An overview of animation deformity in prosthetic breast reconstruction
Introduction
Animation deformity is a common and distressing sequelae of breast reconstruction, estimated to occur in anywhere from 75–100% of sub-pectoral breast reconstructions (1,2). Animation deformity is caused by contraction of the pectoralis muscle against the breast implant, causing it and the overlying breast shape to unnaturally shift with muscle contraction. Recent heightened attention to this phenomenon has contributed to renewed interest in pre-pectoral breast reconstruction to prevent the deformity. Likewise, transition from a sub-pectoral to a pre-pectoral plane is advocated as the primary surgical treatment solution (3). Given that pre-pectoral breast reconstruction partly owes its resurgence to this phenomenon, herein we review current understanding of animation deformity, its prevalence, quantifiable measurements, available grading systems, impact on patient outcomes and existing treatment options.
Literature review
A PubMed search was performed utilizing the term “animation deformity”, returning 81 articles for review. Articles were limited to those in the English language in all years. Titles were reviewed by one author for relevance, yielding 30 articles that involved animation deformity in relation to breast surgery. Given the paucity of articles, both cosmetic and reconstructive breast surgery articles were included. Four additional articles were found on review of article references (4-7). We also included our own article that was accepted for publication September 2018 (8), bringing the total number of articles to 35.
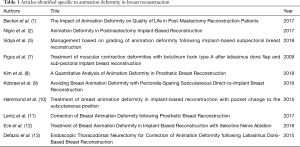
Of the 35 articles identified involving animation deformity in relation to breast surgery, eight articles involved cosmetic breast augmentation while 27 articles involved breast reconstruction. Fourteen articles were more generally about pre-pectoral breast reconstruction rather than animation deformity specifically, with only 13 articles focused entirely on animation deformity in breast reconstruction. Three of these 13 articles were commentaries on other articles, resulting in 10 original articles specific to animation deformity in breast reconstruction (Table 1).
Full table
What is animation deformity?
Animation deformity is a motion deformity characterized by breast implant movement with pectoralis contraction. Movement of the implant, in turn, causes movement of the overlying skin and nipple construct creating an unsightly deformity with movements that engage the pectoralis (Figure 1). Specifically, pectoralis contraction causes the implant to move upward and outward (superolaterally). While many studies have described treatment options to correct animation deformity—particularly transition to a pre-pectoral plane—few studies have actually focused on what causes it and risk factors for developing it.

Although initially described in patients undergoing breast augmentation, animation deformity in patients undergoing breast reconstruction is certainly more prevalent and likely more severe. Spear et al. reported 15% of breast augmentation patients presenting with moderate to severe deformity while studies in reconstructive patients have reported up to 80% with moderate to severe deformity (2,14). In our own series of breast reconstruction patients, we have found an average nipple displacement of 2.12 cm (8). This is in contrast to a study by Cheffe et al. demonstrating an average nipple displacement of only 1 cm after breast augmentation (15). Similarly, only 1% of patients undergoing breast augmentation would not recommend a sub-pectoral plane due to animation deformity, while over half of patients undergoing breast reconstruction would have been interested in knowing about alternative surgical options to prevent animation deformity (2,14)
What causes animation deformity?
Thus, we know animation deformity is certainly more prevalent and severe in the reconstructive compared to the cosmetic breast population. What we still don’t entirely understand are risk factors for developing it. As mentioned, very few studies have set out to look at understanding the etiology, but rather have focused on treatment options.
