Less than total thyroidectomy for goiter: when and how?
“You will learn by reading, but you will understand with love.” —Jalaluddin Rumi.
Introduction
Goiter affects almost 6% of the population and is the second most common neck endocrine disease in the World (1,2). Thyroid surgery remains an important option for treating multinodular goiter and therefore is one of the most performed operations by surgeons, especially in endemic areas. The surgical management of such cases aims to treat the goiter with low morbidity and low recurrence rate.
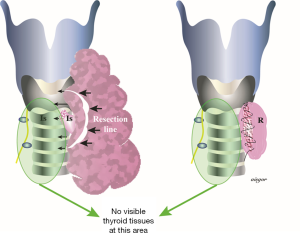
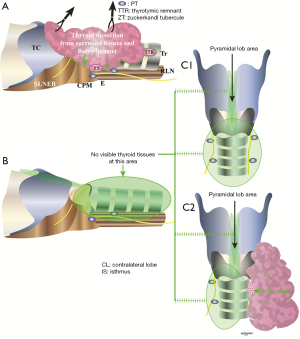
Thyroidectomy for benign goiter has been accepted as a safe treatment believed to have low surgical risk. Nowadays, death related to thyroid surgery is extremely rare. There remains controversy regarding what type of surgery is superior for this benign disease (3). Previously, subtotal thyroidectomy (Figure 1) was considered the gold standard treatment because of its lower complication rates and reduced requirement for life-long hormone replacement therapy (4,5). However, an increased recurrence rates up to 43% may be expected after subtotal thyroidectomy (6). For this reason, current guidelines and meta-analysis recommend total thyroidectomy for both toxic and non-toxic benign multinodular goiter (7,8). Most centers have adopted total and/or near total thyroidectomy (Figure 2) and reported low morbidity rates similar to the subtotal procedure. Meanwhile, the number of publications related to postoperative parathyroid failure after total thyroidectomy has been steadily climbing in recent years and many of patients included in these cohort studies had surgery for benign goiter (1,9,10). This is the reason why it is felt the time is ripe for an in-depth review on this specific topic and various surgical methods that impact on morbidity after goiter surgery will be discussed.

Limits of resection and outcomes of surgery for goiter
Indications for surgery in patients with goiter include suspected malignancy, substernal extension, hyperthyroidism resistant to medical therapy or obstructive symptoms (i.e., dysphagia or shortness of breath). Cosmetic concerns are rarely the reason for carrying out surgery. Limits of resection for thyroid surgery in goiter have changed over years.
Enucleation of nodules or subtotal unilateral lobectomy was abandoned in the 1980s and has no place in current surgical practice.
Subtotal thyroidectomy for benign multinodular goiter had been accepted as standard of management until the end of the 20th century. There was an acknowledged variation between centers with regard to the size and location of the remnant thyroid tissue. Potentially, this led to heterogeneity of outcomes hindering reliable scientific assessment of the efficacy of this technique.
The Dunhill procedure, i.e., hemithyroidectomy plus subtotal resection of the contralateral thyroid lobe, has been suggested as an alternative option compromising between radical surgery and prevention of complications (Figure 3). This may overcome the concern of recurrence or completion surgery for an incidentally discovered thyroid cancer (11). A prospective, randomized two-armed study, Rayes and colleagues compared subtotal resection and the Dunhill procedure in the management of benign multinodular goiter. There were no significant differences in terms of incidence of complications (12). Thomusch and colleagues reported the results of a quality assurance study of goiter, where 5,195 patients treated for benign goiter by primary bilateral resection were assessed. With respect to the extent of resection, three groups were analyzed: bilateral subtotal resection, subtotal resection with contralateral lobectomy (Dunhill procedure) and total thyroidectomy. The postoperative morbidity increased with the extent of resection. The rate of permanent recurrent laryngeal nerve palsy was 0.8% for bilateral subtotal thyroidectomy, 1.4% for Dunhill procedure, and 2.3% for total thyroidectomy. Permanent hypoparathyroidism occurred in 1.5% following subtotal resection, in 2.8% after Dunhill procedure, and 12.5% after total thyroidectomy. Multivariate analysis showed that the extent of resection significantly increased the risk of recurrent laryngeal nerve palsy and hypoparathyroidism. Additionally, the development of permanent hypoparathyroidism was reduced if at least two parathyroid glands were identified. This study provided evidence of total thyroidectomy resulting in higher risk of recurrent laryngeal nerve palsy and hypoparathyroidism, when compared to subtotal resection and Dunhill procedure (13).
