Utilizing large volume fat grafting in breast reconstruction after nipple sparing mastectomies
Introduction
This paper is intended to serve as a broad overview of fat grafting and its potential role in reconstructing the breast following nipple sparing mastectomies. Historically, breast cancer was surgically treated with a Halsted radical mastectomy. Over time, the mastectomy technique has increasingly balanced tumor resection and tissue preservation resulting in increased skin preservation. Today, nipple sparing mastectomy (NSM) has gained popularity in prophylactic mastectomies. For properly selected patients, NSM typically results in a superior aesthetic outcome compared to a modified radical mastectomy.
The oncological safety of NSM has been confirmed with recurrence rates comparable to other types of mastectomy. Furthermore, the complication rates for NSM are comparable to those in skin-sparing mastectomy (1,2).
The inclusion criteria for NSM are as follows: early-stage tumor that is less than 3 cm in size, tumor to nipple distance of at least 2 cm, clinically negative axillary lymph nodes, absence of skin involvement and negative retro-areolar biopsy. These criteria may even become more inclusive as recent data has advocated that NSM may be safely performed with a tumor to nipple distance as small as 1 cm (3).
There are several options for reconstructing breasts after NSM. The variables that determine the appropriate reconstruction include patient habitus, smoking history, breast ptosis, post-mastectomy skin flap viability, and the need for adjunctive radiation and/or chemotherapy. Implant-based breast reconstruction represents the most commonly performed technique. This can include a two-stage procedure with tissue expanders (later exchanged for an implant), or alternatively, a single stage reconstruction with immediate implant placement at the time of the mastectomy. Single stage reconstruction has been arguably associated with higher rates of complications/revisions but excellent aesthetic outcomes can be achieved with proper planning and patient selection. Finally, autologous breast reconstruction has increased in popularity for breast reconstruction and is commonly utilized in NSM reconstruction, as well. Autologous breast reconstruction can be performed in an immediate or delayed fashion. The timing of the reconstruction is typically selected based on multiple intrinsic and extrinsic factors related to the both the patient as well as surgeon preference.
Finally, the development of large volume fat grafting as an additional reconstructive technique that can be utilized in NSM reconstruction, either to complement another reconstructive approach or as a standalone form of reconstruction, has had a major impact on reconstructive outcomes. Initially fat grafting was not widely accepted due to concerns of oncologic safety, tumor surveillance, and technique efficacy. Despite initial criticism and reluctance, there is an increasing body of evidence which has demonstrated that fat grafting can be safely and effectively utilized for breast reconstruction. Currently, well performed large volume fat grafting is generally accepted to be both safe and effective (4,5).
This paper will discuss how large volume fat grafting can be applied to nipple sparing mastectomies to achieve optimal breast reconstructive results.
Surgical technique
Incorporating large volume fat grafting with NSM reconstruction requires that the surgeon appropriately select the best reconstructive method for the patient. This initially begins with excellent communication between the plastic surgeon the breast surgeon and the patient on placement of the mastectomy incision. Following selection of the breast reconstruction technique, large volume fat grafting can be incorporated into NSM reconstruction with several methods that will be discussed below.
Breast mastectomy
The first decision requires selection of the NSM incision placement. A variety of incisions can be utilized commonly including a radial, vertical, or inframammary placement. The primary goal of the incision is to allow for a well-controlled precise and safe mastectomy. Small breasts can adequately be treated through an inframammary incision. However, larger or moderately ptotic breasts should be treated thru an infra areolar incision extending around the lower third of the circumference of the nipple areola complex with an additional vertical limb (Figure 1). Optimal incision placement allows adequate exposure for the surgeon to perform the mastectomy and subsequent reconstruction while also minimizing trauma to the skin flaps throughout the case.

