Complications from tracheal resection for thyroid carcinoma
Introduction
The invasion of upper aero-digestive tract from thyroid cancer is not uncommon, occurring in 6–13% of patients (1). Thyroid cancer extended to trachea has poor prognosis compared to tumors limited to the thyroid gland and its management as the extent of resection are still debated. However, thyroidectomy associated to en bloc tracheal resection with end-to-end anastomosis is universally accepted to achieve tumor local control. The complete resection of local disease has been reported to provide the longest survival and the best palliation but it is related to a sensible postoperative morbidity rate. Thus, patients’ selection, careful preoperative tracheal evaluation and accurate surgical technique are mandatory to reduce postoperative morbidity and mortality.
The present review aims to discuss the complications of en-bloc tracheal resection with end-to-end anastomosis for thyroid cancer.
Methods
The search was performed using PubMed (National Center for Biotechnology Information, U.S. National Library of Medicine; 8600 Rockville Pike, Bethesda MD, 20894 USA) through an overarching for the following terms: “complication of tracheal resection [AND] invasive thyroid cancer”.
Results
Tracheal invasion from thyroid cancer occurs in 4% to 23% of patients and only the 0.5% to 1.5% cases the tumor involves the tracheal wall, getting into the tracheal lumen (2-4). The possible tracheal infiltration form thyroid cancer is generally assessed during the preoperative investigations but sometimes it is discovered during the surgical procedure (2-4).
Tracheal resection for thyroid cancer aims to obtain a complete excision of the neoplasm and to accomplish the loco-regional tumor control. Different surgical techniques can be performed to achieve the en bloc resection of the thyroid tumor invading the trachea as tracheal shave excision, full-thickness tracheal window resection and tracheal sleeve resection with end-to-end anastomosis. The choice of one of these techniques depends on tumor histology and its extent through tracheal wall.
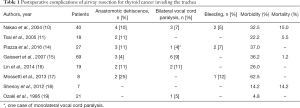
Tracheal sleeve resection with end-to-end anastomosis is the treatment of choice for thyroid cancer invading tracheal wall since it allows an oncologically complete local resection with an overall 5-year survival rate greater than 80% (5-13). However, the postoperative complications are not negligible, ranging from 15% to 39%, and the postoperative mortality is 1.2% (14,15). The most common postoperative complications are: anastomotic dehiscence, airway stenosis, infections and bleeding (Table 1). We include for completeness the tumor local recurrence as a late on-set complication.
Full table
Anastomotic dehiscence
Anastomotic dehiscence is one of the most fearful complications since it is a life-threatening condition and it can occur in all kind of tracheal resection (20). Its incidence ranges from 4% to 14% with a mortality of 7.8%, in large series (21).
In a series described by Gaissert et al. of 69 patients with thyroid carcinoma invading the trachea, the anastomotic dehiscence occurred in three cases (4%) with overall morbidity and mortality respectively of 36.2% and 1.2% (15). Lin et al. reported two anastomotic dehiscence over 19 patients (11%) explaining this complication as result of a not tension-free anastomosis (16). Furthermore, Piazza et al., in their series of 27 patients, detected an anastomotic dehiscence in 11% of cases (14).
One of the most important risk factor of anastomotic dehiscence is the length of the resected tracheal segment that is directly correlated with the tension over the suture line. Tracheal resections longer than 4 cm are associated with a remarkable rise of anastomotic dehiscence rate. Thus, in these cases, it is important to dissect the suprahyoid muscles from the hyoid bone to release the larynx in order to perform an end-to-end tension-free anastomosis (14). Furthermore, to accomplish a low anastomotic tension, it is useful to keep the neck flexed in a “chin to chest” position by two stiches placed in the submental crease and through the upper thoracic skin during the postoperative period. The “chin to chest” position is routinely used by thoracic surgeons and it is kept till the 6th or 7th postoperative day (10,11,17,22). However, some authors suggest using this approach only in case of tracheal resection longer than 4 cm and in re-resections (23).
An additional relevant preventive factor of anastomotic dehiscence is the preservation of the tracheal blood supply, which originates from the inferior thyroid artery and passes laterally along the tracheal wall. Thus, the tracheal dissection should take place along the anterior wall and it should be limited only to the resected segment. Particularly, Piazza et al. suggest dissecting no more than 1 cm from the residual stumps to be anatomized (14). Some surgeons cover anastomotic line with musculocutaneous flap to preserve and protect tracheal anastomosis (24).
