,61-63,69,73,79,91-93), followed by the Rosenberg self-esteem scale (RSES) (9.5%) (23,42,48,50,55,61,62,76,79), then BREAST-Q (8.4%) (17,22,25,30,39,57,70) (Table 3).
Full table
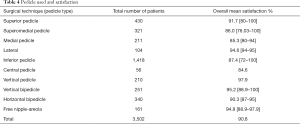
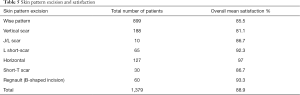
Grouped data found the most commonly used pedicle was inferior (1,418 cases) associated with overall satisfaction of 87.4% (Table 4). Vertical pedicle, used in 210 cases, was associated with highest satisfaction (97.9%). In terms of skin excision pattern, wise pattern was most commonly used, with mean overall satisfaction of 85.5% (Table 5). Horizontal scar [no vertical scar (45)] technique was associated with highest satisfaction (97%).
Full table
Full table
All studies using BREAST-Q reported satisfaction and improvements in physical and psychological quality of life (17,22,25,30,39,57,70). Reported satisfaction ranged from 76.0% to 95.0%. Reported relative rates of improved physical quality of life ranged from 48.15% to 90.61%. Reported absolute rates of improved psychological quality of life ranged from 76.37% to 84.54%.
Studies using the RSES reported improvements in self-esteem with rates between 12.9% to 17.9% (23,42,48,50,55,61,62,76,79).
All studies using the SF-36 reported improvement in bodily pain with rates between 22.34% to 83.33% (6-8,20,23,24,31,33,34,42,43,48,50,55,61-63,69,73,79,91-93). They reported improvement in physical quality of life by 10.38% to 33.24% and psychological quality of life by 3.33% to 33%.
Discussion
Our findings show that the vast majority of patients were happy with their breast reduction procedure, with an overall satisfaction rate of 90.3% amongst patients whose satisfaction was directly measured. While the most common techniques are inferior pedicle and wise-pattern skin resection, highest satisfaction was found with vertical pedicle and horizontal scar; however, these were small sample groups. Regardless of technique, it appears that the cosmetic and physical benefits of reduction mammoplasty are universal.
Despite the plethora of information-seeking methods utilized, the results of our analysis clearly showed that patients felt an overall improvement in their quality of life after breast reduction compared to before. In almost all studies, patients reported improvements in the vast majority of premorbid symptoms, a finding consistent with previous reviews of this subject (97). Other studies have also found that breast reduction had positive effects on depression and sexual function (98), as well as led to a significant improvement in lung function tests with a positive correlation between amount of breast tissue resected and improvement in expiratory capacity (99).
A wide range of questionnaires were captured in the studies investigated in this systematic review. Over half utilized unvalidated surveys, focusing on aspects of patient outcomes specific to their study. In the remaining studies, the SF-36 was used most frequently, followed by the RSES and BREAST-Q. There is significant overlap between these surveys in terms of information sought; both SF-36 and BREAST-Q focus on general physical and psychosocial health, with RSES providing additional questions pertaining to the latter. BREAST-Q also focuses on breast-specific details such as the appearance of their breasts as well as the patients’ satisfaction with the procedure and the care they received from their healthcare providers and team (100-102). While it is difficult to say which questionnaire is best suited to a particular research question, it appears that those that cover a wide range of factors involved in determining quality of life were most often used, and can be useful when added to a breast-specific questionnaire to determine factors directly affected by the surgery. Most studies used more than one questionnaire and combinations, such as the use of SF-36 and BREAST-Q offers a broad assessment of patient outcomes in terms of physical, psychological and breast symptoms.In terms of timing of assessment of patient satisfaction, studies have shown no significant differences in PROM scores at time points of less or greater than 3 months post-operatively (103). It has previously been demonstrated that patients have sharp improvement in quality of life in the immediate post-operative period when experiencing the immediate relief of physical loss of breast weight (25). Patients continue to show satisfaction in the following months as they benefit both physically and psychologically from the surgery once the healing process is completed.This study has a number of strengths, including a comprehensive search strategy encompassing multiple major medical databases, which increases the likelihood that our systematic review included as many relevant articles as possible. The large number of studies we identified led us to be able to appreciate trends and formulate robust conclusions from the presented data. Duplicate author screening and selection of articles ensured that as many relevant articles as possible were included and a comprehensive data extraction process, performed by two authors, aimed to reduce chance of error and bias.Limitations to our study included somewhat heterogeneous questionnaire use and variable target outcomes, which made it more difficult to combine and interpret data. A significant portion of patients in some studies was also lost to follow up, possibly introducing bias to the results; for instance, patients who had no issues with their surgery may not have bothered to provide feedback. Nevertheless, we covered a broad range of patient outcomes and almost all studies reported on patient satisfaction with their breast reduction procedure, which was our major focus.