Lobectomy plus isthmectomy for uninodular goiter and (near) total thyroidectomy for multinodular goiter were recommended by the updated AACE/ACE/AME guidelines (8). Most of the reported studies in the literature consist of retrospective data from single-centers, leading to difficulty in making strong recommendations regarding management of the bilateral multinodular goiter patient. These single-center studies reported very low permanent complications (1%) after total thyroidectomy carried out for bilateral multinodular goiter, emphasizing the role of experience in such cases (14,15). Overall, between 2% and 12% of patients undergoing total thyroidectomy develops permanent hypoparathyroidism, according national registries and large multicenter studies (16).
What is the evidence in favor of total thyroidectomy?
An evidence-based review by Moalem and colleagues identified 13 studies (8 comparative and 3 prospective controlled studies) in 2008, in which they also questioned complications after various types of surgeries for benign nodular goiter. The frequency of temporary and permanent recurrent laryngeal nerve palsy did not differ between procedures. This was also true for permanent hypoparathyroidism, even there was a remarkable increase in transient hypoparathyroidism after total thyroidectomy. As a result, total thyroidectomy was recommended as the procedure of choice for benign multinodular goiter (2). In the retrospective study of Rudolph and colleagues, total thyroidectomy was demonstrated to be safe and efficacious, especially with the aid of technological advancements like vessel sealing systems and intraoperative nerve monitoring (9). Alongside this, concerns raise due to the thermal spread of the recent vessel sealing systems, which may harm the parathyroid tissue, as well as the recurrent laryngeal nerve. Moreover, it is still not proved that the use of intraoperative nerve monitoring decreases the rates of recurrent laryngeal nerve injury during thyroid surgery (17).
What is the evidence in favor of less-than-total thyroidectomy?
In contrast with these encouraging results, a prospective randomized study, Erbil and colleagues reported significantly higher transient hypocalcemia rates after total thyroidectomy in benign multinodular goiter, when compared to near-total thyroidectomy. The incidence of transient hypoparathyroidism was 26% in the total thyroidectomy group, while it was 9.8% in the near-total thyroidectomy group (18). A recent meta-analysis of four randomized trials showed limited information regarding evidence on total thyroidectomy compared with subtotal thyroidectomy. In this Cochrane review, goiters recurred in 0.2% of the total thyroidectomy group compared to 8.4% of the subtotal thyroidectomy group, where the difference was significant. Meanwhile, reoperation was necessary in only 0.8% of subtotal thyroidectomy cases. The incidence of recurrent laryngeal nerve palsy was found to be higher in the total thyroidectomy group. This was also the case for permanent hypoparathyroidism (19). Another study reported by Hauch et al. suggested that total thyroidectomy has higher associated risks of complications compared to hemithyroidectomy (20.4% vs. 10.8%, respectively). They also added that this is true even for the high-volume surgeon and interestingly more than half of the complications (56.4%) occurred after operations for benign disease (20).
Some results regarding comparison between operative methods for benign goiter are summarized in Table 1.

Full table
Post-thyroidectomy hypoparathyroidism—the new driving force for change?
Hypoparathyroidism has a negative impact on the quality of life of the patients. Patients suffer from lifelong therapy, re-admissions to the hospital, disabilities to perform household activities and poor quality of life (24). The risk of permanent hypoparathyroidism after total thyroidectomy has been underestimated. Lorente-Poch and colleagues defined possible reasons for the underestimation of the prevalence of hypoparathyroidism in their review (16). These reasons are lack of clear definitions, conflict of interest, variety of laboratory ranges for normocalcemia and reference values, timing of blood sampling in the postoperative period, wide range in thyroid procedures included in the analysis, heterogeneity of included cases, small series, missing data in national audits, different policies for calcium and vitamin D supplements, short or incomplete follow-up and follow-up not performed by the surgical team but be referring physicians. This review, which concentrates on parathyroid failure after total thyroidectomy, pointed out that the rate of permanent hypoparathyroidism from national registries and large multicenter studies was much higher than those reported from single-center studies, ranging from 6% to 12% (16). In the setting of total thyroidectomy, inadvertent parathyroid excision and parathyroid autotransplantation increases the risk of hypoparathyroidism (25). Autotransplantation may not be a solution for preventing permanent hypoparathyroidism. This was well documented in some series (25,26). On the contrary, there are also studies supporting the possible preventive effect of autotransplantation on the risk of permanent hypoparathyroidism (27,28). The number of parathyroid glands remaining in situ after thyroidectomy is of crucial importance in maintaining calcium homeostasis in the immediate postoperative period (25).