Finally, an important aspect to consider is the management of the oro-tracheal tube during the postoperative period. There is no unanimous consensus about the timing of patients’ extubation. Patients are generally extubated immediately after surgery or 4 days later, according to the experience of each center. Nevertheless, an early oro-tracheal tube removal is suggested to limit the effects of positive ventilation on tracheal suture line (18,24).
Airway stenosis
Airway stenosis is an uncommon postoperative complication of tracheal sleeve resection and reconstruction. It can be the result of bilateral recurrent laryngeal nerve paralysis, fibrotic retraction or granuloma at the anastomotic site and laryngeal edema.
The bilateral vocal cord palsy due to recurrent laryngeal nerve injury occurs about in 10% of cases and it can be managed performing a partial CO2 laser cordectomy or a tracheostomy (10,15,16). Although the tracheostomy allows an immediate and effectiveness management of bilateral vocal cord paralysis, it is not accepted by patients as a long-term solution also when associated with the use of T-tube (10,11). A subsequent partial cordectomy is recommended when possible since it allows to create a considerable breathing space (10,11).
The introduction of new technologies, such as the intermittent or continuous intraoperative nerve monitoring (IIONM or CIONM, respectively), allows an easier identification of the recurrent laryngeal nerves, mainly in complex cases, reducing the risk of their injury (25).
Anastomotic site complications, as stenosis due to fibrotic retraction or to granuloma, are reported as late on-set complications. They are generally related to the development of dyspnea and emoftoe and are successfully treated by endoscopic dilation or laser resection. Piazza and coworkers reported an incidence of 6% of tracheal stenosis due to fibrotic retraction or granuloma at the suture line and the most of them (60%) were successfully managed only by transoral laser surgery (14).
Infection and bleeding
Local infections such as abscesses are rare and are generally related to anastomotic leaks. In a series of 40 cases by Nakao et al., the authors reported four cases (10%) of anastomotic leakage with subsequently development of neck infection and mediastinitis (10).
To prevent local infections some surgeons suggest administrating antibiotic therapy for 2 weeks after surgery (14). In our experience, we limited the antibiotic administration to the one-short preoperative dose without detecting any postoperative local infection (24). Another way to limit the risk of local infection is avoiding preoperative tracheostomy that should be consider only in selected patients, when it is not possible to obtain an optimal airway control (18,26).
Postoperative bleeding when not related to an inaccurate intraoperative hemostasis could be the results of a local infection including abscess which leads to major vascular (common carotid artery and the brachiocephalic artery) injury by the erosion of their wall. This can generally occur when the vessels adventitia has been removed during surgical procedures.
Local recurrence
Although local tumor recurrence is not an early postoperative complication, we consider useful to discuss this issue since it is an important data to consider during patients’ counseling about management, treatment and prognosis.
The thyroid cancer infiltrating the trachea recurs in 8% to 60% of cases after a median of 47.6 months (27). Different factors are reported as related to loco-regional recurrence as the thyroid tumor histopathological pattern and the type of surgery. Particularly a poor differentiated histology and the tracheal shaving technique are associated to a higher rate of tumor recurrence and a worse survival (14,28,29). Focusing on the shaving excision technique (tumor dissection from tracheal wall without tracheal resection), its relationship with a higher risk of tumor recurrence is still controversial and is related to the lack of clear surgical margin (15). Thus, it is still recommended the intraoperative frozen-section examination of surgical margins to verify the presence of tumor infiltration and to achieve a microscopic tumor-free resection.
Kim et al., in their series of 39 patients identified as possible risk factors of local recurrence at univariate analysis the presence of lateral cervical lymph node metastasis, the history of previous thyroid cancer surgery and the esophageal invasion. However, none of those factors were confirmed to be associated to local recurrence at the multivariate analysis (27).
In an interesting paper by Nishida and coworkers, the authors evaluated and compared postoperative tumor local recurrence rate and prognosis of patients with tracheal deep invasion from thyroid cancer undergoing thyroidectomy and additional tracheal resection to those undergoing tumor excisions without airway resection (due to lack of consent to the procedure). The local recurrence was 8% after a follow-up of 6.1 years in the first group and 79% after a follow-up of 1.2 years in the second one. Although this is not a randomized controlled study, mortality rate among two groups (tracheal resection vs. no tracheal resection) were 52% vs. 86%, respectively during the follow-up period (2).
Discussion
Tracheal resection with end-to-end anastomosis is the treatment of choice of thyroid cancer infiltrating the tracheal wall since it allows to obtain the loco-regional disease control and to improve survival and quality of life. Five-year survival rate was reported to be 78% and 88% respectively in Ishihara and Tsai series (11,30). In our previous series of seven patients [all stage IV by Shin (31)] the survival ranged from 18 to 108 months (24).
