Patient determinants as independent risk factors for postoperative complications of breast reconstruction
Introduction
There is lack of large cohort analyses using patient determinants as risk factors for postoperative outcomes after breast reconstruction. Complications after breast reconstructive surgery are common (1-6), and it has been shown that complications affect patient emotional well-being, health-related quality of life and satisfaction (5,7-10). Patients’ satisfaction and health-related quality of life are frequently used as parameters for outcome measurement in plastic surgery.
Identifying independent risk factors for complications could have multiple advantages, such as making the treatment of patients with breast cancer requesting reconstruction more effective and aiding in selection of the best reconstruction method for each patient.
The effect of radiotherapy on breast reconstruction
Many studies on radiotherapy and complications after breast reconstruction have been performed. In the majority of studies, radiotherapy is shown to adversely affect outcome after implant-based breast reconstructions, with increased late failure rates (5,11,12), poor aesthetic results, loss of symmetry (13-15), capsular contracture, and infection, even when using the latest generation of implants (5,11,12,14,16-24).
Results from studies on radiotherapy and autologous reconstructions are more conflicting. Radiotherapy after mastectomy but before reconstruction has not been shown to increase complications after autologous reconstruction (25); however, not all studies are in agreement (26,27). Certain studies show that postoperative radiotherapy to the breast reconstructed with a deep inferior epigastric perforator flap (DIEP) or transverse rectus abdominis myocutaneous (TRAM) flap has no effect on the reconstruction (28,29), while several others show a considerable negative effect on the final results of autologous reconstruction (24,26,30-34).
The effect of chemotherapy and hormone therapy on breast reconstruction
Studies on the effect of adjuvant chemotherapy on postoperative complications are also not conclusive. Chemotherapy has been reported to be associated with a high rate of complications and reconstruction failure (18), but several other studies show no association between adjuvant chemotherapy and adverse events after breast reconstruction (12,35).
In the case of adjuvant hormone therapy, there is no agreement regarding its effect on complications. Some studies show an association with overall complications (36) and, especially, capsular contraction (16,37), while other studies have shown no such association (18,38-41).
The effect of patient characteristics on breast reconstruction
Several studies have examined the relationship between several patient characteristics (other than adjuvant therapy) and complications (2,6,42-45), but there was variation in the factors studied, and inconclusive results.
It is well established that high body mass index (BMI) increases the risk for surgical complications and overall morbidity in all types of breast reconstructions, both implant-based and autologous (46-54). It is also well established that smoking has a negative influence on free flap breast reconstruction (6,45,55-59), although some studies have failed to establish this relationship (4,60-62). The same seems to be true for implant-based reconstructions (16,35,44,63-65), but not all studies can confirm these findings (52). Many studies show no relationship between age and risk for complications (45,57,60-62,66-71), while other studies show that elderly patients have more risk (44,53,63). Diabetes has been associated with postoperative complications after autologous reconstruction, but the results after implant-based breast reconstruction are more conflicting (52,72-75). Patients with renal disease seem to be more prone to complications (75,76). Very little has been published on the history of DVT and postoperative complications, but one study showed an increased risk for thrombosis in free flap surgery in hypercoagulative patients and a very low salvage rate of the affected flaps (77). No reports seem to exist on the effect of concurrent rheumatic or neurologic disease and outcome after breast reconstruction.
The aim of the present study was to investigate the effect of numerous patient-related determinants (adjuvant therapy and concurrent diseases) on postoperative complication frequency among four different methods of breast reconstruction by systematically evaluating the outcome with identical criteria on a consecutive series of breast reconstruction cases.
Methods
The present study is a retrospective analysis of 623 consecutive patients who underwent surgery between 2003 and 2009 with one of four delayed breast reconstruction methods at the Department of Plastic Surgery, Sahlgrenska University Hospital, Gothenburg, Sweden.
The patients were enrolled from the operation database of the clinic (Operätt, C&S Healthcare Software AB, Mölndal, Sweden). The inclusion criteria were as follows: first time delayed reconstruction with (I) DIEP (78); (II) latissimus dorsi flap with silicone implant (LD) (79); (III) lateral thoracodorsal flap (LTDF) with silicone implant (80); or (IV) tissue expander with a secondary silicone implant (EXP) (81). The primary (expander) and secondary (implant) procedures were registered separately, as well as compiled, in the EXP group.
Existing data on at least 30 days of follow-up was required for inclusion; patients lost to follow-up were not included. Data were collected from the chart filing systems (Melior, Siemens Health Care, Upplands Väsby, Sweden, and Operätt) from the patients’ first referral to the last follow-up visit.
Demographic data
Demographic parameters registered were age, BMI, smoking status, previous radio- or chemotherapy, medications (hormone therapy, acetylsalicylic acid, corticosteroids, thyroid supplements, and anticoagulants), concurrent morbidity (diabetes, hypothyroidism, cardiovascular disease, history of thromboembolism, coagulopathy, and rheumatic, neurological, kidney, liver, or lung disease) as well as follow-up-time. Patient demography, perioperative parameters, and frequency of postoperative complications with respect to the different reconstructive methods for this group has previously been published (82).
