Preputialplasty: can be considered an alternative to circumcision? When, how, why? Experience of Italian centre
Introduction
Phimosis is a condition in which the prepuce cannot be retracted over the glans penis. It is a physiologic and common condition in pediatric age. Pathologic form results from inflammatory or traumatic injury (1-3). The most common treatment of phimosis is circumcision. However, it is not devoid of adverse psychological effects. Many children, indeed, refuse circumcision because they do not accept the possibility to have the exposed glans. For this reason, it is important to process alternative treatment’s options. We describe our experience in correcting phimosis by preputialplasty.
Methods
Between 2015 and 2017 we diagnosed pathological phimosis in 210 patients. All of them were European children. One hundred and two patients had recurrent balanoposthitis (15 of them underwent reduction of paraphimosis in emergency), 43 had painful erections, 50 had urinary discomfort, 15 recurrent urinary tract infections.
The mean age of diagnosis was 8.5 years (range, 2–16 years).
We excluded patients <2 years, with previous preputial surgery.
Of 210 patients, 160 (76.1%) underwent topical steroids cream according to two protocols of our Clinic. Ninety patients applied “fluticasone Propionate Cream 0.05%” twice a day for 3 alternate months. Seventy patients applied “betamethasone 0.05%” twice a day over a 4-week.
Of 210 patients, 185 patients underwent surgery and they have been included in this study.
Twenty-five patients: 11 went to a healing, 14 were lost to follow-up.
One hundred twenty four patients accepted circumcision. Sixty-one underwent preputialplasty (22/balanoposthitis, 18/painful erection, 21/urinary discomfort).
Three outcomes were measured: time of surgery; intraoperative and postoperative complications; cosmetic assessment.
Operative technique
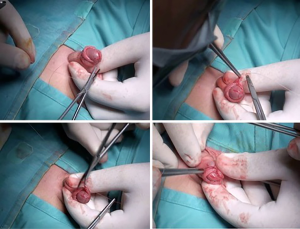
Foreskin was pulled up carefully.
Two markings on the dorsal skin of foreskin are done: an inverted V at the apex of the foreskin and a regular lower V up to a millimeter from the scarring ring. The last one is continuous on the one side and dotted on the other side. The cup on the tip of foreskin is removed and sent to histological exam. Foreskin is incised on the skin along the marked continuous line and on the mucosa along the marked dotted line. By these incisions, the two mucocutaneous flaps of the prepuce are widely separated and then sutured with interrupted Vicryl-Rapide 5-0 stitches. In this way, a dorsal widening of the ring of prepuce is obtained.
Figures 1-6 report all phases of technique. A postoperative dressing involved a gauze around penis with anesthetic ointment (lidocaine).


Results
All patients received general anesthesia with the addition of penile block. They were treated in day surgery. Short-term antibiotic therapy was dispensed before anesthesia induction. Two surgeons performed procedures. The mean operation time was 19 minutes (range, 10–45 minutes).
No intraoperative complications were observed. Early postoperative complications in term of edema and bleeding were present in 23% of patients (14/61) (edema 9/14, bleeding 5/14). One of them 1/14 (7%) underwent surgical revision to stop bleeding.
Long term postoperative complications in term of recurrence of phimosis were present in 3.2% of patients (2/61). All of them were under 3 years. The recurrence was evaluated in a mean of 6 postoperative months. Histological exam showed a lichen sclerosus in 7 patients (11.5%). We purposed a circumcision but all of them refused. One of them is in treatment with urethral dilatation for meatal urethral stenosis from 8 months. The mean follow-up is 14.3 months (range, 2–24 months). All patients underwent three postoperative evaluations: after 1 week, after 1 month and after 6 months. Report each phases of follow up. At last follow-up, 6 months after surgery, all children underwent a cosmetic assessment by a different surgeon.
A valuation of this outcome was done using a modified Hollander wound evaluation scale (WES) that we used before for others studies (3-5). Wound clinical examination is based on: absence of step off, contour irregularities, wound margin separation >2 mm, edge inversion, excessive distortion, and overall cosmetic appearance. Each of these categories was graded on a 0- or l-point scale. A total cosmetic score was derived from the addition of the six categorical variables. A score of 6 was considered optimal, while a score of < or =5 suboptimal. Forty-seven patients (77%) had optimal score and 14 (23%) with suboptimal score.
Discussion
Physiologic phimosis is normal in newborn males. During neonatal development, the prepuce adheres to glans. The inner epithelial lining of the foreskin and the glans are fused. Over time, they spontaneously separate and the foreskin becomes retractile. In a small percentage of children (about 2%) continue to be non-retractability. This is known as pathologic phimosis. It can be due to strong attempts to retract foreskin in physiological phimosis causing bleeding, infection and subsequent scarring, poor hygiene and recurrent balanitis or balanoposthitis (1-3).
The treatment of phimosis can be managed by circumcision or preputialplasty with preservation of the foreskin. This is usually proposed as an alternative especially in Occidental countries in absence of specific conditions as balanitis xerotica obliterans (BXO) that need circumcision.