There is an agreement that the risk of permanent hypocalcaemia is much lower after bilateral subtotal thyroidectomy and Dunhill procedure (13,29). In another multi-center audit comprising 1,385 total thyroidectomy patient, 18% received treatment for hypoparathyroidism, 6 weeks after surgery (30).
In a retrospective cohort study, Lin and colleagues compared four different operative methods (total thyroidectomy, Dunhill procedure, bilateral subtotal thyroidectomy and unilateral thyroidectomy) for multinodular goiter. Regarding morbidity, only transient hypoparathyroidism was found to be significantly increased in the total thyroidectomy group (25.3%). As expected, recurrence rate was the highest in the bilateral subtotal thyroidectomy group (21.6%), but only 1.8% required a reoperation. In this series, among patients who underwent reoperation for goiter recurrence, permanent hypoparathyroidism was observed in 20% (n=2) of cases (21). Concerning Mauriello et al.’s review, published in 2016, 3 randomized controlled trials and 18 retrospective studies were analyzed to compare different surgical approaches for the treatment of benign multinodular goiter. According to this review, Dunhill procedure resulted in fewer complications, better functional status and a non-surgical risk of recurrence, as long as thyroid hormone substitution was continued after surgery in order to prevent recurrence (31).
Need for completion thyroidectomy due to incidental PTC—rarely a problem
Although total thyroidectomy may avoid recurrence and the need for completion thyroidectomy due to incidentally found cancers, this radical approach may increase the risk of iatrogenic injury (32). Besides, it is worth to mention that completion thyroidectomy is rarely required, since 60% to 80% of these cancers are papillary micro carcinomas where hemithyroidectomy is sufficient (33). Thus, in practice, second operations are rarely needed in multinodular goiter patients when a cancer has been discovered incidentally. The possibility of an incidentally found carcinoma is 5–15% of all surgeries for goiter (2,34).
Is subtotal thyroidectomy an option?
Thirty years ago, most of the goiter cases underwent bilateral subtotal thyroidectomy at our institution, Ege University Hospital. However, during long term follow-up after subtotal thyroidectomy in multinodular disease we realized that 29% of these cases developed recurrence (1). The need for a re-operative surgery in some of these cases was becoming a burden, due to expected increased complication rates. After years, the practice changed from bilateral subtotal thyroidectomy to total thyroidectomy. The expectation was the reduction of risk of recurrence, but this type of surgery resulted in higher risk of hypoparathyroidism (1).
Although the role of subtotal thyroidectomy in the management of the multinodular goiter has significantly decreased with the reported safety of total thyroidectomy, it is still in common practice in several centers worldwide (12). This is true for endemic and non-endemic countries. Those authors who favor subtotal resection in benign disease emphasize increased rates of recurrent laryngeal nerve and parathyroid injury. On the other hand, a lifelong hormone replacement therapy has also been questioned in patients receiving a total resection (35,36). However, during long term follow-up of the subtotal resected patients, it was obvious that the subtotal thyroidectomy procedure was related to increased recurrence rates (1). Multinodular goiter itself is accepted as a significant risk factor for recurrence in patients undergoing thyroid surgery else than total thyroidectomy (37). The risk of recurrence was reported in up to 78% of patients (38). Two meta-analyses, reporting recurrence rates from 0% to 50% after subtotal resection of the thyroid gland, have been criticized according different definitions of recurrence, different follow-up periods, and the lack of technical description of surgery. Most data rose from retrospective studies (2,29). It is worth to mention that a 30-year follow-up is required for actual recurrence rates after subtotal thyroidectomy (36).