Conclusions
Reduction mammoplasty led to higher PROM scores compared to before the procedure, which is consistent with previous studies. Patients noted improvements in both physical and mental health. PROM questionnaires that address multiple aspects of health appear to be preferred by most authors. When combined with breast-specific questions, validated PROMs may provide a more accurate assessment of pre- and post-operative quality of life.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Schnur PL, Hoehn JG, Ilstrop D, et al. Reduction mammoplasty: Cosmetic or Reconstructive Procedure? Ann Plast Surg 1991;27:232. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 2009;6:e1000097. [Crossref] [PubMed]
- Adham M, Sawan K, Lovelace C, et al. Patient Satisfaction with Vertical Reduction Mammaplasty: Part I. Aesthet Surg J 2010;30:814-20. [Crossref] [PubMed]
- Agbenorku P, Agamah G, Agbenorku M, et al. Reduction Mammaplasty in a Developing Country: A Guideline for Plastic Surgeons for Patient Selection. Aesthetic Plast Surg 2012;36:91-6. [Crossref] [PubMed]
- Atterhem H, Holmner S, Janson PE. Reduction mammaplasty: Symptoms, complications, and late results - A retrospective study on 242 patients. Scand J Plast Reconstr Surg Hand Surg 1998;32:281-6. [Crossref] [PubMed]
- Behmand RA, Tang DH, Smith DJ. Outcomes in breast reduction surgery. Ann Plast Surg 2000;45:575-80. [Crossref] [PubMed]
- Blomqvist L, Brandberg Y. Three-year follow-up on clinical symptoms and health-related quality of life after reduction mammaplasty. Plast Reconstr Surg 2004;114:49-54. [Crossref] [PubMed]
- Blomqvist L, Eriksson A, Brandberg Y. Reduction mammaplasty provides long-term improvement in health status and quality of life. Plast Reconstr Surg 2000;106:991-7. [Crossref] [PubMed]
- Borkenhagen A, Rohricht F, Preiss S, et al. Changes in body image and health-related quality of life following breast reduction surgery in German macromastia patients - A new tool for measuring body image changes. Ann Plast Surg 2007;58:364-70. [Crossref] [PubMed]
- Boschert MT, Barone CM, Puckett CL. Outcome analysis of reduction mammaplasty. Plast Reconstr Surg 1996;98:451-4. [Crossref] [PubMed]
- Bouwer LR, van der Biezen JJ, Spronk CA, et al. Vertical scar versus the inverted-T scar reduction mammaplasty: A 10-year follow-up. J Plast Reconstr Aesthet Surg 2012;65:1298-304. [Crossref] [PubMed]
- Braig D, Eisenhardt SU, Stark GB, et al. Impact of increasing age on breast reduction surgery: A single centre analysis. J Plast Reconstr Aesthet Surg 2016;69:482-6. [Crossref] [PubMed]
- Breiting LB, Henriksen TF, Kalialis LV, et al. A Prospective Study of Short- and Long-Term Cosmetic Outcome after Reduction Mammaplasty from Three Different Perspectives: The Patient, a Department Surgeon, and an Independent Private Practitioner in Plastic Surgery. Plast Reconstr Surg 2012;130:273-81. [Crossref] [PubMed]
- Brown AP, Hill C, Khan K. Outcome of reduction mammaplasty--a patients' perspective. Br J Plast Surg 2000;53:584-7. [Crossref] [PubMed]
- Brown JR, Holton LH, Chung TL, et al. Breast-feeding, self-exam, and exercise practices before and after reduction mammoplasty. Ann Plast Surg 2008;61:375-9. [Crossref] [PubMed]
- Brühlmann Y, Tschopp H. Breast reduction improves symptoms of macromastia and has a long-lasting effect. Ann Plast Surg 1998;41:240-5. [Crossref] [PubMed]