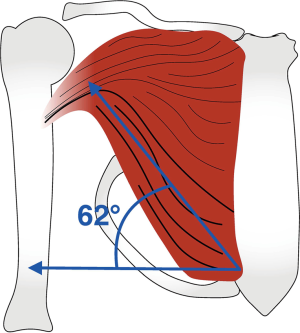
So far, the only factor that clearly contributes to developing animation deformity is placing the implant in a sub-pectoral position. Patient factors, including age, body mass index (BMI), handedness and athleticism have not been shown to correlate with development or severity of animation deformity (2,8). Surgical factors, such as implant size, implant type and mastectomy specimen weight, as well as peri-operative factors, such as radiation, infection and seroma, have also not been shown to correlate with development or degree of animation deformity (2,8). In our patient series, we have found division of the pectoralis with placement of acellular dermal matrix (ADM) is the only factor that correlates with increasing severity of animation deformity. Certainly, this makes sense when comparing it to the breast augmentation literature, which frequently describes preserving inferior pectoralis fibers to prevent animation deformity (4-6,16,17). Likewise, Spear has personally advocated for maintaining the inferior pectoralis insertion onto the sternum to prevent animation deformity (personal communication, S. Spear, 2016). These observations are in congruence with findings form our own patient population that the average vector of nipple displacement is 62 degrees in the superolateral direction—a line approximately parallel to the action of the inferior pectoralis fibers (accepted for publication, Figure 2) (8).
In essence, animation deformity is clearly related to sub-pectoral placement and freedom of pectoralis movement. It only makes sense that given increasing recognition of this phenomenon a paradigm shift in breast reconstruction has occurred to place greater emphasis on pre-pectoral reconstruction.
Quantifying animation deformity
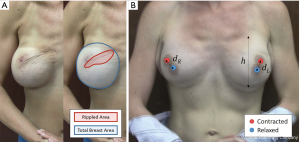
Given lack of a quantifiable description of animation deformity in the literature, our group endeavored to measure animation deformity in patients after sub-pectoral breast reconstruction. To do this, we measured amount of nipple displacement (in cm) with pectoralis muscle contraction, as well as percent surface area of skin contour irregularity on the breast mound. A total of 145 breasts (88 patients) were analyzed by still images captured on video at rest and with pectoralis contraction (Figure 3) (8). In this group, average nipple displacement was 2.12 cm (SD 1.04 cm), average vector of nipple displacement was 62.5 degrees (SD 20.6 degrees) in the superolateral direction and average percent surface area of skin contour irregularity was 16.4% (SD 15.41%). In total, 51.7% of breasts had nipple displacement greater than 2 cm and 29% of breasts had more than one-quarter surface area of the breast with skin contour irregularity. A total of 74.4% of breasts demonstrated nipple displacement between 30 and 80 degrees in the superolateral direction, a line approximately parallel to the action of the inferior pectoralis fibers. We also performed least squares regression analysis between nipple displacement and skin contour irregularity. This yielded a slope of 5.9%, meaning for every 1 cm of nipple displacement there was a 5.9% increase in percent surface area of the breast mound with skin contour irregularity.
Grading animation deformity
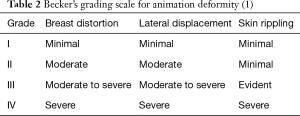
Two subjective grading schemes for animation deformity currently exist in the literature and we have proposed the first quantitative grading scale (Tables 2-4). The first grading scheme was described by Becker et al, dividing patients into one of four grades based on amount of breast distortion, displacement and skin rippling (1). Grade I patients have minimal distortion, lateral displacement and skin rippling. Grade II patients have moderate breast distortion and displacement but minimal skin rippling. Grade III patients have moderate to severe breast distortion with lateral displacement and evident skin rippling. Lastly, grade IV patients have severe breast distortion with lateral or superior displacement and severe skin rippling.
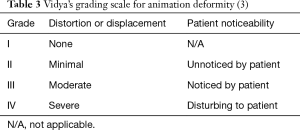
A second subjective grading scale that is perhaps simpler than Becker’s scale was presented by Vidya et al. (3). They again divide patients into four categories by severity of distortion. In addition, they specify whether distortion is noticed by the patient. Grade I patients have no distortion. Grade II patients have minimal distortion but unnoticed by the patient. Grade III patients have moderate distortion that is noticed by the patient. Grade IV patients have severe distortion that is disturbing to the patient.
