Morbidity from minimally invasive video-assisted thyroidectomy: a general review
Minimally invasive video-assisted thyroidectomy (MIVAT) was first described in 1998, and over the past two decades represents an evolution and a valid alternative to the conventional thyroidectomy technique (1,2). Its minimally invasive nature offers advantages over its conventional counterpart, by combining the benefits related to the endoscopic magnification with those due to its close similarity with traditional surgery. This completely gasless procedure is based on the same steps of the standard operation. The same intervention can be performed through a very minimal skin incision thanks to the use of the endoscope (2-5). The excellent visualization, due to the 2- to 3-fold endoscopic magnification, allows an easy and prompt identification of all anatomical structures. Ever since its introduction, MIVAT has been progressively evolving. Endoscopic thyroid surgery too requires an adequate knowledge of anatomy and a good experience in endocrine surgery. For a surgeon who approaches the MIVAT technique, the learning curve takes a longer time than with conventional surgery, having to gain confidence with a smaller surgical incision and with the use of endoscopic instruments (6).
In order to obtain the best results, surgeons who perform this intervention, or even interventions with a lower complication rate than the conventional technique, should be well trained (6).
In our experience, 10 patients represent the early stage of the learning process, 30 patients are the minimal number of cases in order to move on to a higher level, and performing at least 100 times the same procedure allows a reduction of the complication rate (7).
In fact, the operative time for MIVAT decreases gradually as the surgeon’s degree of experience increases (7). Since the time MIVAT was described, the technique has been adopted worldwide, and its indications expanded from the initial benign thyroid disease to low-risk and intermediate-risk carcinoma, demonstrating a level of oncologic radicality comparable to that of the conventional technique. For a long time, the indications for MIVAT remained almost unchanged; however, over the years it has been found that some changes could be made in order to broaden the range of patients eligible for this technique.
With respect to the main works available in the literature (8-10), the main changes concern the length of the surgical incision (increased to 3–3.5 cm); other works mention also the underlying disease, the size of the nodules, and the overall volume of the thyroid gland (10,11).
Furthermore, the minimally invasive nature of the technique has not compromised its ability to accomplish its purpose both safely and effectively.
In order to ensure the success of a minimally invasive video-assisted approach, an accurate selection of the patients is important; however even minimally invasive surgery is not free from complications, which are the same as those at risk with traditional surgery. Therefore, they include major complications, such as permanent recurrent laryngeal nerve (RLN) dysfunction and expanding hematoma, while minor complications include temporary RLN dysfunction, temporary hypocalcemia, temporary superior laryngeal nerve dysfunction, cellulitis, nonsurgical hematoma, seroma, postoperative pain and hypertrophic scar. Although thyroid surgery is associated with significant complications, according to many studies their frequency has gradually decreased over the past century. Duke et al. (12) suggest that MIVAT is associated with fewer overall complications than conventional thyroidectomy because MIVAT is not appropriate for all patients. Patients for MIVAT are carefully selected; they tend to be younger and generally have normal-sized glands with small nodules, and no thyroiditis nor invasive cancer.
In the meta-analysis by Pisanu et al. (13), nine randomized prospective studies were included in the quantitative analysis, comparing the MIVAT technique with conventional surgery (CT). The primary outcome measures that were evaluated comprised the overall morbidity prevalence, transient and permanent RLN paralysis, transient hypocalcemia, the presence of postoperative hematoma, and infection of the surgical wound. The study clearly showed that there were no statistically significant differences between the two techniques; however, this result may be considered in favor of MIVAT, because despite the small surgical incision, thanks to the endoscope it allows an effective visualization of all anatomical structures, faithfully replicating all the steps of conventional surgery (6,14-16).
One of the early results in favor of the MIVAT technique is the randomized prospective study we published in 2008 (7). Our data show a reduced incidence in early voice and swallowing post-surgical problems among patients who undergo MIVAT. The smaller surgical trauma allowed by MIVAT accounts for this more positive outcome.
Recently, Miccoli et al. (17) showed that the rate of complications involving the RLN is substantially similar to that already described in the literature; however, the study indicates that in tertiary referral centers, the incidence may prove slightly higher because of the large number of patients who undergo MIVAT, and of the frequently malignant nature of the underlying disease. Paradoxically, the use of advanced surgical instruments might further increase such rate, for instance due to heat transmission caused by the ultrasound scalpel that some surgeons use for coagulating and dividing vessels.