- Cabral IV, Garcia ED, Neponucena R, et al. Use of the BREAST-Q (TM) Survey in the Prospective Evaluation of Reduction Mammaplasty Outcomes. Aesthetic Plast Surg 2018;42:388-95. [Crossref] [PubMed]
- Cerovac S, Ali FS, Blizard R, et al. Psychosexual function in women who have undergone reduction mammaplasty. Plast Reconstr Surg 2005;116:1306-13. [Crossref] [PubMed]
- Chalekson CP, Neumeister MW, Zook EG, et al. Outcome analysis of reduction mammaplasty using the modified Robertson technique. Plast Reconstr Surg 2002;110:71-9. [Crossref] [PubMed]
- Iwuagwu OC, Walker LG, Stanley PW, et al. Randomized clinical trial examining psychosocial and quality of life benefits of bilateral breast reduction surgery. Br J Surg 2006;93:291-4. [Crossref] [PubMed]
- Chao JD, Memmel HC, Redding JF, et al. Reduction mammaplasty is a functional operation, improving quality of life in symptomatic women: A prospective, single-center breast reduction outcome study. Plast Reconstr Surg 2002;110:1644-52. [Crossref] [PubMed]
- Cogliandro A, Barone M, Cassotta G, et al. Patient Satisfaction and Clinical Outcomes Following 414 Breast Reductions: Application of BREAST-Q. Aesthetic Plast Surg 2017;41:245-9. [Crossref] [PubMed]
- Cole RP, Shakespeare V. Measuring patient-based outcomes in a plastic surgery service: breast reduction surgical patients. Br J Plast Surg 1998;51:79-80. [Crossref] [PubMed]
- Collins ED, Kerrigan CL, Kim M, et al. The effectiveness of surgical and nonsurgical interventions in relieving the symptoms of macromastia. Plast Reconstr Surg 2002;109:1556-66. [Crossref] [PubMed]
- Coriddi M, Nadeau M, Taghizadeh M, et al. Analysis of Satisfaction and Well-Being following Breast Reduction Using a Validated Survey Instrument: The BREAST-Q. Plast Reconstr Surg 2013;132:285-90. [Crossref] [PubMed]
- Corrêa MPD, Dornelas MT, de Carvalho EN, et al. Assessment of quality of life in patients who underwent breast reduction using BREAST-Q. J Plast Reconstr Aesthet Surg 2018;71:929-31. [Crossref] [PubMed]
- Cruz-Korchin N, Korchin L. Vertical versus wise pattern breast reduction: Patient satisfaction, revision rates, and complications. Plast Reconstr Surg 2003;112:1573-8. [Crossref] [PubMed]
- Dabbah A, Lehman JA, Parker MG, et al. Reduction mammaplasty - an outcome analysis. Ann Plast Surg 1995;35:337-41. [Crossref] [PubMed]
- Davis GM, Ringler SL, Short K, et al. Reduction mammaplasty - long-term efficacy, morbidity, and patient satisfaction. Plast Reconstr Surg 1995;96:1106-10. [Crossref] [PubMed]
- Derby BM, Grotting JC, Redden DT. Vertical Sculpted Pillar Reduction Mammaplasty in 317 Patients: Technique, Complications, and BREAST-Q Outcomes. Aesthet Surg J 2016;36:417-30. [Crossref] [PubMed]
- Eggert E, Schuss R, Edsander-Nord A. Clinical outcome, quality of life, patients' satisfaction, and aesthetic results, after reduction mammaplasty. Scand J Plast Reconstr Surg Hand Surg 2009;43:201-6. [Crossref] [PubMed]
- Emami SA, Sobhani R. Impact of reduction mammaplasty on sexuality in patients with macromastia and their partners. J Plast Reconstr Aesthet Surg 2016;69:1335-9. [Crossref] [PubMed]
- Faria FS, Guthrie E, Bradbury E, et al. Psychosocial outcome and patient satisfaction following breast reduction surgery. Br J Plast Surg 1999;52:448-52. [Crossref] [PubMed]