Registered postoperative complications
Follow-up parameters and complications encountered were divided into early (≤30 days after surgery) and late (>30 days after surgery). The registered complications can be seen in Table 1. Detailed definitions of the registered complications have been previously published (82). The data was processed in a secure FileMaker database (Filemaker Inc., Santa Clara, CA, USA).
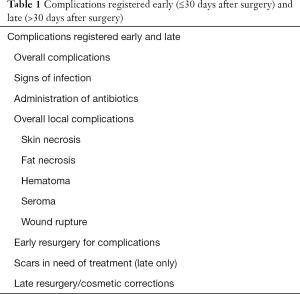
Full table
Statistics
Univariate and multivariate logistic regression was used to analyze the association between the independent (possible risk factors) and the dependent outcome parameters (postoperative complications). As the reconstruction methods varied significantly regarding the duration of surgery, blood loss during surgery, and the incidence of postoperative complications, all models were adjusted to the reconstructive method. Therefore, the reconstructive method itself was not a factor biasing the results of the statistical analysis. To analyze whether patient-related factors had an independent effect on the outcome variables, a multivariate logistic regression with adjustment for patient demographic parameters acting as confounding factors was performed. Thus, all demographic factors that acted as confounding factors were statistically adjusted for and did not bias the results of the statistical analysis. Relationships between independent (possible risk factors) and dependent (outcome) variables are presented with odds ratio (OR), 95% confidence interval (CI), and P value (P). All significance tests were two-sided and conducted at the 5% significance level. P values below 0.05 were considered statistically significant. Statistical analysis was performed with SPSS 23 (IBM Corp., Armonk, NY, USA). The study was approved by the Gothenburg Ethical Committee (No. 043-08).
Results
The median of follow-up time was 26.1 (Q1–Q3 15.1–41.8) months.
Early complications
Table 2 displays the associations between the patient-related factors and early complications. In the multivariate model, the patient factor related to the highest number of the early complications subgroups was smoking, and was associated with early overall complications, early administration of antibiotics, early overall local complications, and early skin necrosis. Increased BMI was ranked second, and was associated with early overall complications, early administration of antibiotics, and early resurgery. History of radiotherapy ranked third, and was associated with early administration of antibiotics, and early overall local complications. Age seemed to be a protective factor regarding development of early seroma.
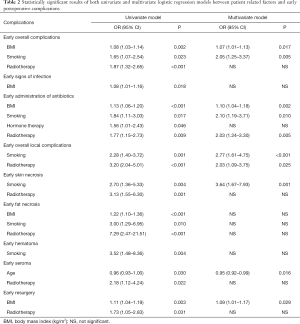
Full table
Independent risk factors combined
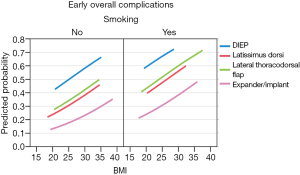
The patient-related factors of BMI and smoking were independent risk factors for overall early complications: BMI (OR 1.07, 95% CI 1.01–1.13, P=0.017) and smoking (OR 2.05, 95% CI 1.25–3.37, P=0.005). Thus, the risk for encountering overall early complications rose by 7% for each unit of BMI increase, and the risk increased over 200% if the patient was a smoker. When both risk factors were combined, the mean predicted probability was 230% higher for smokers with a BMI of 30 compared to non-smokers with a BMI of 20. The patients in the expander group had the greatest increase at 3.8-fold for the combination of high BMI and being a smoker (Figure 1).
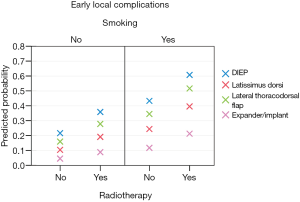
The patient related factors of smoking (OR 2.77, 95% CI 1.61–4.75, P<0.0001) and radiotherapy (OR 2.03, 95% CI 1.09–3.75, P=0.025) were independent risk factors for early local complications. Therefore, the risk for encountering early local complications rose by 277% if the patient was a smoker, and the risk increased over 200% if the patient was irradiated. The predicted probability for all methods increased a mean 3.6-fold for smokers who had undergone radiotherapy compared to patients who were neither smokers and had not undergone radiotherapy. The patients in the expander group had the greatest increase of 4.6-fold for the combination of smoking and radiotherapy (Figure 2).
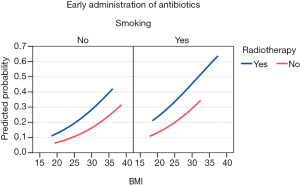
When BMI was added as a third risk factor, the association to early administration of antibiotics was multiplied. BMI (OR 1.10, 95% CI 1.04–1.18, P=0.002), smoking (OR 2.10, 95% CI 1.19–3.71, P=0.010) and radiotherapy (OR 2.03, 95% CI 1.24–3.30, P=0.005) were independent risk factors for early administration of antibiotics. A smoking, irradiated patient with a BMI of 30 had a 7.2-fold risk for early administration of antibiotics than a non-smoking, non-irradiated patient with a BMI of 20 (Figure 3).