Pre-expansion (external volume expansion)
Large volume fat grafting depends on the four Ps, pre-expansion, procurement, processing and placement. The viability of the fat is dependent on the overall parenchymal space for grafting (i.e., the capacity of the recipient site). The volume of the recipient site dictates the volume of fat that can be safely grafted. Over grafting of a low-volume recipient site leads to a negative cascade of events that include graft loss, fat necrosis and oil cysts. Maximal grafting can be determined by lack of resistance to the cannula per pass, peau d’orange appearance of the recipient skin, free flow of fat out through the infiltration site and increased interstitial pressure (if measured). External pre-expansion increases the recipient site capacity and thus, the given volume of graft injected. Additionally, pre-expansion can be helpful in identifying contour irregularities before grafting that can be modified with needle band release. Finally, pre-expansion has been demonstrated to improve vascularity and angiogenesis leading to increased fat viability (Figure 2).
Procurement (harvesting fat)
For the purposes of grafting the breast, most patients [even those with relatively low body mass index (BMI)] have ample fat donor-sites for transfer. Multiple sites are often utilized so as to ensure that the total volume of fat harvested is adequate for the purposes of reconstruction.
We typically utilize a multi-hole cannula connected to a standard in line liposuction aspirator (Figure 3). The cannula holes are determined to match the infiltrating cannula to prevent blockage or subsequent bolus infiltration.
Processing
Our preferred technique utilizes low speed manual centrifugation. The fat is collected in a sterile canister and then transferred to 60 cc syringes which are loaded on to a sterile low force bucket handle centrifuge. The centrifuge is spun for two minutes resulting in about 20–40 G of total force (Figure 4). The additional crystalloid is removed. The result is a fat that has a slushy consistency that is ready for injection (Figure 5).


Placement (fat transfer/injection)
Placement is performed via 60 cc syringe attached to a 16-gauge, 15 cm saddle tip cannula (Coleman cannula) (Figure 6). Injection sites are placed around the breast as needed to accurately inject fat to areas of interest. Injection with a reciprocating “to and fro’ motion is utilized with constant light pressure on the plunger to avoid bolus injections (Figure 7). Care is taken to avoid over injecting beyond the capacity of the recipient site. Signs of a disproportionately high graft to capacity ratio include: peau d’orange skin appearance, very firm tissue turgor, leaking fat leaking from injection sites, and excessive skin blanching (although this is less reliable given concurrent use of epinephrine).


NSM reconstruction utilizing fat alone
Primary large volume fat grafting can be used for patients that desire the natural feel and appearance of autologous reconstruction and desire to avoid the use of implants or flap surgery. Breast size and donor fat adequacy may preclude some patients from autologous reconstruction. Additionally, some patients are dissuaded from autologous free flap reconstruction because of the invasiveness and recovery inherent to the reconstruction.
Our view of primary large volume fat grafting in the NSM requires placement of fat to restore soft tissue deficiency over several stages. Initially, the pectoralis major is injected with fat. Using the blunt tip cannula, fat is injected evenly throughout the pectoralis major muscle. Approximately 100 cc of fat is evenly dispersed within pectoralis major (Figure 8). We incorporate similar principles when injecting into the muscle as we do the breast tissue. Care is again taken to not markedly exceed the capacity of the recipient site. The mastectomy skin flaps are laid over the muscle making sure the nipple is in good position. A recovery period of approximately three months is typically mandated prior to proceeding with the next stage of reconstruction.
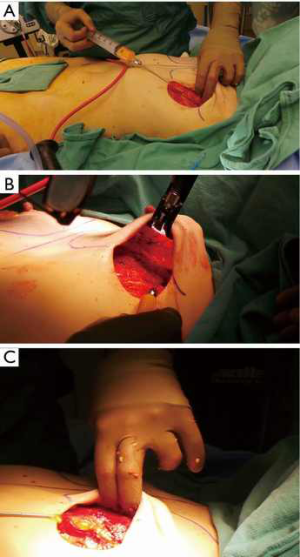
After 3 months, an external volume expansion device is utilized. Pre-expansion is necessary to increase recipient capacity and identify cicatricial adhesions. Patients wear the device over the course of 3 weeks (7 days a week and 6 hours a day). Once pre-expansion is complete, another session of fat grafting is performed. Fat is once again injected as previously described with the goal of injecting as much fat as tolerated by the recipient site. Cicatricial adhesions are treated by needle band release. We utilize a skin hook that is used to place tension on the skin over the adhesion and a percutaneously placed 16-gauge needle is used to release the adhesion (Figure 9). Once the fibrotic band is released, there is less tension in the areas and fat can be grafted to help restore the contour of the breast.