No large series are reported in the literature about this disease and limited data are available about factors associated to postoperative complications and their management. Comorbidity (as diabetes and previous corticosteroid treatment), Shin’s stage disease, length of tracheal resection, extent and aggressiveness of surgical resection (as laringo-tracheal and major vessels resection) are known to be related to anastomotic complications (31). This explains the importance of preoperative patient selection, the respect of the rules to obtain a tension free anastomosis and to reduce the risk of recurrent laryngeal nerve injury, infections and bleeding. Furthermore, the risk of postoperative morbidity can be reduced performing this surgical procedure in high volume centers where the postoperative mortality ranges from 0 to 3% (15,19,30,32).
Conclusions
In locally invasive thyroid cancer, en-bloc resection of the thyroid within the tracheal segment interested by the tumor is suggested by the American Thyroid Association Guidelines since it provides a good prognosis and a significant palliation reducing the risk of asphyxiation or hemoptysis (33). However, the postoperative complication rate related to this operation is non-negligible. Since less aggressive surgical procedures, as the tracheal shaving technique, do not guarantee an oncological loco-regional control of the disease, our suggestion is to perform a regular tracheal resection with end-to-end anastomosis after a careful preoperative patients’ selection and a meticulous respect of tension-free anastomosis principles to reduce the risk of postoperative complications.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Brauckhoff M, Machens A, Thanh PN, et al. Impact of extent of resection for thyroid cancer invading the aerodigestive tract on surgical morbidity, local recurrence, and cancer-specific survival. Surgery 2010;148:1257-66. [Crossref] [PubMed]
- Nishida T, Nakao K, Hamaji M, et al. Differentiated thyroid carcinoma with airway invasion: indication for tracheal resection based on the extent of cancer invasion. J Thorac Cardiovasc Surg 1997;114:84-92. [Crossref] [PubMed]
- Honings J, Stephen AE, Marres HA, et al. The management of thyroid carcinoma invading the larynx or trachea. Laryngoscope 2010;120:682-9. [Crossref] [PubMed]
- Shindo ML, Caruana SM, Kandil E, et al. Management of invasive well-differentiated thyroid cancer: an american head and neck society consensus statement. AHNS Consensus statement. Head Neck 2014;36:1379-90. [PubMed]
- Machens A, Hinze R, Dralle H. Surgery on the cervicovisceral axis for invasive thyroid cancer. Langenbecks Arch Surg 2001;386:318-23. [Crossref] [PubMed]
- Gillenwater AM, Goepfert H. Surgical management of laryngotracheal and esophageal involvement by locally advanced thyroid cancer. Semin Surg Oncol 1999;16:19-29. [Crossref] [PubMed]
- Grillo HC, Suen HC, Mathisen DJ, et al. Resectional management of thyroid carcinoma invading the airway. Ann Thorac Surg 1992;54:3-9. [Crossref] [PubMed]
- Bayles SW, Kingdom TT, Carlson GW. Management of thyroid carcinoma invading the aerodigestive tract. Laryngoscope 1998;108:1402-7. [Crossref] [PubMed]
- Wada N, Nakayama H, Masudo Y, et al. Clinical outcome of different modes of resection in papillary thyroid carcinomas with laryngotracheal invasion. Langenbecks Arch Surg 2006;391:545-9. [Crossref] [PubMed]
- Nakao K, Kurozumi K, Nakahara M, et al. Resection and reconstruction of the airway in patients with advanced thyroid cancer. World J Surg 2004;28:1204-6. [Crossref] [PubMed]
- Tsai YF, Tseng YL, Wu MH, et al. Aggressive resection of the airway invaded by thyroid carcinoma. Br J Surg 2005;92:1382-7. [Crossref] [PubMed]
- Yang CC, Lee CH, Wang LS, et al. Resectional treatment for thyroid cancer with tracheal invasion: a long-term follow-up study. Arch Surg 2000;135:704-7. [Crossref] [PubMed]
- Brauckhoff M, Meinicke A, Bilkenroth U, et al. Long-term results and functional outcome after cervical evisceration in patients with thyroid cancer. Surgery 2006;140:953-9. [Crossref] [PubMed]