Hypothyroidism, cardiovascular disease, coagulopathy, liver disease, and lung disease had no statistically significant relationship to any of the complications registered.
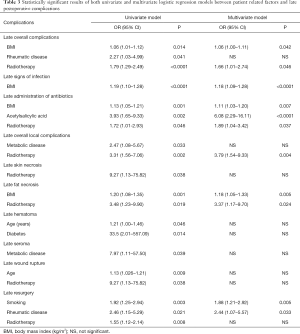
Late complications
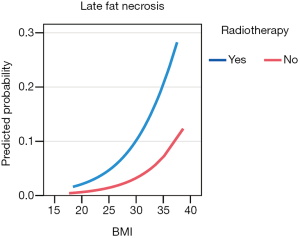
Table 3 displays the associations between the patient-related factors and late complications. In the multivariate model, the patient factors related to the highest number of the subgroups of late complications were high BMI (late overall complications, late signs of infection, late administration of antibiotics, and late fat necrosis), and history of radiotherapy (late overall complications, late administration of antibiotics, late overall local complications, and late fat necrosis). Smoking had a relationship with late resurgery only. Taking acetylsalicylic acid had a relationship with late administration of antibiotics.
Full table
Independent risk factors combined
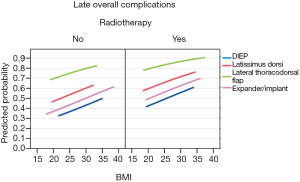
The patient related factors of BMI and history of radiotherapy were independent risk factors for late overall complications; BMI (OR 1.06, 95% CI 1.00–1.11, P=0.042) and radiotherapy (OR 1.66, 95% CI 1.01–2.74, P=0.046). Thus, the risk of encountering overall late complications rose by 6% for each unit of BMI increased, and the risk rose by 66% if the patient was irradiated. When both risk factors were combined, an irradiated patient with a BMI of 30 had a 2.3-fold higher risk for late overall complications than a non-irradiated patient with a BMI of 20 (Figure 4).
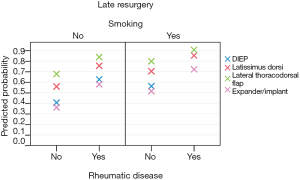
The patient related factors of smoking and rheumatic disease were independent risk factors for late resurgery—smoking (OR 1.88, 95% CI 1.21–2.92, P=0.005) and rheumatic disease (OR 2.44, 95% CI 1.07–5.57, P=0.033). Thus, the risk for encountering late resurgery was 88% higher if the patient was a smoker, and 244% higher if the patient had rheumatic disease. A smoking patient with history of rheumatic disease had over 3-fold higher risk for late resurgery compared to that in a non-smoking patient without rheumatic disease (Figure 5).
The patient related factors of BMI and radiotherapy were independent risk factors for late fat necrosis: BMI (OR 1.18, 95% CI 1.05–1.33, P=0.005) and radiotherapy (OR 3.37, 95% CI 1.17–9.70, P=0.024). Therefore, the risk of encountering late fat necrosis rose by 18% for each unit of BMI increase, and the risk increased by 337% if the patient was irradiated. An irradiated patient with a BMI of 30 had a 16.4-fold higher risk for late fat necrosis than a non-irradiated patient with BMI of 20 (Figure 6).
Discussion
In the present study, we found that smoking, increased BMI, and history of radiotherapy were closely associated with several postoperative complications, both early and late, irrespective of reconstruction method. Interestingly, smoking was associated with several early complications (early overall complications, early administration of antibiotics, early overall local complications, and early skin necrosis), but only one late complication (late resurgery). Increased BMI affects both early complications (early overall complications, early administration of antibiotics, and early resurgery) and late complications (late overall complications, late signs of infection, late administration of antibiotics, and late fat necrosis). History of radiotherapy, on the other hand, generally affects late complications (late overall complications, late administration of antibiotics, late overall local complications, and late fat necrosis), but also has some effect on early complications (early administration of antibiotics and early overall local complications). Additionally, when the different independent risk factors are combined, the risks increased considerably.
Significant independent risk factors have been previously identified, both in plastic surgery and in other specialities (40,44,45,50,72,83-93). However, the advantage of the present study is the evaluation of four different reconstruction methods with the same criteria for complications. This is the first study on a large group of patients where the association between an extensive panorama of patient-related factors and meticulously registered postoperative complications was studied using the same stringent definition of complications applied to all reconstruction methods, and showing that the risk increases were independent of surgical method. The large number of patients also allows adjustment for all confounding factors, providing independent risk factors and the construction of risk models (Figures 1-6).