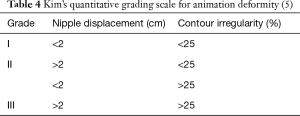
Both of the above-mentioned scales are relatively new, presented in the literature within the past 2 years. Given they both rely on subjective assessment of the amount of distortion by the rater, we developed a quantitative grading scale based on the measurements presented in the previous section to help standardize description of animation deformity across patients and raters (8). Our scale divides patients into three categories based on amount of nipple displacement (in cm) and percent surface area of skin rippling evident on the breast mound. Grade I patients have less than 2 cm nipple displacement and less than 25% (one-quarter of the breast mound) of skin rippling. Grade II patients have either greater than 2 cm nipple displacement or more than 25% surface area of skin rippling. Grade III patients have both greater than 2 cm nipple displacement and 25% surface area skin rippling. We hope this quantitative scale will simplify grading assessment of animation deformity and standardize discussion of animation deformity across studies as more research delves into this phenomenon.
Impact on patient outcomes
Just as few studies have examined etiology of animation deformity, only a handful of studies have examined how this complication affects patient satisfaction with their reconstruction. While animation deformity has been studied more in the breast augmentation literature, it has not been shown that animation deformity affects patient satisfaction with their breast augmentation, likely because it tends to be less severe in this group of patients (14). This contrasts with the breast reconstruction population in which deformity tends to be more severe and is more likely to be asymmetric given greater likelihood of a unilateral procedure. Indeed, it has been shown that asymmetry after breast reconstruction does contribute to patient emotional distress (18).
Nigro et al. surveyed patients to determine patient awareness of animation deformity (2). In this group, 75.6% were aware of the presence of animation deformity. More importantly, half of patients would have liked information on alternative surgical options to prevent animation deformity.
Becker et al looked specifically at the impact of animation deformity on quality of life in reconstructive patients (1). In this group, 80% of patients noted they were bothered by animation deformity with nearly half of patients saying it affected them on a daily basis. One-fourth of patients stated it affected their personal relationships and 40% stated it negatively impacted them emotionally or psychologically. This study underscored the importance of counseling patients about animation deformity prior to reconstruction given its prevalence and significance in this patient population.
Treatment options
Up to 28% of breast reconstruction patients will request revisionary surgery due to animation deformity and half of patients state they would have liked to know about alternative surgical options to avoid animation deformity at the time of mastectomy (1,2). Given this, some surgeons are converting to pre-pectoral breast reconstruction in the hopes of preventing this complication entirely (9). Downsides to pre-pectoral reconstruction, including greater implant visibility, ledge contouring and increased risk of mastectomy skin flap necrosis, have to be weighed against the desire to prevent animation deformity and patients should be counseled on an individual basis as to their likelihood of success with such a procedure. Delayed transition from a sub-pectoral to a pre-pectoral plane is also an option for treating animation deformity should it occur and may mitigate some of the risks related to mastectomy skin flap necrosis with pre-pectoral reconstruction at the time of mastectomy (10,11). Another alternative for treatment is partial conversion to a pre-pectoral plane, as has been described by multiple authors in cosmetic augmentation (4-6,16,17). This gives the benefit of eliminating the pectoralis fibers that have the greatest effect on implant movement while still maintaining pectoralis upper pole coverage to reduce implant visibility, palpability and contour ledging.
Given that the only modifiable factor that has been shown to impact degree of animation deformity in our data is release of the pectoralis, further surgical refinements could focus on ways to perform sub-pectoral reconstruction without release of the muscle when a pre-pectoral plane is not an option. A recent alternative treatment for animation deformity introduced by Eck and colleagues describes selective nerve ablation (12,13). One case study describes a patient with animation deformity who was successfully treated with selective cautery ablation of the medial and lateral pectoral nerves, allowing her to keep the implant in a sub-pectoral position (12). A similar but non-surgical treatment involves Botox injection into the pectoralis, although this only gives a temporary effect (7).