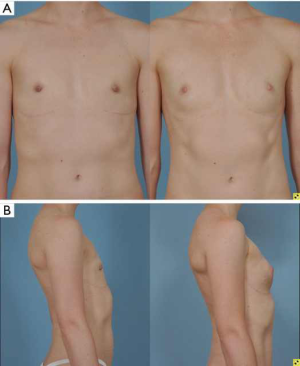
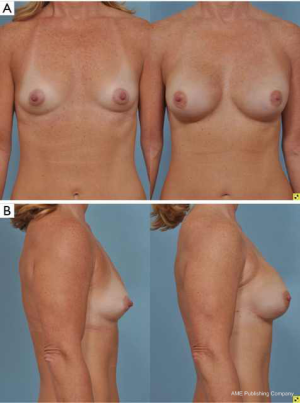
Patients return to the operating room in subsequent three to 6-month intervals for additional fat grafting, as needed (most patients require two to four sessions in total). Based on the work of Del Vecchio and Bucky, an estimated sixty percent of volume maintenance is expected per session however, there are many factors that influence volume maintenance (graft to capacity ratio, radiation, scarring, quality of harvest/processing, injection technique) (8). The end result in reconstruction of NSM strictly with fat grafting is a breast of natural proportion and feel (Figure 10).
NSM with composite augmentation (implant and fat grafting)
Composite augmentation, which combines both a prosthetic implant and large volume fat grafting, is the technique that is most commonly utilized. This approach utilizes the implant for the core volume and projection. The result is improved by the addition of autologous fat around the implant and to areas of contour irregularity in order to provide a more natural appearance and feel.
The process includes determining a breast implant size based on breast and chest dimensions. Both round implants, and newer, anatomically shaped form stable implants are utilized with success (Figures 11,12).

Another alternative for composite augmentation includes the use of tissue expanders followed by fat grafting. Appropriate tissue expander selection has been well described. We prefer medium height expanders to control nipple position in NSM patients. The short height tissue expander is more commonly utilized for non-NSM because of the greater lower pole expansion. However, if used in nipple sparing mastectomies the nipple tends to be positioned too superiorly and laterally. Expanders may be covered with biologic mesh (i.e., acellular dermal matrix) or total submuscular coverage can be used to secure the expander under the skin flap (i.e., serratus musculofascial flap to close the inferolateral aspect of the pocket covering the tissue expander). Tissue expansion is typically performed over 3 months.
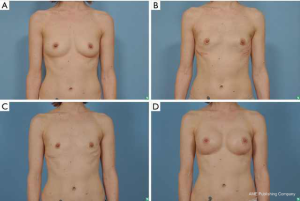
Once the final volume of the implant is achieved, a decision is made whether fat grafting is necessary. Fat grafting prior to tissue expander removal allows for replacement of soft tissue deficit. After three months, the tissue expander is replaced with an implant of choice. At this time, further fat grafting can be performed with care to place the fat superficial to expander/implant capsule. The optimal result provides a natural appearing breast with excellent contour and feel (Figure 13).
Discussion
NSM has evolved in order to provide breast cancer patients with better aesthetic outcomes following mastectomy. By preserving the nipple-areola complex (NAC), as well as the native inframammary fold and breast skin envelope, the patient is able to obtain a more natural and improved aesthetic result (9,10). In comparison to women whom have undergone skin-sparing mastectomies and NAC reconstruction, women who underwent NSM were demonstrated to have improved body image self-assessment, psychological adjustment, nipple sensitivity, and overall higher levels of satisfaction (9).
NSM has also been shown to be a safe procedure with low complication rates, including a nipple necrosis rate of around 4%. Factors associated with complications include smoking, use of periareolar incision, increasing BMI, and preoperative radiation therapy (2). NSM can be safely performed in combination with tissue expander, direct to implant (DTI) or autologous reconstruction. For NSM patients, tissue expander reconstruction has been found to have the lowest rate of both complete nipple necrosis (1.3% vs. 3.9% and 3% for tissue expander, DTI and autologous reconstruction respectively) as well as major mastectomy flap necrosis (1.9% vs. 6.5% and 5.3% for tissue expander, DTI and autologous reconstruction respectively) (11).