In this study, the negative findings are almost equally interesting. Hormone and chemotherapy did not appear to affect complication rates after breast reconstruction, which is in agreement with most other studies (1,12,35), but conflicts with one (18). Additionally, age does not appear to have an association with postoperative complications except for a protective effect on early seroma. History of chemotherapy, adjuvant hormone therapy, and concurrent morbidity (diabetes, hypothyroidism, cardiovascular disease, history of thromboembolism, coagulopathy, and rheumatic, neurological, kidney, liver, or lung disease) had no association with any of the registered complications.
The obviously increased risk associated with smoking and high BMI actualizes the question on whether healthcare providers should demand that patients cease smoking and reduce to normal BMI before surgery.
Radiotherapy is still one of the most beneficial treatments to increase survival in many types of breast cancer (94,95). Radiotherapy inevitably damages the tissue, and, as long as the modus of radiotherapy is unchanged, post-radiation breast reconstruction will be more challenging. Most studies find that radiotherapy in an implant-based reconstruction increases complications and late failure rates (5,11-23). The results of the present study are in line with those of other studies in this field (5,11-23,30,31,33).
Radiotherapy after mastectomy but before reconstruction has not been shown to increase complications of the flaps after autologous reconstruction (25), although not all studies agree on this (26,27). However, autologous breast reconstruction provides reduced morbidity than implant-based reconstruction in the setting of postoperative radiotherapy (2,26). In the present study, no patients received radiotherapy after the breast reconstruction, only before.
The association between radiotherapy and implant-based reconstruction has been addressed in many studies using various methodologies. However, in the present study, all complications were meticulously registered, and the same complication definitions were used for all four methods. The study group was large, which enabled the construction of a strong statistical model, allowing for adjustment for all factors acting as confounding factors. Consequently, the statistically significant associations are true associations, and unbiased by the surgical method or patient determinants acting as confounding factors in the model.
The aim for a successful breast reconstruction is to ensure the patient is satisfied with a breast that is almost never the same quality or has the same sensation compared to that before the mastectomy. One of the key elements to patient satisfaction is safety during the procedure. It is well established that postoperative complications influence patient satisfaction (5,7,8). Therefore it is essential to minimize risks during the surgery. The present study contains an important piece of information to assist in optimal patient assessment before breast reconstruction and provides evidence for the goal of making an individual assessment of each patient to minimize the risks of the surgical procedure, and thereby maximal gain in health-related quality of life after breast reconstruction.
Conclusions
The present study firmly supports that, among a group of patients undergoing four different breast reconstruction methods, there is good evidence that patients should cease smoking and overweight patients should lose weight before surgery. Additionally, if the patient has had radiotherapy, the reconstruction method should be carefully chosen. This could reduce the likelihood of negative outcomes, reduce costs, and provide better cosmetic results and postoperative quality of life.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Gothenburg Ethical Committee (No. 043-08).
References
- Alderman AK, Wilkins EG, Kim HM, et al. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg 2002;109:2265-74. [Crossref] [PubMed]
- Chawla AK, Kachnic LA, Taghian AG, et al. Radiotherapy and breast reconstruction: complications and cosmesis with TRAM versus tissue expander/implant. Int J Radiat Oncol Biol Phys 2002;54:520-6. [Crossref] [PubMed]
- Cordeiro PG, McCarthy CM. A single surgeon's 12-year experience with tissue expander/implant breast reconstruction: part I. A prospective analysis of early complications. Plast Reconstr Surg 2006;118:825-31. [Crossref] [PubMed]
- Hofer SO, Damen TH, Mureau MA, et al. A critical review of perioperative complications in 175 free deep inferior epigastric perforator flap breast reconstructions. Ann Plast Surg 2007;59:137-42. [Crossref] [PubMed]
- Krueger EA, Wilkins EG, Strawderman M, et al. Complications and patient satisfaction following expander/implant breast reconstruction with and without radiotherapy. Int J Radiat Oncol Biol Phys 2001;49:713-21. [Crossref] [PubMed]
- Selber JC, Kurichi JE, Vega SJ, et al. Risk factors and complications in free TRAM flap breast reconstruction. Ann Plast Surg 2006;56:492-7. [Crossref] [PubMed]
- Andrade WN, Baxter N, Semple JL. Clinical determinants of patient satisfaction with breast reconstruction. Plast Reconstr Surg 2001;107:46-54. [Crossref] [PubMed]
