Surgery for benign thyroid disease in 2018
I read with interest the paper by Ozer Makay “Less than total thyroidectomy for goiter: when and how”, published on Gland Surgery (1).
Certainly, the manuscript is greatly knowledgeable, and rise significant results on surgery for benign thyroid disease in a modern era of more conservative treatment and active surveillance in the endocrine pathology field (1).
Makay contribution to improve quality of endocrine surgery is outstanding (1).
Standardized surgical treatments for benign thyroid disease are safe and satisfactory among experienced surgeons (1).
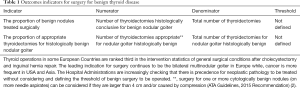
Hospitals Administrations increasingly require outcomes and results indicators (Table 1).
Full table
A better understanding of the clinical characteristics of patients with thyroid nodules is important for preventing complications, improving clinical outcomes, the hospitals auditing and defining thresholds (Table 1).
The thyroid nodule is a common and mostly benign pathology. In the adult population, there is a prevalence of approximately 4–7% of palpable thyroid nodules (3). This prevalence is increased to 10–41% if non-palpated nodules detected by imaging are included (3,4). About 5–10% corresponds to cancers, and is often of excellent prognosis (4). The risk factors for thyroid cancer are age, female sex, pregnancy, iodine deficiency, positive family history and history of cervical irradiation (3-5).
Until now, investigations were recommended for a palpated nodule or in case of accidental discovery of a solid nodule larger than 10 mm and from 5 mm in the case of a positive family history, a history of irradiation or very suspicious ultrasound criteria (3-5). Now, these investigations are proposed for a size greater than 10 mm, regardless of risk factors and ultrasound suspicion, even if it is high (2).
The management of a thyroid nodule begins with the determination of TSH (2). A low value should search for a hot nodule, most commonly benign, and the examination of choice is thyroid scintigraphy (2).
Ultrasonography is the first morphological examination of choice to look for and investigate nodules when the value of TSH is normal or increased, or cold nodules (6). Ultrasound can be used to determine the size and characterize the nodule in solid, mixed or cystic. Standardization of the exam using Thyroid Imaging Reporting and Data System (TI-RADS) assessment categories helps to stratify the risk of thyroid carcinoma for each nodule as well as the course of action (7). It contains a lexical atlas, defining and illustrating terms to describe thyroid nodules in a standardized way, then classifying them according to the degree of suspicion (from 1 to 6, from normal to malignant) (7). Ultrasound criteria for malignancy are hypoechogenicity, size, poorly defined and irregular margins, absence of hypoechoic halo around the periphery, presence of microcalcifications, a larger than high nodule, and cervical lymphadenopathy. The grouping of these criteria makes it possible to categorize the nodule in favor of benignity or malignancy. It is therefore proposed, when the TI-RADS score is greater than 4, to carry out fine needle sampling guided by ultrasound (6,7).
Ultrasound-guided fine needle aspiration (FNA) is used to evaluate the thyroid nodule (2). This technique of good sensitivity is simple, minimally invasive, rapid, and the complications are rare and minor (hematoma at the point of puncture, pain, vagal discomfort). It has improved the selection of patients who are candidates for surgery. Indeed, before the use of FNA, only 14% of resected thyroid nodules were malignant on histology, whereas with a preliminary cytological examination, this proportion rises up to 50% (8,9). The indication for FNA is selected according to the type of nodule (solid, mixed, or cystic), its size and the degree of suspicion evaluated by ultrasound (8,9).
The cytological classification of Bethesda, used since 2008 is an international classification that has standardized the diagnostic criteria and proposes a management of thyroid nodules according to the cytological diagnosis (9,10). There are six categories, each representing a proven level of cancer risk; for each, there is also a proposal for care (9,10).
A prospective study described the fate of an asymptomatic nodule with benign cytology over 5 years (11). Outcomes were growth, diagnosis of cancer (false negative of the initial needle aspiration) and the appearance of new nodules. The inclusion criteria were the presence of one to four thyroid nodules measuring between 0.4 and 4 cm, with either low suspicious criteria for initial thyroid ultrasound or benign cytology (Bethesda II classification) at the puncture site. This is a study comprising 992 patients (with a total of 1,567 nodules), mostly female (82%), with a mean age of 52.4 years, who received regular annual follow-up. ultrasound. The majority of nodules showed no significant change in size or a slight decrease during the 5 years of follow-up. Significant growth of nodules, defined by the American Thyroid Association as a 20% increase in size on two axes, was observed in 15% of patients at 5 years (2). Out of 365 repeated punctures due to a significant increase in size or structural modification of the nodule, cytodiagnosis confirmed mildness in 361 cases. Only five thyroid cancers were diagnosed, accounting for 0.3% of the nodules. As a criticism of this study, we note that it mainly analyzes nodules of small size (less than 1.5 cm), which are often non-evolutive and insignificant; indeed, these do not reflect the size of the nodules that we see in clinic. In addition, the duration of the study is short compared to the generally slow growth of thyroid cancers (11).
Two monocentric studies, one retrospective, the second prospective demonstrated, on the other hand, a higher incidence of thyroid cancer when monitoring initially benign nodules at the puncture site for larger nodules (>3 and 4 cm), and a poorer sensitivity of the puncture (12,13). These studies have certainly many limitations and bias but show a rate ranging from 2% up to 22% for nodules greater than 4 cm long axis, regardless of ultrasound criteria.