- Freire M, Neto MS, Garcia EB, et al. Quality of life after reduction mammaplasty. Scand J Plast Reconstr Surg Hand Surg 2004;38:335-9. [Crossref] [PubMed]
- Freire M, Neto MS, Garcia EB, et al. Functional capacity and postural pain outcomes after reduction mammaplasty. Plast Reconstr Surg 2007;119:1149-56. [Crossref] [PubMed]
- Glatt BS, Sarwer DB, O'Hara DE, et al. A retrospective study of changes in physical symptoms and body image after reduction mammaplasty. Plast Reconstr Surg 1999;103:76-82. [Crossref] [PubMed]
- Godwin Y, Barron EJ, Edmunds MC, et al. A comparison of the patient and surgeon opinion on the long-term aesthetic outcome of reduction mammaplasty: Have we improved over 15 years? J Plast Reconstr Aesthet Surg 2014;67:932-8. [Crossref] [PubMed]
- Godwin Y, Wood SH, O'Neill TJ. A comparison of the patient and surgeon opinion on the long-term aesthetic outcome of reduction mammaplasty. Br J Plast Surg 1998;51:444-9. [Crossref] [PubMed]
- Gonzalez MA, Glickman LT, Aladegbami B, et al. Quality of Life After Breast Reduction Surgery: A 10-Year Retrospective Analysis Using the Breast Q Questionnaire Does Breast Size Matter? Ann Plast Surg 2012;69:361-3. [Crossref] [PubMed]
- Spector JA, Kleinerman R, Culliford AT 4th, et al. The vertical reduction mammaplasty: A prospective analysis of patient outcomes. Plast Reconstr Surg 2006;117:374-81; discussion 382-3. [Crossref] [PubMed]
- Hang-Fu L. Subjective comparison of six different reduction mammoplasty procedures. Aesthetic Plast Surg 1991;15:297-302. [Crossref] [PubMed]
- Hermans BJE, Boeckx WD, De Lorenzi F, et al. Quality of life after breast reduction. Ann Plast Surg 2005;55:227-31. [Crossref] [PubMed]
- Hernanz F, Fidalgo M, Muñoz P, et al. Impact of reduction mammoplasty on the quality of life of obese patients suffering from symptomatic macromastia: A descriptive cohort study. J Plast Reconstr Aesthet Surg 2016;69:e168-73. [Crossref] [PubMed]
- Hofmann AK, Wuestner-Hofmann MC, Bassetto F, et al. Breast reduction;Modified "Lejour technique" in 500 large breasts. Plast Reconstr Surg 2007;120:1095-104. [Crossref] [PubMed]
- Hosnuter M, Tosun Z, Kargi E, et al. No-vertical-scar technique versus inverted T-scar technique in reduction mammoplasty: A two-center comparative study. Aesthetic Plast Surg 2005;29:496-502. [Crossref] [PubMed]
- Hughes LA, Mahoney JL. Patient satisfaction with reduction mammaplasty - an early survey. Aesthetic Plast Surg 1993;17:345-9. [Crossref] [PubMed]
- Kakagia D, Harkiolakis G, Sgouras N. Symptomatic macrornastia: A quality of life evaluation after reduction mammaplasty. Breast J 1998;4:152-5. [Crossref]
- Kececi Y, Sir E, Gungor M. Patient-Reported Quality-of-Life Outcomes of Breast Reduction Evaluated with Generic Questionnaires and the Breast Reduction Assessed Severity Scale. Aesthet Surg J 2015;35:48-54. [Crossref] [PubMed]
- Kim YS, Hwang K, Kim JH, et al. Central pedicle reduction mammaplasty with a vertical scar: a technical modification. J Plast Surg Hand Surg 2017;51:436-45. [Crossref] [PubMed]
- Klassen A, Fitzpatrick R, Jenkinson C, et al. Should breast reduction surgery be rationed? A comparison of the health status of patients before and after treatment: Postal questionnaire survey. BMJ 1996;313:454-7. [Crossref] [PubMed]
- Makki AS, Ghanem AA. Long-term results and patient satisfaction with reduction mammaplasty. Ann Plast Surg 1998;41:370-7. [Crossref] [PubMed]
