Impact of completion thyroidectomy timing on post-operative complications: a systematic review and meta-analysis
Introduction
Completion thyroidectomy is the removal of the remaining thyroid tissues with a second operation in patients who have had a lobectomy as the primary operation that revealed thyroid malignancy (1). The indication of completion thyroidectomy fall under three categories. These are: postoperative diagnosis of cancer, residual or recurrent cancer, and symptomatic recurrent multinodular goiter (2,3).
Completion thyroidectomy is thought to carries a higher risk of post-operative complications Due to the issues of tissue inflammation, adhesions, edema, and development of scar tissue after the primary operation (4-8). The risks of complications usually occurs during dissection of the scar tissue that surround the recurrent laryngeal nerve or the vascular pedicle of the parathyroid glands (9,10), due to loss of landmarks. As in the primary thyroid surgery, recurrent laryngeal nerve palsy and hypoparathyroidism are the major complications in completion thyroidectomy operation.
In this study early completion thyroidectomy is the procedure done between 7 to 90 days, whereas delayed completion thyroidectomy is done after 90 days. Performing completion thyroidectomy in the time period between 7 and 90 days has been suggested to be associated with higher risk of complications compared to completion thyroidectomy done after 90 days (11-14).
The best timing of completion thyroidectomy remains uncertain. In view of this, we aim to present a comprehensive systematic review and a meta-analysis to compare the result of early completion thyroidectomy (7–90 days) versus delayed completion thyroidectomy (>90 days) from the reported studies.
Methods
This systematic review and Mata analysis was conducted according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (15).
Electronic literature databases
A literature search was conducted in September 2017 using the following databases: PubMed, Ovid MEDLINE(R) (including Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily, Cochrane library (Issue 7 of 12, July 2017), Elsevier Scopus and google scholar, identifying all related articles from 1995 until 2017. The key word combinations used for the search were: (“completion thyroidectomy” OR “thyroid reoperation”) AND (“timing”). The cited articles in the included articles were also screened to identify relevant articles not found by our literature search. The first search yielded 146 articles. Concrete reviews of abstracts were performed by two authors independently to select appropriate studies for full-text review. Disagreements regarding selected articles were resolved by through discussion.
Inclusion and exclusion criteria
All studies comparing the outcomes of completion thyroidectomy done within 7–90 days versus after 90 days of the primary surgery, either prospective randomized or retrospective, in any language were considered candidates. The included studies had to contain specific complication rate data to allow for their calculation.
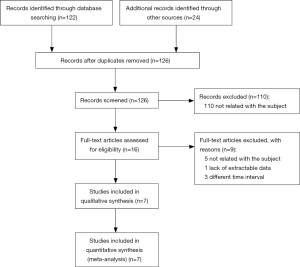
Exclusion criteria were reviews, case reports or series, comments or letters, and duplicate publication, we also excluded studies with incomplete initial data. The full text of articles that survived the abstract review were retrieved and examined for further selection based on the criteria mentioned above. Finally, 7 articles passed the full-text review and were thus included in this analysis (Figure 1).
Study quality assessment
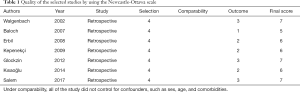
Two authors independently judged the methodological quality of all the selected studies using the Newcastle-Ottawa scale (NOS) for cohort studies (16). The checklist contained 9 items (regarding patient selection, comparability of the study and exposure) with every item accounting for 1 point. The scores were evaluated as follows: ≤5, low quality; 6–7, medium quality; 8–9, high quality. Article with a final score of 5 or more points were included. The quality score average was medium with 6 studies obtaining a score of 6 or more (ranging between 5 and 7) (Table 1) the proportion of agreement was measured by using the intraclass correlation coefficient. A coefficient of 0.7 or greater was considered adequate.