Conclusions
Animation deformity is a distressing sequelae of sub-pectoral breast reconstruction and we are only starting to understand how prevalent and significant the phenomenon really is. Based on our quantitative analysis, average nipple displacement is 2.12 cm at 62 degrees in the superolateral direction and the only factor correlated with severity is release of the pectoralis muscle—highlighting the pectoralis’ role in contributing to the deformity. Grading systems are still relatively new, underscoring the limited amount of research that has gone into the causes and implications behind animation deformity. Some degree of deformity is likely present in all patients with sub-pectoral breast reconstruction and the majority of patients notice its presence. As such, further research into causes and especially methods to enhance pre-pectoral reconstruction are warranted given this is the primary mode of treatment.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Becker H, Fregosi N. The Impact of Animation Deformity on Quality of Life in Post-Mastectomy Reconstruction Patients. Aesthet Surg J 2017;37:531-6. [Crossref] [PubMed]
- Nigro LC, Blanchet NP. Animation Deformity in Postmastectomy Implant-Based Reconstruction. Plast Reconstr Surg Glob Open 2017;5:e1407. [Crossref] [PubMed]
- Vidya R, Tafazal H, Salem F, et al. Management based on grading of animation deformity following implant-based subpectoral breast reconstruction. Arch Plast Surg 2018;45:185-90. [Crossref] [PubMed]
- Khan UD. Muscle-splitting breast augmentation: a new pocket in a different plane. Aesthetic Plast Surg 2007;31:553-8. [Crossref] [PubMed]
- Khan UD. Muscle-splitting, subglandular, and partial submuscular augmentation mammoplasties: a 12-year retrospective analysis of 2026 primary cases. Aesthetic Plast Surg 2013;37:290-302. [Crossref] [PubMed]
- Baxter RA. Subfascial breast augmentation: theme and variations. Aesthet Surg J. 2005;25:447-53. [Crossref] [PubMed]
- Figus A, Mazzocchi M, Dessy LA, et al. Treatment of muscular contraction deformities with botulinum toxin type A after latissimus dorsi flap and sub-pectoral implant breast reconstruction. J Plast Reconstr Aesthet Surg 2009;62:869-75. [Crossref] [PubMed]
- Kim JY, Qiu CS, Chiu WK, et al. A Quantitative Analysis of Animation Deformity in Prosthetic Breast Reconstruction. Plast Reconstr Surg 2018. [Epub ahead of print].
- Kobraei EM, Cauley R, Gadd M, et al. Avoiding breast animation deformity with pectoralis-sparing subcutaneous direct-to-implant breast reconstruction. Plast Reconstr Surg Glob Open 2016;4:e708. [Crossref] [PubMed]
- Hammond DC, Schmitt WP, O’Connor EA. Treatment of breast animation deformity in implant-based reconstruction with pocket change to the subcutaneous position. Plast Reconstr Surg 2015;135:1540-4. [Crossref] [PubMed]
- Lentz RB, Piper ML, Gomez-Sanchez C, et al. Correction of breast animation deformity following prosthetic breast reconstruction. Plast Reconstr Surg 2017;140:643-4e. [Crossref] [PubMed]
- Eck DL, Nguyen DC, Barnes LL, et al. Treatment of Breast Animation Deformity in Implant-Based Reconstruction with Selective Nerve Ablation. Aesthetic Plast Surg 2018;42:1472-5. [Crossref] [PubMed]
- DeFazio MV, Pittman TA. Endoscopic thoracodorsal neurectomy for correction of animation deformity following latissimus dorsi-based breast reconstruction. Plast Reconstr Surg 2015;136:573-4e. [Crossref] [PubMed]
- Spear SL, Schwartz J, Dayan JH, et al. Outcome assessment of breast distortion following submuscular breast augmentation. Aesthetic Plast Surg 2009;33:44-8. [Crossref] [PubMed]
- Cheffe MR, Valentini JD, Collares MV, et al. Quantifying Dynamic Deformity After Dual Plane Breast Augmentation. Aesthetic Plast Surg 2018;42:716-24. [Crossref] [PubMed]
- Khan UD. High transverse capsuloplasty for the correction of malpositioned implants following augmentation mammoplasty in partial submuscular plane. Aesthetic Plast Surg 2012;36:590-9. [Crossref] [PubMed]
- Baxter RA. Update on the split-muscle technique for breast augmentation: prevention and correction of animation distortion and double-bubble deformity. Aesthetic Plast Surg 2011;35:426-9. [Crossref] [PubMed]
- Kim MK, Kim T, Moon HG, et al. Effect of cosmetic outcome on quality of life after breast cancer surgery. Eur J Surg Oncol 2015;41:426-32. [Crossref] [PubMed]