Other authors were interested in identifying the best criterion to motivate a new FNA for nodules with initial benign cytology to exclude a false negative (14). This prospective, non-blind, single-center study, published in 2015, included 560 patients, without risk factors for thyroid cancer, between 2009 and 2014. These had an asymptomatic nodule and FNA confirmed the initial benign character. The patients were then divided into four groups according to the degree of suspicion on ultrasound, based on criteria similar to those of TI-RADS (such as marked hypoechogenicity, microcalcifications, microlobulations and irregular margins of the patient nodule, as well as exclusively central vascularization) and growth evaluated by ultrasound follow-up at 6 and 12 months, then annually over 5 years (7). Group A (55 patients), included benign nodules with suspicious ultrasound criteria, group B (82 patients) benign nodules without suspicious ultrasound criteria but significant growth, group C1 (18 patients) benign nodules presenting an ultrasound change and the last, C2 (398 patients), benign nodules without growth. The second FNA was guided by thyroid ultrasound findings and diagnosed with differentiated thyroid cancer in 18.2% of patients in group A, 2.4% of group B and 11% in group C1. No cancer was diagnosed in group C2, which represents the largest group of patients. Subject to the limitations of this study, the initial ultrasound appearance and appearance of ultrasound changes appear to be more predictive of thyroid cancer than nodule growth.
Finally, other authors were interested in the optimal time to repeat the FNA in case of benign nodule and especially the mortality related to this diagnosis (14). The interest of this monocentric and retrospective study is that of an average follow-up of 8.5 years (0.25–18 years) of 1,369 patients of average age of 50 years presenting a nodule with a benign cytology. These were nodules of average size 2.3 cm (1–9.4 cm); there is no precision about the ultrasound data. During follow-up, the authors observed 30 deaths, none related to thyroid cancer. Eighteen cancers were diagnosed after a mean follow-up of 4.5 years (0.3–10 years) after the initial FNA; none had distant metastases (14).
As already mentioned, the recommendations of the Endocrine Society, published in October 2015, now offer investigations for suspicious nodules from the size of 10 mm instead of 5 mm, regardless of the risk factors (2). This is related to the generally mild nature of differentiated thyroid cancers, their excellent prognosis at a localized stage, and their very low mortality. FNA is proposed for nodules with medium to low suspicion, up to 20 mm in size, i.e., for a predominantly cystic spongy nodule.
An ultrasonographic follow-up of the nodule with benign cytology by the specialist is always recommended, but can be adapted according to the degree of suspicion, between 6 and 24 months (2). In the absence of growth or low growth without modification during initial monitoring, it can be spaced (2). For nodules with strong ultrasound suspicion or structural modification, it is necessary to consider a new FNA (2). The sensitivity of this is insufficient for nodules larger than 4 cm and lobectomy remains recommended (5).
Acknowledgements
Thanks for the opportunity to write this letter.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Makay Ö. Less than total thyroidectomy for goiter: when and how? Gland Surg 2017;6:S49-58. [Crossref] [PubMed]
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;26:1-133. [Crossref] [PubMed]
- Hegedüs L. Clinical practice. The thyroid nodule. N Engl J Med 2004;351:1764-71. [Crossref] [PubMed]
- Frates MC, Benson CB, Charboneau JW, et al. Management of thyroid nodules detected at US: Society of Radiologists in Ultrasound consensus conference statement. Radiology 2005;237:794-800. [Crossref] [PubMed]
- Cooper DS, Doherty GM, Haugen BR, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2006;16:109-42. [Crossref] [PubMed]
- Leenhardt L. Management of thyroid nodule. J Radiol 2009;90:354-61. [Crossref] [PubMed]
- Russ G, Bigorgne C, Royer B, et al. The Thyroid Imaging Reporting and Data System (TIRADS) for ultrasound of the thyroid. J Radiol 2011;92:701-13. [Crossref] [PubMed]
- Cibas ES, Ali SZ. NCI Thyroid FNA State of the Science Conference. The Bethesda System For Reporting Thyroid Cytopathology. Am J Clin Pathol 2009;132:658-65. [Crossref] [PubMed]
- Theoharis CG, Schofield KM, Hammers L, et al. The Bethesda thyroid fine-needle aspiration classification system: year 1 at an academic institution. Thyroid 2009;19:1215-23. [Crossref] [PubMed]
- Durante C, Costante G, Lucisano G, et al. The natural history of benign thyroid nodules. JAMA 2015;313:926-35. [Crossref] [PubMed]
- Sohn YM, Kim EK, Moon HJ, et al. Suspiciously malignant findings on ultrasound after fine needle aspiration biopsy in a thyroid nodule with initially benign ultrasound and cytologic result: to repeat or to follow-up. Clin Imaging 2011;35:470-5. [Crossref] [PubMed]
- Wharry LI, McCoy KL, Stang MT, et al. Thyroid nodules (≥4 cm): can ultrasound and cytology reliably exclude cancer? World J Surg 2014;38:614-21. [Crossref] [PubMed]
- Rosário PW, Calsolari MR. What Is the Best Criterion for Repetition of Fine-Needle Aspiration in Thyroid Nodules with Initially Benign Cytology? Thyroid 2015;25:1115-20. [Crossref] [PubMed]
- Nou E, Kwong N, Alexander LK, et al. Determination of the optimal time interval for repeat evaluation after a benign thyroid nodule aspiration. J Clin Endocrinol Metab 2014;99:510-6. [Crossref] [PubMed]