A recent meta-analysis comparing total thyroidectomy and bilateral subtotal thyroidectomy for bilateral multinodular nontoxic goiter, reported higher risk of postoperative transient hypocalcemia and lower rate of recurrence after total thyroidectomy. Although being the first meta-analysis of randomized clinical trials comparing the results of total thyroidectomy and bilateral subtotal thyroidectomy, selection bias and having no standard definition of recurrence were the pitfalls of this review (39). In a recently published systematic review, although reporting an increased rate of transient hypocalcemia, total thyroidectomy was reported to be superior to subtotal thyroidectomy due to the increased risk of recurrence of disease and risk of leaving few traces of inadequately treated thyroid cancers after subtotal thyroidectomy (40). The important difficulty of subtotal thyroidectomy is that we may pass over the risk of a possible nodular process left behind in the remnant lobe. Karakoyun and colleagues evaluated pathological findings in the remnant lobe after near total and subtotal thyroidectomy. The results showed that more than a half of the residual tissue had pathological findings. More importantly, these pathological findings, benign and malignant, did not differ between the two surgical procedures (62% for subtotal resection and 56% for near total resection) (41).
Defenders of subtotal thyroidectomy claim that surgery is warranted in not more than 4% of recurred cases (42-44). Our rate of clinical recurrence requiring surgery in cases undergoing subtotal resection lies just above this range, in other words 5% (1). However, there are also studies reporting reoperation rates from 5% to 26% (1,45,46). Gibelin et al. previously showed that multinodular goiter is a highly significant risk factor for recurrence in benign thyroid disease where a less than total thyroidectomy was performed (37). Thus, after subtotal thyroidectomy, if a nodule-free tissue remains behind and thyroid hormone replacement therapy is prescribed for recurrence prophylaxis, only about 0–0.5% of patients will undergo a reoperation for recurrent goiter (11).
Some cases may need further surgical treatment after subtotal thyroidectomy, due to incidentally found follicular cancers and multicentric or large papillary cancers. This may be evident in nearly one third of subtotal thyroidectomized cases (39). On the contrary, based on results of two prospective trials, incidental cancers may be rare and no carcinoma may be discovered at all (12,47). Nevertheless, in a study by Giles and colleagues, the need for a completion thyroidectomy was as low as 3.5% of bilateral multinodular goiter patients (48). This was similar to the rate of completion thyroidectomy after bilateral subtotal surgery (3.68%) reported in another randomized controlled study (49).
Reoperations are associated with higher morbidity rates, when compared to primary operations (15) due to the distortion of the central neck anatomy. Rudolph et al. demonstrated a significantly increased risk of permanent recurrent laryngeal nerve injury and hypoparathyroidism following previous subtotal thyroidectomy when compared to previous unilateral thyroidectomy (9). Recurrence may arise from the remnant posterolateral tissue that extends into the retrotracheal and retroesophageal areas. This may be another reason for the increase of complexity of surgery, resulting in increased complication rates (50). On the other hand, we demonstrated that reoperations could still be performed with minimal morbidity. In our series, no permanent recurrent laryngeal nerve injury occurred and a permanent hypoparathyroidism rate of 1.6% was achieved in reoperations for thyroid cancer (51).
Complication rates are especially higher after total thyroidectomy when the surgery has been performed by surgeons who are not specialized in endocrine surgery (52). It is important to mention that nearly half of the thyroidectomies are performed in low-volume centers throughout the USA and Europe (49). The principal risk of total thyroidectomy relates to the recurrent laryngeal nerve and more importantly to the parathyroid glands and their blood supply. Grant emphasized that it would be risky to consider total thyroidectomy as the only acceptable alternative in the treatment of benign thyroid disease, as this would risk causing more cases of troublesome hypoparathyroidism than it would prevent cases of goiter recurrence (53).
Unilateral thyroid lobectomy: when?
Multinodular goiter limited to only one lobe is a rare clinical situation and for such patients’ hemithyroidectomy is indicated. This has been recommended in the meta-analysis of Li and colleagues (39). A one-side surgery will avoid the need for a life-long L-thyroxine treatment, and in case of a recurrence, the patient will not suffer from increased complication rates due to re-do surgery of the opposite lobe, since this contralateral lobe has been left untouched during the primary surgery. It is important to note that only 12% of patients suffer from recurrence after a previous unilateral thyroidectomy (54). Meanwhile, between 14–30% of patients undergoing unilateral surgery may require L-thyroxine treatment in the postoperative period to prevent hypothyroidism (22,55).