Autologous fat grafting is frequently used in both cosmetic as well as reconstructive cases to improve breast size and contour. There are many aspects of fat grafting that make it an ideal filler for the breast. It is nontoxic, biocompatible, easy to use and not expensive. It also provides a natural feel and appearance (12). In the past, there have been concerns that fat grafting to the breast will impede the detection of early breast cancers on mammography. However, fat grafting has proven to be a safe and effective procedure and postoperative mammographic findings are similar to those seen after other breast procedures such as breast reduction (13). Furthermore, studies have demonstrated no increased risk of loco-regional recurrence or decrease in survival following fat grafting after breast reconstruction (14,15). Complication rates are low (6.3%) with the most common being fat necrosis (3.6%), oil cysts (1.8%) and infection (0.9%). Significant aesthetic improvements can be made in breast volume, contour and superomedial fullness (16). Additionally, fat grafting may improve skin quality and wound healing in mastectomy skin flaps that have previously undergone radiation therapy. It has been proposed that contents within the lipoaspirate or fat itself may be responsible for this effect (17-20). Radiation therapy has traditionally been associated with high complication rates in implant-based reconstruction. For this reason, Salgarello et al. have reported two cases of delayed breast reconstruction where fat grafting was performed after the radiation treatments in order to improve the local soft tissues prior to placement of an implant (21).
Fat grafting has several potential roles for breast reconstruction patients. It can be used in women who have already undergone an autologous or implant-based reconstruction to add additional volume, correct asymmetries or otherwise fine tune an aesthetic result. Fat grafting can also be a part of the original reconstructive plan to add additional volume and/or a more natural feel to an implant-based reconstruction.
Qureshi et al. looked at 59 patients who underwent 113 implant based reconstructions after NSM. They subsequently performed fat grafting in 24.4% of the DTI patients and 55.6% of the tissue expander patients. On average, each patient underwent one round of fat grafting and the average volume injected was 104 mL for DTI and 73 mL for tissue expander based reconstructions. They administered the BREAST-Q survey 3 months postoperatively and found that fat grafting significantly improved patient satisfaction with their outcome (22).
Fat grafting has more recently been employed as a primary procedure for total breast reconstruction. For patients with inadequate tissue or some other contraindication to autologous reconstruction, who are averse or have had failed prosthetic reconstruction, autologous fat grafting has become a viable option. It has the benefits of no foreign material compared to implant-based reconstructions, and is less invasive than traditional flap-based autologous reconstructions. Fat grafting for total reconstruction can be done as a delayed reconstruction or can be started as an immediate reconstruction. For immediate reconstructions, the fat is injected into the pectoralis muscle, as well as the lateral thoracic fascia and the base of the mastectomy flaps. This can be done under direct vision once the mastectomy is completed. Additional fat grafting treatments can proceed after the mastectomy skin flaps heal and become adherent to the pectoralis muscle (23). Howes et al. describe harvesting 1,000 mL of fat from the abdomen and then injecting 400 mL of filtered fat into the pectoralis major muscle, pectoral fascia and the skin envelope to reconstruct a breast in one stage along with a contralateral reduction for symmetry (24). Panettiere et al. describe a case of failed implant-based reconstruction after NSM, who was not a candidate for general anesthesia due to obesity and severe asthma. A total of 700 mL of fat was injected in nine treatments over the course of 13.5 months. This resulted in an improved aesthetic result as well as improvement in the skin which was damaged from prior radiation treatments (25).
Negative pressure pre-expansion has been advocated by some as a way to increase the amount of fat grafted per session and to have less volume loss in total breast reconstruction cases (23,26). Patient compliance is extremely important to achieving a good result (26,27). Once the skin flaps have healed and become adherent to the muscle (about 4–6 weeks) the expansion process can be started. Additional cycles of expansion and fat grafting can be repeated until the desired breast volume is reached (23).