- McCulley SJ, Rousseau TE. A modified Chiari L short-scar mammoplasty - the technique and results. Br J Plast Surg 1999;52:112-7. [Crossref] [PubMed]
- McCulley SJ, Schaverien MV. Superior and Superomedial Pedicle Wise-Pattern Reduction Mammaplasty Maximizing Cosmesis and Minimizing Complications. Ann Plast Surg 2009;63:128-34. [Crossref] [PubMed]
- McGregor JC, Hafeez A. Is there still a place for free nipple areolar grafting in breast reduction surgery? A review of cases over a three year period. J Plast Reconstr Aesthet Surg 2006;59:213-8. [Crossref] [PubMed]
- Mello AA, Domingos NAM, Miyazaki MC. Improvement in Quality of Life and Self-Esteem After Breast Reduction Surgery. Aesthetic Plast Surg 2010;34:59-64. [Crossref] [PubMed]
- Menderes A, Mola F, Vayvada H, et al. Evaluation of results from reduction mammaplasty: Relief of symptoms and patient satisfaction. Aesthetic Plast Surg 2005;29:83-7. [Crossref] [PubMed]
- Menéndez-Cardo A, Guillen-Grima F, Hontanilla B. Analysis of satisfaction after breast reduction comparing vertical scar versus inverted T-shaped technique using the Breast-Q questionnaire. Is patient satisfaction influenced by the amount of tissue removed? J Plast Surg Hand Surg 2017;51:414-9. [Crossref] [PubMed]
- Miller AP, Zacher JB, Berggren RB, et al. Breast reduction for symptomatic macromastia - can objective predictors for operative success be identified. Plast Reconstr Surg 1995;95:77-83. [Crossref] [PubMed]
- Mizgala CL, MacKenzie KM. Breast reduction outcome study. Ann Plast Surg 2000;44:125-33. [Crossref] [PubMed]
- Nguyen JT, Palladino H, Sonnema AJ, et al. Long-Term Satisfaction of Reduction Mammaplasty for Bilateral Symptomatic Macromastia in Younger Patients. J Adolesc Health 2013;53:112-7. [Crossref] [PubMed]
- Nuzzi LC, Firriolo JM, Pike CM, et al. The Effect of Reduction Mammaplasty on Quality of Life in Adolescents With Macromastia. Pediatrics 2017;140. [Crossref] [PubMed]
- O'Blenes CAE, Delbridge CL, Miller BJ, et al. Prospective study of outcomes after reduction mammaplasty: Long-term follow up. Plast Reconstr Surg 2006;117:351-8. [Crossref] [PubMed]
- Pérez-Panzano E, Gascon-Catalan A, Sousa-Dominguez R, et al. Reduction mammaplasty improves levels of anxiety, depression and body image satisfaction in patients with symptomatic macromastia in the short and long term. J Psychosom Obstet Gynaecol 2017;38:268-75. [Crossref] [PubMed]
- Pérez-Panzano E, Guemes-Sanchez A, Gascon-Catalan A. Quality of Life Following Symptomatic Macromastia Surgery: Short- and Long-term Evaluation. Breast J 2016;22:397-406. [Crossref] [PubMed]
- Portincasa A, Ciancio F, Cagiano L, et al. Septum-Enhanced Mammaplasty in Inferocentral Pedicled Breast Reduction for Macromastia and Gigantomastia Patients. Aesthetic Plast Surg 2017;41:1037-44. [Crossref] [PubMed]
- Radosa JC, Radosa MP, Baum S, et al. Reduction mammaplasty for symptomatic macromastia: which factors influence the post-operative outcome? Arch Gynecol Obstet 2013;287:715-22. [Crossref] [PubMed]
- Raispis T, Zehring RD, Downey DL. Long-term functional results after reduction mammaplasty. Ann Plast Surg 1995;34:113-6. [Crossref] [PubMed]
- Rogliani M, Gentile P, Labardi L, et al. Improvement of physical and psychological symptoms after breast reduction. J Plast Reconstr Aesthet Surg 2009;62:1647-9. [Crossref] [PubMed]