Unilateral multinodularity is a risk factor for recurrence of the disease in the remaining lobe (56). According to the study of Bellantone and colleagues, one third of patients receiving unilateral surgery had shown recurrence after a mean follow-up of 80 months (57). In a study by Barbier and colleagues, 36% of patients diagnosed with a single nodule during the preoperative work-up were reported to have a multinodular formation post-surgery (58). However, whether these small nodules have any clinical pertinence is an issue that is worth to be discussed (53).
Compared to bilateral subtotal thyroidectomy, previous unilateral thyroid lobectomy, is associated with a 5-fold decrease in complications after re-operative surgery (6,59). Sancho and colleagues compared two different surgical techniques—hemithyroidectomy vs. Dunhill procedure—for the surgical management of multinodular goiter in a multicenter and randomized study. They recruited 118 patients from 6 centers. The rate of transient hypoparathyroidism was higher in the group undergoing Dunhill procedure, but no patient developed permanent hypoparathyroidism (22). Bauer and colleagues reported similar permanent complications in their short-term follow-up study of benign multinodular goiter cases undergoing unilateral or bilateral total thyroidectomy, although transient hypoparathyroidism was higher in the bilateral resection group (23). This was also the case in another study by Olson and colleagues, where patients were followed up for 134 months. In the latter study, the authors expressed that in selected patients with unilateral disease, unilateral thyroid lobectomy would be the procedure of choice for multinodular goiter. Although the recurrence rate was higher in the lobectomy group (11% vs. 3%), in patients undergoing reoperation for recurrence, the rates of complications were similar to that of initial surgery (60).
Regarding re-operative surgery in these cases, Vasica and colleagues demonstrated that most re-operative surgery has been a unilateral thyroidectomy, following a previous lobectomy (61). Furthermore, there is a body of literature reporting a role for unilateral thyroidectomy in cases with bilateral multinodular goiter with minimal multinodular formation on the contralateral lobe (60,62).
Most of the cases undergoing unilateral thyroid surgery did not require further surgery or hormone supplementation to maintain a euthyroid state. Even some cases undergo a reoperation, which can be performed without an increase in complication rates.
Conclusions
The debate continues regarding the type of surgery in benign multinodular goiter. Lobectomy should be the choice for symptomatic unilateral multinodular goiter. For bilateral disease the choice is between subtotal thyroidectomy, condemned for its recurrence rate, and total thyroidectomy, condemned for its high percentage of postsurgical complications. The published outcome data has a low level of evidence but there is enough evidence to show that the rate of transient and permanent hypoparathyroidism rises in correlation with the extent of thyroidectomy. Individualizing the extent of surgery for goiter based on extent of disease, surgical expertise, social and economic issues related to the need for life-long thyroxine replacement therapy and patients’ choice should allow a favorable outcome for the vast majority of patients with benign multinodular goiter (Table 2).