- Gopie JP, Timman R, Hilhorst MT, et al. The short-term psychological impact of complications after breast reconstruction. Psychooncology 2013;22:290-8. [PubMed]
- Nicholson RM, Leinster S, Sassoon EM. A comparison of the cosmetic and psychological outcome of breast reconstruction, breast conserving surgery and mastectomy without reconstruction. Breast 2007;16:396-410. [Crossref] [PubMed]
- Isern AE, Tengrup I, Loman N, et al. Aesthetic outcome, patient satisfaction, and health-related quality of life in women at high risk undergoing prophylactic mastectomy and immediate breast reconstruction. J Plast Reconstr Aesthet Surg 2008;61:1177-87. [Crossref] [PubMed]
- Barreau-Pouhaer L, Lê MG, Rietjens M, et al. Risk factors for failure of immediate breast reconstruction with prosthesis after total mastectomy for breast cancer. Cancer 1992;70:1145-51. [Crossref] [PubMed]
- Nahabedian MY, Tsangaris T, Momen B, et al. Infectious complications following breast reconstruction with expanders and implants. Plast Reconstr Surg 2003;112:467-76. [Crossref] [PubMed]
- Vandeweyer E, Deraemaecker R. Radiation therapy after immediate breast reconstruction with implants. Plast Reconstr Surg 2000;106:56-8; discussion 59-60. [Crossref] [PubMed]
- Evans GR, Schusterman MA, Kroll SS, et al. Reconstruction and the radiated breast: is there a role for implants? Plast Reconstr Surg 1995;96:1111-5; discussion,1116-8. [Crossref] [PubMed]
- Gerber B, Krause A, Dieterich M, et al. The oncological safety of skin sparing mastectomy with conservation of the nipple-areola complex and autologous reconstruction: an extended follow-up study. Ann Surg 2009;249:461-8. [Crossref] [PubMed]
- Cowen D, Gross E, Rouannet P, et al. Immediate post-mastectomy breast reconstruction followed by radiotherapy: risk factors for complications. Breast Cancer Res Treat 2010;121:627-34. [Crossref] [PubMed]
- McCarthy CM, Pusic AL, Disa JJ, et al. Unilateral postoperative chest wall radiotherapy in bilateral tissue expander/implant reconstruction patients: a prospective outcomes analysis. Plast Reconstr Surg 2005;116:1642-7. [Crossref] [PubMed]
- Tallet AV, Salem N, Moutardier V, et al. Radiotherapy and immediate two-stage breast reconstruction with a tissue expander and implant: complications and esthetic results. Int J Radiat Oncol Biol Phys 2003;57:136-42. [Crossref] [PubMed]
- Clough KB, O'Donoghue JM, Fitoussi AD, et al. Prospective evaluation of late cosmetic results following breast reconstruction: I. Implant reconstruction. Plast Reconstr Surg 2001;107:1702-9. [Crossref] [PubMed]
- Kronowitz SJ, Robb GL. Breast reconstruction with postmastectomy radiation therapy: current issues. Plast Reconstr Surg 2004;114:950-60. [Crossref] [PubMed]
- Ringberg A, Tengrup I, Aspegren K, et al. Immediate breast reconstruction after mastectomy for cancer. Eur J Surg Oncol 1999;25:470-6. [Crossref] [PubMed]
- Vandeweyer E, Hertens D, Nogaret JM, et al. Immediate breast reconstruction with saline-filled implants: no interference with the oncologic outcome? Plast Reconstr Surg 2001;107:1409-12. [Crossref] [PubMed]
- Spear SL, Onyewu C. Staged breast reconstruction with saline-filled implants in the irradiated breast: recent trends and therapeutic implications. Plast Reconstr Surg 2000;105:930-42. [Crossref] [PubMed]
- Kronowitz SJ, Robb GL. Radiation therapy and breast reconstruction: a critical review of the literature. Plast Reconstr Surg 2009;124:395-408. [Crossref] [PubMed]
- Williams JK, Bostwick J 3rd, Bried JT, et al. TRAM flap breast reconstruction after radiation treatment. Ann Surg 1995;221:756-64; discussion 764-6. [Crossref] [PubMed]
- Barry M, Kell MR. Radiotherapy and breast reconstruction: a meta-analysis. Breast Cancer Res Treat 2011;127:15-22. [Crossref] [PubMed]
- Javaid M, Song F, Leinster S, et al. Radiation effects on the cosmetic outcomes of immediate and delayed autologous breast reconstruction: an argument about timing. J Plast Reconstr Aesthet Surg 2006;59:16-26. [Crossref] [PubMed]
- Chatterjee JS, Lee A, Anderson W, et al. Effect of postoperative radiotherapy on autologous deep inferior epigastric perforator flap volume after immediate breast reconstruction. Br J Surg 2009;96:1135-40. [Crossref] [PubMed]
- Schaverien MV, Macmillan RD, McCulley SJ. Is immediate autologous breast reconstruction with postoperative radiotherapy good practice?: a systematic review of the literature. J Plast Reconstr Aesthet Surg 2013;66:1637-51. [Crossref] [PubMed]
- Tran NV, Evans GR, Kroll SS, et al. Postoperative adjuvant irradiation: effects on tranverse rectus abdominis muscle flap breast reconstruction. Plast Reconstr Surg 2000;106:313-7; discussion 318-20. [Crossref] [PubMed]
- Tran NV, Chang DW, Gupta A, et al. Comparison of immediate and delayed free TRAM flap breast reconstruction in patients receiving postmastectomy radiation therapy. Plast Reconstr Surg 2001;108:78-82. [Crossref] [PubMed]
- Shaikh-Naidu N, Preminger BA, Rogers K, et al. Determinants of aesthetic satisfaction following TRAM and implant breast reconstruction. Ann Plast Surg 2004;52:465-70; discussion 470. [Crossref] [PubMed]
- Rogers NE, Allen RJ. Radiation effects on breast reconstruction with the deep inferior epigastric perforator flap. Plast Reconstr Surg 2002;109:1919-24;discussion 1925-6.