- Romeo M, Cuccia G, Zirilli A, et al. Reduction mammaplasty and related impact on psychosexual function. J Plast Reconstr Aesthet Surg 2010;63:2112-6. [Crossref] [PubMed]
- Ron O, Inbal A, Arad E, et al. Superomedial Pedicle Vertical Scar Breast Reduction: Objective and Subjective Assessment of Breast Symmetry and Aesthetics. Aesthetic Plast Surg 2018;42:639-47. [Crossref] [PubMed]
- Saariniemi K, Luukkaala T, Kuokkanen H. The outcome of reduction mammaplasty is affected more by psychosocial factors than by changes in breast dimensions. Scand J Surg 2011;100:105-9. [Crossref] [PubMed]
- Saariniemi KM, Joukamaa M, Raitasalo R, et al. Breast reduction alleviates depression and anxiety and restores self-esteem: A prospective randomised clinical trial. Scand J Plast Reconstr Surg Hand Surg 2009;43:320-4. [Crossref] [PubMed]
- Saariniemi KM, Sintonen H, Kuokkanen HO. The improvement in quality of life after breast reduction is comparable to that after major joint replacement. Scand J Plast Reconstr Surg Hand Surg 2008;42:194-8. [Crossref] [PubMed]
- Saariniemi KMM, Keranen UH, Salminen-Peltola PK, et al. Reduction mammaplasty is effective treatment according to two quality of life instruments. A prospective randomised clinical trial. J Plast Reconstr Aesthet Surg 2008;61:1472-8. [Crossref] [PubMed]
- Saariniemi KM, Kuokkanen HO, Tukiainen EJ. The outcome of reduction mammaplasty remains stable at 2-5 years' follow-up: A prospective study. J Plast Reconstr Aesthet Surg 2011;64:573-6. [Crossref] [PubMed]
- Sabino Neto M, Demattê MF, et al. Self-esteem and functional capacity outcomes following reduction mammaplasty. Aesthet Surg J 2008;28:417-20. [Crossref] [PubMed]
- Schnur PL, Schnur DP, Petty PM, et al. Reduction mammaplasty: An outcome study. Plast Reconstr Surg 1997;100:875-83. [Crossref] [PubMed]
- Serletti JM, Reading G, Caldwell E, et al. Long-term patient satisfaction following reduction mammoplasty. Ann Plast Surg 1992;28:363-5. [Crossref] [PubMed]
- Shakespeare V, Cole RP. Measuring patient-based outcomes in a plastic surgery service: Breast reduction surgical patients. Br J Plast Surg 1997;50:242-8. [Crossref] [PubMed]
- Shakespeare V, Postle K. A qualitative study of patients' views on the effects of breast-reduction surgery: a 2-year follow-up survey. Br J Plast Surg 1999;52:198-204. [Crossref] [PubMed]
- Shan XY, Huang XM, Wang MS, et al. Follow-up observational study of "bi-ring method" breast surgery for treating hypermastia and mastoptosis. Clin Exp Obstet Gynecol 2016;43:57-62. [PubMed]
- Sharma KS, Lim P, Baines R, et al. Reduction mammaplasty in adolescents: a review of the indications, timing, and outcomes in a regional plastic surgery unit. Eur J Plast Surg 2014;37:661-6. [Crossref]
- Shipkov H, Mojallal A, Braye F. Breast reduction with the posterosuperior pedicle: a series of 200 consecutive patients. Folia Med (Plovdiv) 2011;53:34-41. [Crossref] [PubMed]
- Singh KA, Pinell XA, Losken A. Is Reduction Mammaplasty a Stimulus for Weight Loss and Improved Quality of Life? Ann Plast Surg 2010;64:585-7. [PubMed]
- Spector JA, Karp NS. Reduction mammaplasty: A improvement at any size. Plast Reconstr Surg 2007;120:845-50. [Crossref] [PubMed]