Full table
Data extraction
Full text articles were obtained for studies that fulfilled the inclusion criteria or for which sufficient information was given. Two authors independently reviewed the included articles to extract data on excel spreadsheet. The extracted data sets were compared to confirm accuracy, any discrepancies in extracted data were resolved by through discussion. The following data were extracted from the articles: first author’s last name, publication year, country, number of patient, mean age, sex, study design and the timing of CT (Table 2). The primary outcome measure incidences of postoperative complication, including Transient and persistent: hypocalcemia, vocal cord paresis and hypoparathyroidism.
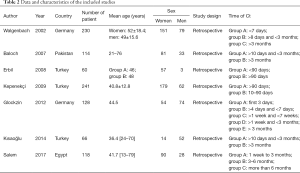
Full table
Statistical analysis
Seven articles were analyzed using Revman 5.3 (RevMan version 5.3., Copenhagen: the Nordic Cochrane collaboration, 2012) to estimate the overall pooled effect size. The incidence of post-operative complication was calculated based on the number of events. The pooled risks for the overall complications include transient and persistent hypocalcemia, vocal cord paresis and hypoparathyroidism. The overall complication was estimated and compared between the early completion thyroidectomy and delayed completion thyroidectomy groups.
The result of the Mata-analysis were presented using the fixed effect model, odds ratio and corresponding 95% confident intervals (CIs) and the Z test for pooled effect size estimate. Forest plots were used for graphical display of the results.
To assess the heterogeneity among studies, we calculated using the I2 statistic: 25% to 50% indicates low heterogeneity, 50% to 75% indicate moderate heterogeneity, >75% indicate high heterogeneity.
A (P value) equal to or less than 0.05 was consider statistically significant different. Potential publication bias was assessed by performing visual inspection of funnel plot for asymmetry, based on the primary outcome, that is, postoperative complication.
Results
Search result
Our searched yield 126 studies from searching all the data bases mentioned above (Figure 1) present a flowchart that briefly overviews the search process for the studies included in the meta-analysis. Out of a total of 126 studies, we excluded 119 studies. After a thorough evaluation of the final studies, we selected 7 studies that met eligibility criteria.
Basic characteristics and quality assessment
The included studies were published between 2002 and 2017. The characteristics of the included studies are summarized in (Table 2). All included studies were retrospective cohort design. The sample size ranged from 26 to 113 patients. Three of the studies were conducted in Turkey, two in Germany, one in Egypt and one in Pakistan. We judged 6 studies of moderate methodology quality, and 1 study to be low quality (Table 1).
Meta-analysis of primary outcomes
A total of 7 studies were included in this analysis to estimate the pooled risk of complication.
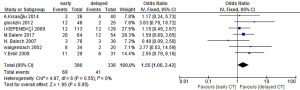
Transient hypocalcemia occurred in 8.97% (27/301) and 8.2% (20/244) of the patient in the early CT and delayed CT, respectively. The persistent hypocalcemia rates were 1.52% and 0.72% in the early CT (5/330) and delayed CT (2/276), respectively. There were no significant difference in the occurrence of transient hypocalcemia (OR =1.21; 95% CI, 0.65–2.25; Z=0.60; P=0.55) or persistent hypocalcemia (OR =1.95; 95% CI, 0.40–9.49; Z=0.83; P=0.41) (Figure 2).
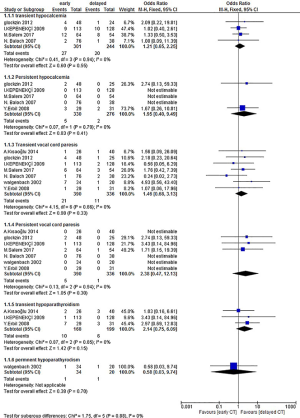
The prevalence of Transient vocal cord paresis was 5.38% (21/390) in early CT group versus 3.27% (11/336) in the delayed CT group, without significant deference (OR =1.46; 95% CI, 0.68–3.13; Z=0.98; P=0.33). The prevalence of Persistent vocal cord paresis was 1.28% (5/390) in early CT group versus 0.3% (1/336) in the delayed CT group, without any significant deference (OR =2.38; 95% CI, 0.47–12.13; Z=1.05; P=0.30) (Figure 2).