- Spear SL, Ducic I, Low M, et al. The effect of radiation on pedicled TRAM flap breast reconstruction: outcomes and implications. Plast Reconstr Surg 2005;115:84-95. [PubMed]
- McCarthy CM, Mehrara BJ, Riedel E, et al. Predicting complications following expander/implant breast reconstruction: an outcomes analysis based on preoperative clinical risk. Plast Reconstr Surg 2008;121:1886-92. [Crossref] [PubMed]
- Alderman A, Gutowski K, Ahuja A, et al. ASPS clinical practice guideline summary on breast reconstruction with expanders and implants. Plast Reconstr Surg 2014;134:648e-55e. [Crossref] [PubMed]
- Carnevale A, Scaringi C, Scalabrino G, et al. Radiation therapy after breast reconstruction: outcomes, complications, and patient satisfaction. Radiol Med 2013;118:1240-50. [Crossref] [PubMed]
- Whitfield GA, Horan G, Irwin MS, et al. Incidence of severe capsular contracture following implant-based immediate breast reconstruction with or without postoperative chest wall radiotherapy using 40 Gray in 15 fractions. Radiother Oncol 2009;90:141-7. [Crossref] [PubMed]
- Baschnagel AM, Shah C, Wilkinson JB, et al. Failure rate and cosmesis of immediate tissue expander/implant breast reconstruction after postmastectomy irradiation. Clin Breast Cancer 2012;12:428-32. [Crossref] [PubMed]
- Kim SH, Kim JM, Park SH, et al. Analysis of the effects of breast reconstruction in breast cancer patients receiving radiotherapy after mastectomy. Arch Plast Surg 2012;39:222-6. [Crossref] [PubMed]
- Eberlein TJ, Crespo LD, Smith BL, et al. Prospective evaluation of immediate reconstruction after mastectomy. Ann Surg 1993;218:29-36. [Crossref] [PubMed]
- Francis SH, Ruberg RL, Stevenson KB, et al. Independent risk factors for infection in tissue expander breast reconstruction. Plast Reconstr Surg 2009;124:1790-6. [Crossref] [PubMed]
- Miller RB, Reece G, Kroll SS, et al. Microvascular breast reconstruction in the diabetic patient. Plast Reconstr Surg 2007;119:38-45; discussion 46-8. [Crossref] [PubMed]
- Petersen A, Eftekhari AL, Damsgaard TE. Immediate breast reconstruction: a retrospective study with emphasis on complications and risk factors. J Plast Surg Hand Surg 2012;46:344-8. [Crossref] [PubMed]
- Seidenstuecker K, Munder B, Mahajan AL, et al. Morbidity of microsurgical breast reconstruction in patients with comorbid conditions. Plast Reconstr Surg 2011;127:1086-92. [Crossref] [PubMed]
- Hanwright PJ, Davila AA, Hirsch EM, et al. The differential effect of BMI on prosthetic versus autogenous breast reconstruction: a multivariate analysis of 12,986 patients. Breast 2013;22:938-45. [Crossref] [PubMed]
- Lin KY, Johns FR, Gibson J, et al. An outcome study of breast reconstruction: presurgical identification of risk factors for complications. Ann Surg Oncol 2001;8:586-91. [Crossref] [PubMed]
- Olsen MA, Lefta M, Dietz JR, et al. Risk factors for surgical site infection after major breast operation. J Am Coll Surg 2008;207:326-35. [Crossref] [PubMed]
- Munhoz AM, Aldrighi CM, Montag E, et al. Clinical outcomes following nipple-areola-sparing mastectomy with immediate implant-based breast reconstruction: a 12-year experience with an analysis of patient and breast-related factors for complications. Breast Cancer Res Treat 2013;140:545-55. [Crossref] [PubMed]
- Ogunleye AA, de Blacam C, Curtis MS, et al. An analysis of delayed breast reconstruction outcomes as recorded in the American College of Surgeons National Surgical Quality Improvement Program. J Plast Reconstr Aesthet Surg 2012;65:289-94. [Crossref] [PubMed]
- Davies K, Allan L, Roblin P, et al. Factors affecting post-operative complications following skin sparing mastectomy with immediate breast reconstruction. Breast 2011;20:21-5. [Crossref] [PubMed]
- Kato H, Nakagami G, Iwahira Y, et al. Risk factors and risk scoring tool for infection during tissue expansion in tissue expander and implant breast reconstruction. Breast J 2013;19:618-26. [Crossref] [PubMed]