With regard to the incidence of hypoparathyroidism, causing hypocalcemia, the data found in the literature are discordant. However, Del Rio et al. (18) observed that the risk of postoperative hypocalcemia and the intraoperative identification of the parathyroid glands are more favourable than with conventional thyroidectomy, with a 7.58% rate of clinically symptomatic hypocalcemia.
The study by Neidich et al. (19) focuses on malignancy, finding remarkable differences between permanent and transient hypocalcemia and hypoparathyroidism. No case of permanent damage is reported, whereas the rate of transient complications recorded is, in fact, 10.7% for hypocalcemia and 25% for hypoparathyroidism. A further point of view can be found in the 2004 work by Micccoli et al. (20), which analyzed a cohort of 572 patients, recording a hypoparathyroidism rate of 0.2%, comparable to that of conventional surgery.
This is likely due to several factors. First, the enhanced visualization afforded by the endoscope aids in the early detection of the superior parathyroid glands. Second, the absence of thyroiditis in these patients may also contribute to the accurate detection of the parathyroid glands, and facilitate their dissection from the thyroid gland, without compromising their vascular supply. By means of two well-designed randomized trails (level II B), Gal et al. (14) and El Labban (21) reached the same conclusions. The studies show that the complication rate with the two approaches is similar, and that although conventional thyroidectomy involves a shorter operative time, the benefits of MIVAT are less scarring and more satisfactory cosmetic results, and reduced postoperative distress. Several comparative studies showed that MIVAT offers some significant advantages over conventional surgery, mainly in terms of improved cosmetic result and reduced post-operative pain, with no additional morbidity (6,22). A prospective randomized study by Miccoli et al. (23) confirmed the most favourable postoperative outcome of MIVAT through the dosage of different biochemical pain mediators, before and after surgery. The authors reported that VAS scores were significantly higher in the open group, whereas TGF-b and MCP-1 levels were found to be significantly lower in the open group than in the MIVAT group (23). Also, Zheng et al. (24) demonstrated that MIVAT entails a lower degree of immunosuppression, by minimizing the trauma (Table 1).
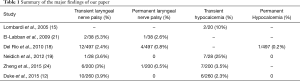
Full table
The literature seems consistent with a better postoperative outcome of MIVAT (17). In particular, during the whole postoperative period, it has been found that patients take less pain medications. For patients who undergo conventional surgery, the trauma, edema, the size of the surgical wound, represent some of the main causes of postoperative pain; this clearly represents an advantage of MIVAT (15,17). It is also obvious that from an aesthetic point of view, the patient prefers a smaller surgical incision (MIVAT 2–2.5 cm vs. CT 5–6 cm) (14) (Figure 1).
The less traumatic approach could also give reason for the reduced wound infection rate after MIVAT (6), and even the incidence of post-operative hematoma seems to be low. Actually, hematoma was never recorded in any of nine prospective randomized trials included in the meta-analysis by Pisanu (13). A precise selection of patients plays a significant role in ensuring the success of minimally invasive video-assisted approaches. At present, in selected cases and in experienced centers, MIVAT can be considered the standard treatment, having proven to be a feasible, practical, safe and effective surgical option. Its outcome equals that of conventional thyroidectomy, but with better cosmetic results.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Miccoli P, Pinchera A, Cecchini G, et al. Minimally invasive, video-assisted parathyroid surgery for primary hyperparathyroidism. J Endocrinol Invest 1997;20:429-30. [Crossref] [PubMed]
- Bellantone R, Lombardi CP, Raffaelli M, et al. Minimally invasive, totally gasless video-assisted thyroid lobectomy. Am J Surg 1999;177:342-43. [Crossref] [PubMed]