Full table
Acknowledgements
I would like to gratefully and sincerely thank Dr. Adnan Isgor for his wonderful illustrations and Dr. Radu Mihai for his support for proofreading.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare
References
- Yoldas T, Makay O, Icoz G, et al. Should subtotal thyroidectomy be abandoned in multinodular goiter patients from endemic regions requiring surgery? Int Surg 2015;100:9-14. [Crossref] [PubMed]
- Moalem J, Suh I, Duh QY. Treatment and prevention of recurrence of multinodular goiter: an evidence-based review of the literature. World J Surg 2008;32:1301-12. [Crossref] [PubMed]
- Ozbas S, Kocak S, Aydintug S, et al. Comparison of the complications of subtotal, near total and total thyroidectomy in the surgical management of multinodular goitre. Endocr J 2005;52:199-205. [Crossref] [PubMed]
- Torre G, Barreca A, Borgonovo G, et al. Goiter recurrence in patients submitted to thyroid-stimulating hormone suppression: possible role of insulin-like growth factors and insulin-like growth factor-binding proteins. Surgery 2000;127:99-103. [Crossref] [PubMed]
- Barbier J, Kraimps JL. Comments on the prevention of recurrence with thyroid hormone therapy. Ann Endocrinol (Paris) 1993;54:291-2. [PubMed]
- Röjdmark J, Järhult J. High long term recurrence rate after subtotal thyroidectomy for nodular goitre. Eur J Surg 1995;161:725-7. [PubMed]
- Ross DS, Burch HB, Cooper DS, et al. 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid 2016;26:1343-421. [Crossref] [PubMed]
- Gharib H, Papini E, Garber JR, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules-2016 update. Endocr Pract 2016;22:622-39. [Crossref] [PubMed]
- Rudolph N, Dominguez C, Beaulieu A, et al. The morbidity of reoperative surgery for recurrent benign nodular goitre: Impact of previous unilateral thyroid lobectomy versus subtotal thyroidectomy. J Thyroid Res 2014;2014:231857. [PubMed]
- Dralle H, Lorenz K, Machens A. State of the art: surgery for endemic goiter—a plea for individualizing the extent of resection instead of heading for routine total thyroidectomy. Langenbecks Arch Surg 2011;396:1137-43. [Crossref] [PubMed]
- Rayes N, Seehofer D, Neuhaus P. The surgical treatment of bilateral benign nodular goiter: balancing invasiveness with complications. Dtsch Arztebl Int 2014;111:171-8. [PubMed]
- Rayes N, Steinmüller T, Schröder S, et al. Bilateral subtotal thyroidectomy versus hemithyroidectomy plus subtotal resection (Dunhill procedure) for benign goiter: long-term results of a prospective, randomized study. World J Surg 2013;37:84-90. [Crossref] [PubMed]
- Thomusch O, Sekulla C, Dralle H. Is primary total thyroidectomy justified in benign multinodular goiter? Results of a prospective quality assurance study of 45 hospitals offering different levels of care. Chirurg 2003;74:437-43. [Crossref] [PubMed]
- Zambudio AR, Rodríguez J, Riquelme J, et al. Prospective study of postoperative complications after total thyroidectomy for multinodular goiters by surgeons with experience in endocrine surgery. Ann Surg 2004;240:18-25. [Crossref] [PubMed]
- Delbridge L, Guinea AI, Reeve TS. Total thyroidectomy for bilateral benign multinodular goiter: effect of changing practice. Arch Surg 1999;134:1389-93. [Crossref] [PubMed]
- Lorente-Poch L, Sancho JJ, Muñoz-Nova JL, et al. Defining the syndromes of parathyroid failure after total thyroidectomy. Gland Surg 2015;4:82-90. [PubMed]
- Yang S, Zhou L, Lu Z, et al. Systematic review with meta-analysis of intraoperative neuromonitoring during thyroidectomy. Int J Surg 2017;39:104-13. [Crossref] [PubMed]
- Erbil Y, Barbaros U, Salmaslioğlu A, et al. The advantage of near-total thyroidectomy to avoid postoperative hypoparathyroidism in benign multinodular goiter. Langenbecks Arch Surg 2006;391:567-73. [Crossref] [PubMed]
- Cirocchi R, Trastulli S, Randolph J, et al. Total or near-total thyroidectomy versus subtotal thyroidectomy for multinodular non-toxic goitre in adults. Cochrane Database Syst Rev 2015.CD010370. [PubMed]