Three studies reported transient hypoparathyroidism, and there was no significant differences in the occurrences between the groups (OR =2.14; 95% CI, 0.75–6.09; Z=1.42; P=0.15) (Figure 2).
One study reported permanent hypoparathyroidism, with no significant differences in the occurrences between the groups (OR =0.58; 95% CI, 0.03–9.74; Z=0.38; P=0.70).
Pooled analysis revealed significant reduction in the overall complications in the delayed surgery group compared too early surgery group (OR =1.55; 95% CI, 1.00–2.42; Z=1.95, P=0.05) (Figure 3). A similar result for the test of overall effect was obtained when the random-effect model was used. No significant heterogeneity was detected between the studies (I2=0%, P=0.55) (Figure 3).
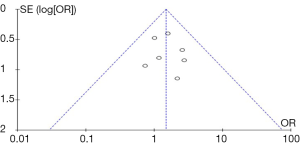
Funnel plots of the studies showed symmetry of the study distribution, indicating low possibility of publication bias in this analysis (Figure 4). However, the result is unreliable, since there is limited number of studies in this analysis.
Discussion
We performed a systemic review and meta-analysis of reported outcomes to compare the result of early completion thyroidectomy versus delayed completion thyroidectomy. A total of 7 studies were included in the current study. All of which were retrospective cohort studies including 957 patients. Most common complications reported were transient hypocalcemia, persistent hypocalcemia, transient vocal cord paresis, persistent vocal cord paresis and transient hypoparathyroidism. In Most patients the histopathologic examination of the restricted thyroid gland, after the primary procedure showed papillary cancer (1,13,17,18). The heterogeneity in our meta-analysis was low (I2=0), indicating that the studies included in our systematic review and meta-analysis were statistically reliable.
The included studies comparing complication rates between early and delayed completion thyroidectomy have shown mixed results. Some conclude that delayed completion thyroidectomy have lower rates of postoperative complications, including transient hypocalcemia, persistent hypocalcemia, transient vocal cord paresis, persistent vocal cord paresis and transient hypoparathyroidism, compared to early completion thyroidectomy (11,13,18,19), other studies suggest the Timing of completion thyroidectomy did not significantly affect the incidence of post-operative complication (1,13,19).
The result of our meta-analysis suggested that delayed completion thyroidectomy surgery was significantly associated with lower odds of post-operative complications (P=0.05) compared to early completion thyroidectomy surgery.
Limited studies reported the incidence of post-operative complications In patients who had the completion thyroidectomy in the first week after the initial surgery, which might be due to restriction of timing in Establishing the diagnosis and recovery from the first operation often goes beyond the first week to 10 days deadline (20), therefore these periods in the studies were exclude from this meta-analysis, and there is a need for additional well designed studies to clear the insights into the effects of this timing period
This study has some limitations. First, all of the studies in our meta-analysis were retrospective cohort studies, and is therefore subject to the individual limitation of the included studies. Second, the type of cancer, the operation, operation technique and definitions for hypocalcaemia and RLN palsies varies between the studies. These variations may limit the effective comparison of the outcomes. Therefore For meaningful comparisons a standardization of definitions and protocols for hypocalcaemia and RLN palsies is required.
Despite these limitations, this review is the first to summarize the outcome of early verse delayed completion thyroidectomy.
Conclusions
On the basis of current evidence, delayed completion thyroidectomy is associated with lower rate of post-operative complications compared to early completion thyroidectomy. Further studies are needed for definite conclusion.