- Mourad M, Saab N, Malaise J, et al. Minimally invasive video-assisted approach for partial and total thyroidectomy: initial experience. Surg Endosc 2001;15:1108-11. [Crossref] [PubMed]
- Bellantone R, Lombardi CP, Raffaelli M, et al. Video-assisted thyroidectomy. J Am Coll Surg 2002;194:610-4. [Crossref] [PubMed]
- Miccoli P, Berti P, Raffaelli M, et al. Minimally invasive video-assisted thyroidectomy. Am J Surg 2001;181:567-70. [Crossref] [PubMed]
- Miccoli P, Berti P, Raffaelli M, et al. Comparison between minimally invasive video-assistedthyroidectomy and conventional thyroidectomy: a prospectiverandomised study. Surgery 2001;130:1039-43. [Crossref] [PubMed]
- Lombardi CP, Raffaelli M, D’Alatri L, et al. Video-assisted thyroidectomy significantly reduces the risk of early post-thyroidectomy voice and swallowing symptoms. World J Surg 2008;32:693-700. [Crossref] [PubMed]
- Terris DJ, Seybt MW. Modifications of Miccoli minimallyinvasive thyroidectomy for the low-volume surgeon. Am J Otolaryngo 2011;132:392-7. [Crossref]
- Fík Z, Astl J, Zábrodský M, et al. Minimally invasive video-assisted versus minimally invasive nonendoscopic thyroidectomy. Biomed Res Int 2014;2014:450170. [PubMed]
- Billmann F, Bokor-Bilmann T, Lapshyn H, et al. Minimal-access video-assisted thyroidectomyfor benign disease: a retrospective analysis of risk factors for postoperative complications. Int J Surg 2014;12:1306-9. [Crossref] [PubMed]
- Lai SY, Walvekar RR, Ferris RL. Minimally invasive video assisted thyroidectomy: expanded indications and oncologic completeness. Head Neck 2008;30:1403-7. [Crossref] [PubMed]
- Duke WS, White JR, Waller JL, et al. Six-Year Experience With Endoscopic Thyroidectomy: Outcomes and Safety Profile. Ann Otol Rhinol Laryngol 2015;124:915-20. [Crossref] [PubMed]
- Pisanu A, Podda M, Reccia I, et al. Systematic review with meta-analysis of prosèective randomized trials comparing minimally invasive video-assisted hyroidectomy (MIVAT) and convetional thyroidectomy (CT). Langenbecks Arch Surg 2013;398:1057-68. [Crossref] [PubMed]
- Gal I, Solymosi T, Szabo Z, et al. Minimally invasive video-assisted thyroidectomy and conventional thyroidectomy: a prospective randomized study. Surg Endosc 2008;22:2445-9. [Crossref] [PubMed]
- Lombardi CP, Raffaelli M, Princi P, et al. Safety of video-assisted thyroidectomy versus conventional surgery. Head Neck 2005;27:58-64. [Crossref] [PubMed]
- Chao TC, Lin JD, Chen MF. Video-assisted open thyroid lobectomy through a small incision. Surg Laparosc Endosc Percutan Tech 2004;14:15-9. [Crossref] [PubMed]
- Miccoli P, Materazzi G, Baggiani A, et al. Miniinvasive video-assisted surgery of the thyroid and parathyroid glands: a 2011 update. J Endocrinol Invest 2011;34:473-80. [Crossref] [PubMed]
- Del Rio P, Arcuri MF, Pisani P, et al. Minimally invasive video-assisted thyroidectomy (MIVAT): what is the real advantage? Langenbecks Arch Surg 2010;395:323-6. [Crossref] [PubMed]
- Neidich MJ, Steward DL. Safety and feasibility of elective minimally invasive video-assisted central neck dissection for thyroid carcinoma. Head Neck 2012;34:354-8. [Crossref] [PubMed]
- Miccoli P, Berti P, Materazzi G, et al. Minimally invasive video-assisted thyroidectomy: five years of experience. J Am Coll Surg 2004;199:243-8. [Crossref] [PubMed]
- El-Labban GM. Minimally invasive video-assisted thyroidectomy versus conventional thyroidectomy: A single-blinded, randomized controlled clinical trial. J Minim Access Surg 2009;5:97-102. [Crossref] [PubMed]
- Bellantone R, Lombardi CP, Bossola M, et al. Video-assisted vs conventional thyroid lobectomy - A randomized trial. Arch Surg 2002;137:301-4. [Crossref] [PubMed]
- Miccoli P, Rago R, Massi M, et al. Standard versus video-assisted thyroidectomy: objective postoperative pain evaluation. Surg Endosc 2010;24:2415-7. [Crossref] [PubMed]
- Zheng C, Liu S, Geng P, et al. Minimally invasive videoassisted versus conventional open thyroidectomy on immune response: a meta analysis. Int J Clin Exp Med 2015;8:2593-9. [PubMed]