Over the years many prepuce-saving techniques have been described: V-flap, Z-flap repair, triple incision plasty, limited dorsal slit, multiple Y-V plasty and Triple T (6-15).
In our center, we purpose a limited dorsal Y-V incision that is enough to divide the fibrous ring. It is an easy procedure, with easy learning curve, with satisfactory results and a lower rate of complication. We usually purpose this surgery as alternative to circumcision in selected cases. The ideal patient is a pre-puberal male, with a prepuce no more long, in absence of suspicion of lichen sclerosus, with a good compliance to postoperative retraction of prepuce at least two times per day for a month. We introduced this technique to our Institute in 2010. Previous preputialplasty consisted in a linear dorsal incision that caused a foreskin’s anomalies known as “dog ears”. Many parents complained for these findings. Parents and children usually refuse circumcision because do not accept the possibility to have the exposed glans. The cosmetic satisfaction is the most important aspect of foreskin’s surgery. We retrospectively analyzed our series in term of intraoperative and postoperative outcomes and cosmetic assessment of patients.
About the first outcome, intra and postoperative complications, the poor manipulation of foreskin during surgery ensured fewer complications in term of edema and bleeding. We report indeed 23% of postoperative early complications (edema and bleeding) but only 1 of them (1/61–1.6%) required surgical revision. Two patients (2/61–3.2%) had a recurrence of phimosis. All of them were under 3 years and their compliance of postoperative retraction of prepuce was negative. Cosmetic assessment showed an optimal result in 77% of patients.
There was no difference in term of time of surgery, anesthesia, postoperative pain between this group of patients and patients who underwent circumcisions.
Conclusions
In conclusion, our technique is a good option of preputialplasty. It is a safe, easy and simple to learn. It is a good alternative to circumcision for patients that can’t accept the exposed glans. The main limits of this surgery are related to the absence of compliance of child/family and the presence of lichen sclerosus. In both cases the circumcision can be considered the next choice after 6 months from preputialplasty.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethics Committee Approval was informed but it was no necessary to perform the study, because this is a retrospective descriptive study. Informed consent form, however, was obtained from children’s parents before each procedure. We performed the study without external founds.
References
- Drake T, Rustom J, Davies M. Phimosis in childhood. BMJ 2013;346:f3678. [Crossref] [PubMed]
- Kolehmainen M, Taskinen S, Ossi L. Foreskin surgery. Duodecim 2010;126:75-83. [PubMed]
- Angotti R, Cerchia E, Molinaro F, et al. Circumcision with Glubran(®) 2 in children: experience of Italian Center. Gland Surg 2016;5:391-7. [Crossref] [PubMed]
- Hollander JE, Singer AJ, Valentine S, et al. Wound registry: development and validation. Ann Emerg Med 1995;25:675-85. [Crossref] [PubMed]
- Quinn JV, Drzewiecki AE, Stiell IG, et al. Appearance scales to measure cosmetic outcomes of healed lacerations. Am J Emerg Med 1995;13:229-31. [Crossref] [PubMed]
- Pedersini P, Parolini F, Bulotta AL, et al. "Trident" preputial plasty for phimosis in childhood. J Pediatr Urol 2017;13:278.e1-4. [Crossref] [PubMed]
- Cuckow PM, Rix G, Mouriquand PD. Preputial plasty: a good alternative to circumcision. J Pediatr Surg 1994;29:561-3. [Crossref] [PubMed]
- Emmett AJ. Four V-flap repair of preputial stenosis (phimosis). Plast Reconstr Surg 1975;55:687-9. [Crossref] [PubMed]
- Emmett AJ. Z-plasty reconstruction for preputial stenosis--a surgical alternative to circumcision. Aust Paediatr J 1982;18:219-20. [PubMed]
- Wåhlin N. "Triple incision plasty". A convenient procedure for preputial relief. Scand J Urol Nephrol 1992;26:107-10. [Crossref] [PubMed]
- Holmlund DE. Dorsal incision of the prepuce and skin closure with Dexon in patients with phimosis. Scand J Urol Nephrol 1973;7:97-9. [Crossref] [PubMed]
- Hoffman S, Metz P, Ebbehøj J. A new operation for phimosis: prepuce-saving technique with multiple Y-V-plasties. Br J Urol 1984;56:319-21. [Crossref] [PubMed]
- Dessanti A, Ginesu G, Iannuccelli M, et al. Phimosis. Preputial plasty using transversal widening on the dorsal side with EMLA local anesthetic cream. J Pediatr Surg 2005;40:713-5. [Crossref] [PubMed]
- Fischer-Klein Ch, Rauchenwald M. Triple incision to treat phimosis in children: an alternative to circumcision? BJU Int 2003;92:459-62; discussion 462. [Crossref] [PubMed]
- Nieuwenhuijs JL, Dik P, Klijn AJ, et al. Y-V plasty of the foreskin as an alternative to circumcision for surgical treatment of phimosis during childhood. J Pediatr Urol 2007;3:45-7. [Crossref] [PubMed]