Khouri et al. looked at 477 patients reconstructed using BRAVA and autologous fat grafting (80 immediate and 397 delayed reconstructions). They found that for delayed reconstruction following mastectomy they required an average of 2.8 procedures for non-irradiated compared to 4.9 procedures for irradiated patients. Immediate reconstruction required slightly fewer procedures averaging 2.1 and 4.2 for non-irradiated and irradiated patients respectively. They injected an average of 225 mL per breast per session, but injected smaller amounts earlier on and increasing amounts once the breast mound became larger. Satisfaction with volume, contour and feel of the breast were very high with 97% of patients being “satisfied” or “very satisfied” with the result (23). BRAVA and fat grafting has resulted in significant improvements in breast volume symmetry, breast contour and breast mound location (27).
Today, large volume fat grafting should be part of every reconstructive surgeon’s treatment plan. Fat grafting is increasingly utilized as a safe and efficacious technique in order to improve the outcomes for patients’ reconstruction of the breast after NSM.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Consent for the images used in this article was obtained.
References
- De La Cruz L, Moody AM, Tappy EE, et al. Overall Survival, Disease-Free Survival, Local Recurrence, and Nipple-Areolar Recurrence in the Setting of Nipple-Sparing Mastectomy: A Meta-Analysis and Systematic Review. Ann Surg Oncol 2015;22:3241-9. [Crossref] [PubMed]
- Colwell AS, Tessler O, Lin AM, et al. Breast reconstruction following nipple-sparing mastectomy: Predictors of complications, reconstruction outcomes, and 5-year trends. Plast Reconstr Surg 2014;133:496-506. [Crossref] [PubMed]
- Dent BL, Miller JA, Eden DJ, et al. Tumor-to-Nipple distance as a predictor of nipple involvement: expanding the inclusion criteria for nipple-sparing mastectomy. Plast Reconstr Surg 2017;140:1e-8e. [Crossref] [PubMed]
- Cohen O, Lam G, Karp N, et al. Determining the Oncologic Safety of Autologous Fat Grafting as a Reconstructive Modality: An Institutional Review of Breast Cancer Recurrence Rates and Surgical Outcomes. Plast Reconstr Surg 2017;140:382e-92e. [Crossref] [PubMed]
- Delay E, Gosset J, Toussoun G, et al. Efficacy of lipomodelling for the management of sequelae of breast cancer conservative treatment. Ann Chir Plast Esthet 2008;53:153-68. [Crossref] [PubMed]
- Stark RY, Mirzabeigi MN, Vonderhaar RJ, et al. Injection technique is performed using a “to and fro” injecting small aliquots into multiple planes of the breast. Asvide 2018;5:531. Available online: http://asvidett.amegroups.com/article/view/25103
- Stark RY, Mirzabeigi MN, Vonderhaar RJ, et al. Needle band release is performed with a skin hook to tension the scar bands and a 16-gauge needle to sharply release the bands. Asvide 2018;5:532. Available online: http://asvidett.amegroups.com/article/view/25104
- Del Vecchio DA, Bucky LP. Breast augmentation using preexpansion and autologous fat transplantation: A clinical radiographic study. Plast Reconstr Surg 2011;127:2441-50. [Crossref] [PubMed]
- Didier F, Radice D, Gandini S, et al. Does nipple preservation in mastectomy improve satisfaction with cosmetic results, psychological adjustment, body image and sexuality? Breast Cancer Res Treat 2009;118:623-33. [Crossref] [PubMed]
- Moyer HR, Ghazi B, Daniel JR, et al. Nipple-Sparing Mastectomy Technical Aspects and Aesthetic Outcomes. Ann Plast Surg 2012;68:446-50. [Crossref] [PubMed]