- Spector JA, Kleinerman R, Culliford AT, et al. The vertical reduction mammaplasty: A prospective analysis of patient outcomes. Plast Reconstr Surg 2006;117:374-81. [Crossref] [PubMed]
- Spector JA, Singh SP, Karp NS. Outcomes after breast reduction - Does size really matter? Ann Plast Surg 2008;60:505-9. [Crossref] [PubMed]
- Sprole AM, Adepoju I, Ascherman J, et al. Horizontal or vertical? an evaluation of patient preferences for reduction mammaplasty scars. Aesthet Surg J 2007;27:257-62. [Crossref] [PubMed]
- Strong B, Hall-Findlay EJ. How Does Volume of Resection Relate to Symptom Relief for Reduction Mammaplasty Patients? Ann Plast Surg 2015;75:376-82. [Crossref] [PubMed]
- Taylor CJ, Chester DL. Bilateral breast reduction surgery in elderly women - A retrospective review of outcomes. J Plast Reconstr Aesthet Surg 2012;65:304-11. [Crossref] [PubMed]
- Thoma A, Ignacy TA, Duku EK, et al. Randomized Controlled Trial Comparing Health-Related Quality of Life in Patients Undergoing Vertical Scar versus Inverted T-Shaped Reduction Mammaplasty. Plast Reconstr Surg 2013;132:48e-60e. [Crossref] [PubMed]
- Thoma A, Sprague S, Veltri K, et al. Methodology and measurement properties of health-related quality of life instruments: A prospective study of patients undergoing breast reduction surgery. Health Qual Life Outcomes 2005;3:44. [Crossref] [PubMed]
- Thoma A, Sprague S, Veltri K, et al. A prospective study of patients undergoing breast reduction surgery: Health-related quality of life and clinical outcomes. Plast Reconstr Surg 2007;120:13-26. [Crossref] [PubMed]
- Tykkä E, Asko-Seljavaara S, Hietanen H. Patients' satisfaction with breast reconstruction and reduction mammaplasty. Scand J Plast Reconstr Surg Hand Surg 2001;35:399-405. [Crossref] [PubMed]
- Tykkä E, Rasanen P, Tukiainen E, et al. Cost-utility of breast reduction surgery - A prospective study. J Plast Reconstr Aesthet Surg 2010;63:87-92. [Crossref] [PubMed]
- Valtonen JP, Setala LP, Mustonen PK, et al. Can the efficacy of reduction mammoplasty be predicted? The applicability and predictive value of breast-related symptoms questionnaire in measuring breast-related symptoms pre- and postoperatively. J Plast Reconstr Aesthet Surg 2014;67:676-81. [Crossref] [PubMed]
- Chadbourne EB, Zhang S, Gordon MJ, et al. Clinical outcomes in reduction mammaplasty: a systematic review and meta-analysis of published studies. Mayo Clin Proc 2001;76:503-10. [Crossref] [PubMed]
- Beraldo FN, Veiga DF, Veiga-Filho J, et al. Sexual Function and Depression Outcomes Among Breast Hypertrophy Patients Undergoing Reduction Mammaplasty. Ann Plast Surg 2016;76:379-82. [Crossref] [PubMed]
- Ceber M, Yuksek A, Mutlu L, et al. Reduction Mammaplasty Effect on Pulmonary Function and Arterial Blood Gas in the Overweight Female. Aesthetic Plast Surg 2015;39:540-6. [Crossref] [PubMed]
- Pusic AL, Klassen AF, Scott AM, et al. Development of a New Patient-Reported Outcome Measure for Breast Surgery: The BREAST-Q. Plast Reconstr Surg 2009;124:345-53. [Crossref] [PubMed]
- Ware JE Jr, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual Framework and Item Selection. Med Care 1992;30:473-83. [Crossref] [PubMed]
- Rosenberg, M. Society and the adolescent self-image. Princeton University Press, 1965.
- Cohen WA, Homel P, Patel NP. Does Time Affect Patient Satisfaction and Health-Related Quality of Life After Reduction Mammoplasty? Eplasty 2016;16:e7. [PubMed]