- Piazza C, Del Bon F, Barbieri D, et al. Tracheal and Crico-Tracheal Resection and Anastomosis for Malignancies Involving the Thyroid Gland and the Airway. Ann Otol Rhinol Laryngol 2016;125:97-104. [Crossref] [PubMed]
- Gaissert HA, Honings J, Grillo HC, et al. Segmental laryngotracheal and tracheal resection for invasive thyroid carcinoma. Ann Thorac Surg 2007;83:1952-9. [Crossref] [PubMed]
- Lin S, Huang H, Liu X, et al. Treatments for complications of tracheal sleeve resection for papillary thyroid carcinoma with tracheal invasion. Eur J Surg Oncol 2014;40:176-81. [Crossref] [PubMed]
- Mossetti C, Palestini N, Bruna MC, et al. Segmental tracheal resection for invasive differentiated thyroid carcinoma. Our experience in eight cases. Langenbecks Arch Surg 2013;398:1075-82. [Crossref] [PubMed]
- Shenoy AM, Burrah R, Rao V, et al. Tracheal resection for thyroid cancer. J Laryngol Otol 2012;126:594-7. [Crossref] [PubMed]
- Ozaki O, Sugino K, Mimura T, et al. Surgery for patients with thyroid carcinoma invading the trachea: Circumferential sleeve resection followed by end-to-end anastomosis. Surgery 1995;117:268-71. [Crossref] [PubMed]
- Wright CD, Grillo HC, Wain JC, et al. Anastomotic complications after tracheal resection: prognostic factors and management. J Thorac Cardiovasc Surg 2004;128:731-9. [Crossref] [PubMed]
- Gerwat J, Bryce DP. The management of subglottic laryngeal stenosis by resection and direct anastomosis. Laryngoscope 1974;84:940-57. [Crossref] [PubMed]
- Grillo HC. Tracheal reconstruction: anterior approach and extended resection. In: Grillo HC. editor. Surgery of the Trachea and Bronchi. Hamilton: BC Decker Inc., 2004:539.
- Mutrie CJ, Eldaif SM, Rutledge CW, et al. Cervical tracheal resection: new lessons learned. Ann Thorac Surg 2011;91:1101-6. [Crossref] [PubMed]
- Pappalardo V, La Rosa S, Imperatori A, et al. Thyroid cancer with tracheal invasion: a pathological estimation. Gland Surg 2016;5:541-5. [Crossref] [PubMed]
- Schneider R, Randolph GW, Barczynski M, et al. Continuous intraoperative neural monitoring of the recurrent nerves in thyroid surgery: a quantum leap in technology. Gland Surg 2016;5:607-16. [Crossref] [PubMed]
- Price DL, Wong RJ, Randolph GW. Invasive thyroid cancer: management of the trachea and esophagus. Otolaryngol Clin North Am 2008;41:1155-68. ix-x. [Crossref] [PubMed]
- Kim H, Jung HJ, Lee SY, et al. Prognostic factors of locally invasive well-differentiated thyroid carcinoma involving the trachea. Eur Arch Otorhinolaryngol 2016;273:1919-26. [Crossref] [PubMed]
- Kasperbauer JL. Locally advanced thyroid carcinoma. Ann Otol Rhinol Laryngol 2004;113:749-53. [Crossref] [PubMed]
- Park CS, Suh KW, Min JS. Cartilage-shaving procedure for the control of tracheal cartilage invasion by thyroid carcinoma. Head Neck 1993;15:289-91. [Crossref] [PubMed]
- Ishihara T, Kobayashi K, Kikuchi K, et al. Surgical treatment of advanced thyroid carcinoma invading the trachea. J Thorac Cardiovasc Surg 1991;102:717-20. [PubMed]
- Shin DH, Mark EJ, Suen HC, et al. Pathologic staging of papillay carcinoma of the thyroid with airway invasion based on the anatomic manner of extension to the trachea: a clinicopathological study based on 22 patients who underwent thyroidectomy and airway resection. Hum Pathol 1993;24:866-70. [Crossref] [PubMed]
- Amorós JM, Ramos R, Villalonga R, et al. Tracheal and cricotracheal resection for laryngotracheal stenosis: axperience in 54 consecutive cases. Eur J Cardiothorac Surg 2006;29:35-9. [Crossref] [PubMed]
- Haugen BR, Sawka AM, Alexander EK, et al. American Thyroid Association Guidelines on the Management of Thyroid Nodules and Differentiated Thyroid Cancer Task Force Review and Recommendation on the Proposed Renaming of Encapsulated Follicular Variant Papillary Thyroid Carcinoma Without Invasion to Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features. Thyroid 2017;27:481-3. [Crossref] [PubMed]