- Fischer JP, Nelson JA, Serletti JM, et al. Peri-operative risk factors associated with early tissue expander (TE) loss following immediate breast reconstruction (IBR): a review of 9305 patients from the 2005-2010 ACS-NSQIP datasets. J Plast Reconstr Aesthet Surg 2013;66:1504-12. [Crossref] [PubMed]
- Momeni A, Ahdoot MA, Kim RY, et al. Should we continue to consider obesity a relative contraindication for autologous microsurgical breast reconstruction? J Plast Reconstr Aesthet Surg 2012;65:420-5. [Crossref] [PubMed]
- Booi DI, Debats IB, Boeckx WD, et al. Risk factors and blood flow in the free transverse rectus abdominis (TRAM) flap: smoking and high flap weight impair the free TRAM flap microcirculation. Ann Plast Surg 2007;59:364-71. [Crossref] [PubMed]
- Chang DW, Reece GP, Wang B, et al. Effect of smoking on complications in patients undergoing free TRAM flap breast reconstruction. Plast Reconstr Surg 2000;105:2374-80. [Crossref] [PubMed]
- Gill PS, Hunt JP, Guerra AB, et al. A 10-year retrospective review of 758 DIEP flaps for breast reconstruction. Plast Reconstr Surg 2004;113:1153-60. [Crossref] [PubMed]
- Padubidri AN, Yetman R, Browne E, et al. Complications of postmastectomy breast reconstructions in smokers, ex-smokers, and nonsmokers. Plast Reconstr Surg 2001;107:342-9; discussion 350-1. [Crossref] [PubMed]
- Vega S, Smartt JM Jr, Jiang S, et al. 500 Consecutive patients with free TRAM flap breast reconstruction: a single surgeon’s experience. Plast Reconstr Surg 2008;122:329-39. [Crossref] [PubMed]
- Nahabedian MY, Momen B, Galdino G, et al. Breast Reconstruction with the free TRAM or DIEP flap: patient selection, choice of flap, and outcome. Plast Reconstr Surg 2002;110:466-75; discussion 476-7. [Crossref] [PubMed]
- Nahabedian MY, Momen B, Manson PN. Factors associated with anastomotic failure after microvascular reconstruction of the breast. Plast Reconstr Surg 2004;114:74-82. [Crossref] [PubMed]
- Peeters WJ, Nanhekhan L, Van Ongeval C, et al. Fat necrosis in deep inferior epigastric perforator flaps: an ultrasound-based review of 202 cases. Plast Reconstr Surg 2009;124:1754-8. [Crossref] [PubMed]
- Fischer JP, Wes AM, Tuggle CT 3rd, et al. Risk analysis of early implant loss after immediate breast reconstruction: a review of 14,585 patients. J Am Coll Surg 2013;217:983-90. [Crossref] [PubMed]
- Christensen BO, Overgaard J, Kettner LO, et al. Long-term evaluation of postmastectomy breast reconstruction. Acta Oncol 2011;50:1053-61. [Crossref] [PubMed]
- Woerdeman LA, Hage JJ, Hofland MM, et al. A prospective assessment of surgical risk factors in 400 cases of skin-sparing mastectomy and immediate breast reconstruction with implants to establish selection criteria. Plast Reconstr Surg 2007;119:455-63. [Crossref] [PubMed]
- Guerra AB, Metzinger SE, Bidros RS, et al. Bilateral breast reconstruction with the deep inferior epigastric perforator (DIEP) flap: an experience with 280 flaps. Ann Plast Surg 2004;52:246-52. [Crossref] [PubMed]
- Lipa JE, Youssef AA, Kuerer HM, et al. Breast reconstruction in older women: advantages of autogenous tissue. Plast Reconstr Surg 2003;111:1110-21. [Crossref] [PubMed]
- Nahabedian MY. Breast reconstruction: a review and rationale for patient selection. Plast Reconstr Surg 2009;124:55-62. [Crossref] [PubMed]
- Tzafetta K, Ahmed O, Bahia H, et al. Evaluation of the factors related to postmastectomy breast reconstruction. Plast Reconstr Surg 2001;107:1694-701. [Crossref] [PubMed]
- Walton L, Ommen K, Audisio RA. Breast reconstruction in elderly women breast cancer: a review. Cancer Treat Rev 2011;37:353-7. [Crossref] [PubMed]
- Leyngold MM, Stutman RL, Khiabani KT, et al. Contributing variables to post mastectomy tissue expander infection. Breast J 2012;18:351-6. [Crossref] [PubMed]
- Wang XL, Liu LB, Song FM, et al. Meta-analysis of the safety and factors contributing to complications of MS-TRAM, DIEP, and SIEA flaps for breast reconstruction. Aesthetic Plast Surg 2014;38:681-91. [Crossref] [PubMed]
- Qin C, Vaca E, Lovecchio F, et al. Differential impact of non-insulin-dependent diabetes mellitus and insulin-dependent diabetes mellitus on breast reconstruction outcomes. Breast Cancer Res Treat 2014;146:429-38. [Crossref] [PubMed]