- Hauch A, Al-Qurayshi Z, Randolph G, et al. Total thyroidectomy is associated with increased risk of complications for low- and high-volume surgeons. Ann Surg Oncol 2014;21:3844-52. [Crossref] [PubMed]
- Lin YS, Wu HY, Yu MC, et al. Patient outcomes following surgical management of multinodular goiter: Does multinodularity increase the risk of thyroid malignancy? Medicine (Baltimore) 2016;95:e4194. [Crossref] [PubMed]
- Sancho JJ, Prieto R, Dueñas JP, et al. A randomized trial of hemithyroidectomy versus Dunhill for the surgical management of asymmetrical multinodular goiter. Ann Surg 2012;256:846-51. [Crossref] [PubMed]
- Bauer PS, Murray S, Clark N, et al. Unilateral thyroidectomy for the treatment of benign multinodular goiter. J Surg Res 2013;184:514-8. [Crossref] [PubMed]
- Hadker N, Egan J, Sanders J, et al. Understanding the burden of illness associated with hypoparathyroidism reported among patients in the PARADOX study. Endocr Pract 2014;20:671-9. [Crossref] [PubMed]
- Sitges-Serra A, Ruiz S, Girvent M, et al. Outcome of protracted hypoparathyroidism after total thyroidectomy. Br J Surg 2010;97:1687-95. [Crossref] [PubMed]
- Pattou F, Combemale F, Fabre S, et al. Hypocalcemia following thyroid surgery: incidence and prediction of outcome. World J Surg 1998;22:718-24. [Crossref] [PubMed]
- Olson JA Jr, DeBenedetti MK, Baumann DS, et al. Parathyroid autotransplantation during thyroidectomy. Results of long-term follow-up. Ann Surg 1996;223:472-8. [Crossref] [PubMed]
- Almquist M, Hallgrimsson P, Nordenström E, et al. Prediction of permanent hypoparathyroidism after total thyroidectomy. World J Surg 2014;38:2613-20. [Crossref] [PubMed]
- Agarwal G, Aggarwal V. Is total thyroidectomy the surgical procedure of choice for benign multinodular goiter? An evidence-based review. World J Surg 2008;32:1313-24. [Crossref] [PubMed]
- Bergenfelz A, Jansson S, Kristoffersson A, et al. Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3,660 patients. Langenbecks Arch Surg 2008;393:667-73. [Crossref] [PubMed]
- Mauriello C, Marte G, Canfora A, et al. Bilateral benign multinodular goiter: What is the adequate surgical therapy? A review of literature. Int J Surg 2016;28:S7-12. [Crossref] [PubMed]
- Thomusch O, Machens A, Sekulla C, et al. Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: prospective multicenter study in Germany. World J Surg 2000;24:1335-41. [Crossref] [PubMed]
- Mercante G, Frasoldati A, Pedroni C, et al. Prognostic factors affecting neck lymph node recurrence and distant metastasis in papillary microcarcinoma of the thyroid: results of a study in 445 patients. Thyroid 2009;19:707-16. [Crossref] [PubMed]
- Friguglietti CU, Lin CS, Kulcsar MA. Total thyroidectomy for benign thyroid disease. Laryngoscope 2003;113:1820-6. [Crossref] [PubMed]
- Bononi M, de Cesare A, Atella F, et al. Surgical treatment of multinodular goiter: incidence of lesions of the recurrent nerves after total thyroidectomy. Int Surg 2000;85:190-3. [PubMed]
- Anderson PE, Hurley PR, Rosswick P. Conservative treatment and long term prophylactic thyroxine in the prevention of recurrence of multinodular goiter. Surg Gynecol Obstet 1990;171:309-14. [PubMed]
- Gibelin H, Sierra M, Mothes D, et al. Risk factors for recurrent nodular goiter after thyroidectomy for benign disease: case-control study of 244 patients. World J Surg 2004;28:1079-82. [Crossref] [PubMed]
- Miccoli P, Antonelli A, Iacconi P, et al. Prospective, randomized, double-blind study about effectiveness of levothyroxine suppressive therapy in prevention of recurrence after operation: result at the third year of follow-up. Surgery 1993;114:1097-101. [PubMed]
- Li Y, Li Y, Zhou X. Total thyroidectomy versus bilateral subtotal thyroidectomy for bilateral multinodular nontoxic goiter: a meta-analysis. ORL J Otorhinolaryngol Relat Spec 2016;78:167-75. [Crossref] [PubMed]