Acknowledgements
This project was supported by the Health Science Research Center at Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Supporting Information: PRISMA Checklist (DOC).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kısaoğlu A, Ozogul B, Akcay MN, et al. Completion thyroidectomy in differentiated thyroid cancer: When to perform? Ulus Cerrahi Derg 2014;30:18-21. [Crossref] [PubMed]
- Makay O, Unalp O, Icoz G, et al. Completion thyroidectomy for thyroid cancer. Acta Chir Belg 2006;106:528-531. [Crossref] [PubMed]
- Varaldo E, Ansaldo GL, Assalino M, et al. Completion thyroidectomy for differentiated thyroid cancer (Results in a Consecutive Series of 68 Patients). Acta Chirurgica Belgica 2012;112:40-3. [Crossref] [PubMed]
- Hardman JC, Smith JA, Nankivell P, et al. Re-operative thyroid surgery: a 20-year prospective cohort study at a tertiary referral centre. European archives of oto-rhino-laryngology Eur Arch Otorhinolaryngol 2015;272:1503-8. [Crossref] [PubMed]
- Vaiman M, Nagibin A, Olevson J. Complications in primary and completed thyroidectomy. Surg Today 2010;40:114-8. [Crossref] [PubMed]
- Lefevre JH, Tresallet C, Leenhardt L, et al. Reoperative surgery for thyroid disease. Langenbecks Arch Surg 2007;392:685-91. [Crossref] [PubMed]
- Rigberg D, Chandler C, Ashley S, et al. Safety of completion thyroidectomy for multicentric carcinoma. Am Surg 1998;64:189-91. [PubMed]
- Pironi D, Pontone S, Vendettuoli M, et al. Prevention of complications during reoperative thyroid surgery. Clin Ter 2014;165:e285-90. [PubMed]
- Pezzullo L, Delrio P, Losito NS, et al. Post-operative complications after completion thyroidectomy for differentiated thyroid cancer. Eur J Surg Oncol 1997;23:215-8. [Crossref] [PubMed]
- Li YJ, Wang YZ, Yi ZB, et al. Comparison of Completion Thyroidectomy and Primary Total Surgery for Differentiated Thyroid Cancer: A Meta-Analysis. Oncol Res Treat 2015;38:528-31. [Crossref] [PubMed]
- Erbil Y, Bozbora A, Ademoglu E, et al. Is timing important in thyroid reoperation? J Otolaryngol Head Neck Surg 2008;37:56-64. [PubMed]
- Chao TC, Jeng LB, Lin JD, et al. Reoperative thyroid surgery. World J Surg 1997;21:644-7. [Crossref] [PubMed]
- Salem MA, Ahmed BM, Elshoieby MH. Optimum Timing and Complication of Completion Thyroidectomy for Differentiated Thyroid Cancer. J Cancer Ther 2017;8:518-26. [Crossref]
- Chao TC, Jeng LB, Lin JD, et al. Completion thyroidectomy for differentiated thyroid carcinoma. Otolaryngol Head Neck Surg 1998;118:896-9. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 2009;6. [Crossref] [PubMed]
- Wells GA, Shea B, O'Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2011. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed March 01, 2015.
- Kepenekçi I, Demirer S, Koçak S, et al. Timing of the reoperation in completion thyroidectomy. Turk Klin Tip Etigi Hukuku Tarihi 2009;29:1212-6.
- Glockzin G, Hornung M, Kienle K, et al. Completion Thyroidectomy: Effect of Timing on Clinical Complications and Oncologic Outcome in Patients with Differentiated Thyroid Cancer. World J Surg 2012;36:1168-73. [Crossref] [PubMed]
- Walgenbach S, Junginger T. Is the timing of completion thyroidectomy for differentiated thyroid carcinoma prognostic significant? Zentralbl Chir 2002;127:435-8. [Crossref] [PubMed]
- Baloch MN, Aslam T, Maher M. Completion thyroidectomy: relation of timing with complications. Pak J Surg 2007;23:245-7.