- Fischer JP, Tuggle CT, Au A, et al. A 30-day risk assessment of mastectomy alone compared to immediate breast reconstruction (IBR). J Plast Surg Hand Surg 2014;48:209-15. [Crossref] [PubMed]
- Jeong HS, Miller TJ, Davis K, et al. Application of the Caprini risk assessment model in evaluation of non-venous thromboembolism complications in plastic and reconstructive surgery patients. Aesthet Surg J 2014;34:87-95. [Crossref] [PubMed]
- Miller TJ, Jeong HS, Davis K, et al. Evaluation of the American Society of Anesthesiologists Physical Status classification system in risk assessment for plastic and reconstructive surgery patients. Aesthet Surg J 2014;34:448-56. [Crossref] [PubMed]
- Wang TY, Serletti JM, Cuker A, et al. Free tissue transfer in the hypercoagulable patient: a review of 58 flaps. Plast Reconstr Surg 2012;129:443-53. [Crossref] [PubMed]
- Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg 1994;32:32-8. [Crossref] [PubMed]
- Bostwick J 3rd, Scheflan M. The latissimus dorsi musculocutaneous flap: a one-stage breast reconstruction. Clin Plast Surg 1980;7:71-8. [PubMed]
- Holmström H, Lossing C. The lateral thoracodorsal flap in breast reconstruction. Plast Reconstr Surg 1986;77:933-43. [Crossref] [PubMed]
- Strock LL. Two-stage expander implant reconstruction: recent experience. Plast Reconstr Surg 2009;124:1429-36. [Crossref] [PubMed]
- Thorarinsson A, Fröjd V, Kölby L, et al. A retrospective review of the incidence of various complications in different delayed breast reconstruction methods. J Plast Surg Hand Surg 2016;50:25-34. [Crossref] [PubMed]
- Balentine CJ, Wilks J, Robinson C, et al. Obesity increases wound complications in rectal cancer surgery. J Surg Res 2010;163:35-9. [Crossref] [PubMed]
- Chan MM, Hamza N, Ammori BJ. Duration of surgery independently influences risk of venous thromboembolism after laparoscopic bariatric surgery. Surg Obes Relat Dis 2013;9:88-93. [Crossref] [PubMed]
- Eriksson M, Anveden L, Celebioglu F, et al. Radiotherapy in implant-based immediate breast reconstruction: risk factors, surgical outcomes, and patient-reported outcome measures in a large Swedish multicenter cohort. Breast Cancer Res Treat 2013;142:591-601. [Crossref] [PubMed]
- Fischer JP, Nelson JA, Au A, et al. Complications and morbidity following breast reconstruction--a review of 16,063 cases from the 2005-2010 NSQIP datasets. J Plast Surg Hand Surg 2014;48:104-14. [Crossref] [PubMed]
- Hanwright PJ, Davila AA, Mioton LM, et al. A predictive model of risk and outcomes in tissue expander reconstruction: a multivariate analysis of 9786 patients. J Plast Surg Hand Surg 2013;47:513-8. [PubMed]
- Hirsch EM, Seth AK, Kim JY, et al. Analysis of risk factors for complications in expander/implant breast reconstruction by stage of reconstruction. Plast Reconstr Surg 2014;134:692e-9e. [Crossref] [PubMed]
- Lundberg J, Thorarinsson A, Karlsson P, et al. When is the deep inferior epigastric artery flap indicated for breast reconstruction in patients not treated with radiotherapy? Ann Plast Surg 2014;73:105-13. [Crossref] [PubMed]
- Nguyen KT, Hanwright PJ, Smetona JT, et al. Body mass index as a continuous predictor of outcomes after expander-implant breast reconstruction. Ann Plast Surg 2014;73:19-24. [Crossref] [PubMed]
- Nugent EK, Hoff JT, Gao F, et al. Wound complications after gynecologic cancer surgery. Gynecol Oncol 2011;121:347-52. [Crossref] [PubMed]
- Schaverien MV, Mcculley SJ. Effect of obesity on outcomes of free autologous breast reconstruction: a meta-analysis. Microsurgery 2014;34:484-97. [Crossref] [PubMed]
- Tønnesen H, Nielsen PR, Lauritzen JB, et al. Smoking and alcohol intervention before surgery: evidence for best practice. Br J Anaesth 2009;102:297-306. [Crossref] [PubMed]
- Cotlar AM, Dubose JJ, Rose DM. History of surgery for breast cancer: radical to the sublime. Curr Surg 2003;60:329-37. [Crossref] [PubMed]
- Poortmans P. Evidence based radiation oncology: breast cancer. Radiother Oncol 2007;84:84-101. [Crossref] [PubMed]