- Padur AA, Kumar N, Guru A, et al. Safety and effectiveness of total thyroidectomy and its comparison with subtotal thyroidectomy and other thyroid surgeries: a systematic review. J Thyroid Res 2016;2016:7594615. [PubMed]
- Karakoyun R, Bülbüller N, Koçak S, et al. What do we leave behind after neartotal and subtotal thyroidectomy: just the tissue or the disease? Int J Clin Exp Med 2013;6:922-9. [PubMed]
- Cohen-Kerem R, Schachter P, Sheinfeld M, et al. Multinodular goiter: the surgical procedure of choice. Otolaryngol Head Neck Surg 2000;122:848-50. [Crossref] [PubMed]
- Kraimps JL, Marechaud R, Gineste D, et al. Analysis and prevention of recurrent goiter. Surg Gynecol Obstet 1993;176:319-22. [PubMed]
- Lasagna B. Subtotal thyroidectomy, the preferred option for eu- and hyperthyroid goitre. Panminerva Med 1994;36:22-4. [PubMed]
- Marchesi M, Biffoni M, Tartaglia F, et al. Total versus subtotal thyroidectomy in the management of multinodular goiter. Int Surg 1998;83:202-4. [PubMed]
- Yang W, Shao T, Ding J, et al. The feasibility of total or near-total bilateral thyroidectomy for the treatment of bilateral multinodular goiter. J Invest Surg 2009;22:195-200. [Crossref] [PubMed]
- Pappalardo G, Guadalaxara A, Frattaroli FM, et al. Total compared with subtotal thyroidectomy in benign nodular disease: personal series and review of published reports. Eur J Surg 1998;164:501-6. [Crossref] [PubMed]
- Giles Y, Boztepe H, Terzioglu T, et al. The advantage of total thyroidectomy to avoid reoperation for incidental thyroid cancer in multinodular goiter. Arch Surg 2004;139:179-82. [Crossref] [PubMed]
- Barczyński M, Konturek A, Hubalewska-Dydejczyk A, et al. Five-year follow-up of a randomized clinical trial of total thyroidectomy versus Dunhill operation versus bilateral subtotal thyroidectomy for multinodular nontoxic goiter. World J Surg 2010;34:1203-13. [Crossref] [PubMed]
- Colak T, Akca T, Kanik A, et al. Total versus subtotal thyroidectomy for the management of benign multinodular goiter in an endemic region. ANZ J Surg 2004;74:974-8. [Crossref] [PubMed]
- Makay O, Unalp O, Icoz G, et al. Completion thyroidectomy for thyroid cancer. Acta Chir Belg 2006;106:528-31. [Crossref] [PubMed]
- Reeve TS, Curtin A, Fingleton L, et al. Can total thyroidectomy be performed as safely by general surgeons in provincial centers as by surgeons in specialized endocrine surgical units? Making the case for surgical training. Arch Surg 1994;129:834-6. [Crossref] [PubMed]
- Grant CS. Invited critique: total thyroidectomy for bilateral benign multinodular goiter. Arch Surg 1999;132:1393. [Crossref]
- Wadström C, Zedenius J, Guinea A, et al. Multinodular goitre presenting as a clinical single nodule: how effective is hemithyroidectomy? Aust N Z J Surg 1999;69:34-6. [Crossref] [PubMed]
- Stoll SJ, Pitt SC, Liu J, et al. Thyroid hormone replacement after thyroid lobectomy. Surgery 2009;146:554-8. [Crossref] [PubMed]
- La Gamma A, Letoquart JP, Kunin N, et al. Predictive factors of nodular recurrence after thyroidectomy for goiter. J Chir (Paris) 1994;131:66-72. [PubMed]
- Bellantone R, Lombardi CP, Boscherini M, et al. Predictive factors for recurrence after thyroid lobectomy for unilateral non-toxic goiter in an endemic area: results of a multivariate analysis. Surgery 2004;136:1247-51. [Crossref] [PubMed]
- Barbier J, Kraimps JL, Sudre Y, et al. Nodular recurrence after thyroid surgery, excluding cancer. Chirurgie 1985;111:119-23. [PubMed]
- Reeve TS, Delbridge L, Brady P, et al. Secondary thyroidectomy: a twenty-year experience. World J Surg 1988;12:449-53. [Crossref] [PubMed]
- Olson SE, Starling J, Chen H. Symptomatic benign multinodular goiter: unilateral or bilateral thyroidectomy? Surgery 2007;142:458-61. [Crossref] [PubMed]
- Vasica G, O'Neill CJ, Sidhu SB, et al. Reoperative surgery for bilateral multinodular goitre in the era of total thyroidectomy. Br J Surg 2012;99:688-92. [Crossref] [PubMed]
- Phitayakorn R, Narendra D, Bell S, et al. What constitutes adequate surgical therapy for benign nodular goiter? J Surg Res 2009;154:51-5. [Crossref] [PubMed]