- Frey JD, Choi M, Salibian AA, et al. Comparison of Outcomes with Tissue Expander, Immediate Implant, and Autologous Breast Reconstruction in Greater Than 1000 Nipple-Sparing Mastectomies. Plast Reconstr Surg 2017;139:1300-10. [Crossref] [PubMed]
- Bucky LP, Percec I. The Science of Autologous Fat Grafting: Views on Current and Future Approaches to Neoadipogenesis. Aesthet Surg J 2008;28:313-21. [Crossref] [PubMed]
- Coleman SR, Saboeiro AP. Fat Grafting to the Breast Revisited: Safety and Efficacy. Plast Reconstr Surg 2007;119:775-85. [Crossref] [PubMed]
- Kaoutzanis C, Xin M, Ballard NS, et al. Outcomes of autologous fat grafting following breast reconstruction in post-mastectomy patients. Plast Reconstr Surg 2014;134:86-7. [Crossref]
- Seth AK, Hirsch EM, Kim JY, et al. Long-Term Outcomes following Fat Grafting in Prosthetic Breast Reconstruction: A Comparative Analysis. Plast Reconstr Surg 2012;130:984-90. [Crossref] [PubMed]
- de Blacam C, Momoh AO, Coakoglu S, et al. Evaluation of Clinical Outcomes and Aesthetic Results after Autologous Fat Grafting for Contour Deformities of the Reconstructed Breast. Plast Reconstr Surg 2011;128:411e-8e. [Crossref] [PubMed]
- Sarfati I, Ihrai T, Kaufman G, et al. Adiposetissue grafting to the post-mastectomy irradiated chest wall: Preparing the ground for implant reconstruction. J Plast Reconstr Aesthet Surg 2011;64:1161-6. [Crossref] [PubMed]
- Serra-Renom JM, Munoz-Olmo JL, Serra-Mestre JM. Fat grafting in postmastectomy breast reconstruction with expanders and prostheses in patients who have received radiotherapy: Formation of new subcutaneous tissue. Plast Reconstr Surg 2010;125:12-8. [Crossref] [PubMed]
- Salgarello M, Visconti G, Barone-Adesi L. Fat grafting and breast reconstruction with implant: Another option for irradiated breast cancer patients. Plast Reconstr Surg 2012;129:317-29. [Crossref] [PubMed]
- Rigotti G, Marchi A, Galie M, et al. Clinical treatment of radiotherapy tissue damage by lipoaspirate transplant: A healing process mediated by adipose-derived adult stem cells. Plast Reconstr Surg 2007;119:1409. [Crossref] [PubMed]
- Salgarello M, Visconti G, Farallo E. Autologous Fat Graft in Radiated Tissue Prior to Alloplastic Reconstruction of the Breast: Report of Two Cases. Aesthetic Plast Surg 2010;34:5-10. [Crossref] [PubMed]
- Qureshi AA, Odom EB, Parikh RP, et al. Patient-Reported Outcomes of Aesthetics and Satisfaction in Immediate Breast Reconstruction After Nipple-Sparing Mastectomy With Implants and Fat Grafting. Aesthet Surg J 2017;37:999-1008. [Crossref] [PubMed]
- Khouri RK, Rigotti G, Khouri RK Jr, et al. Tissue-Engineered Breast Reconstruction with Brava-Assisted Fat Grafting: A 7-Year, 488-Patient, Multicenter Experience. Plast Reconstr Surg 2015;135:643-58. [Crossref] [PubMed]
- Howes BH, Fosh B, Watson DI, et al. Autologous Fat Grafting for Whole Breast Reconstruction. Plast Reconstr Surg Glob Open 2014;2:e124. [Crossref] [PubMed]
- Panettiere P, Accorsi D, Marchetti L, et al. Large-Breast Reconstruction Using Fat Graft Only after Prosthetic Reconstruction Failure. Aesthetic Plast Surg 2011;35:703-8. [Crossref] [PubMed]
- Khouri R, Del Vecchio D. Breast Reconstruction and Augmentation Using Pre –Expansion and Autologous Fat Transplantation. Clin Plast Surg 2009;36:269-80. [Crossref] [PubMed]
- Uda H, Sugawara Y, Sarukawa S, et al. Brava and Autologous Fat Grafting for Breast Reconstruction after Cancer Surgery. Plast Reconstr Surg 2014;133:203-13. [Crossref] [PubMed]