Preoperative management in patients with Graves’ disease
Graves’ disease is the most common cause of hyperthyroidism in iodine-sufficient geographical areas, with a prevalence rate in the USA of about 1.2% (0.5% overt and 0.7% subclinical) (1) and with an annual incidence of 20 to 50 cases per 100,000 persons (2).
More common in women, Graves’ disease is an autoimmune disorder that involves the whole thyroid gland and results from complex interactions between genetic and environmental factors (3). Thyroid-stimulating immunoglobulins of the IgG1 subclass stimulate thyroid follicular cells and cause the overproduction and release of thyroid hormones by activating the thyrotropin (TSH) receptor, thus abrogating the physiological regulatory role of the hypothalamic-pituitary axis. In addition, infiltrating immune cells, such as B and T cells and antigen-presenting-cells, produce a number of cytokines (interleukins 1β, 6, 12, 16, and 17, interferon-γ, tumor necrosis factor α, CD40 ligand, and others), which in turn activate and maintain inflammation and alter the behavior of thyroid epithelial cells (4).
The Merseburg triad, including palpitations (due to hyperthyroidism), goiter, and exophthalmos (Graves’ orbitopathy), characterizes the classical description of Graves’disease. However, clinical presentation is heterogeneous, depending on the age of the patient at the onset of dysfunction, as well as on the severity and duration of thyroid hormones excess. Symptoms and signs result from both hyperthyroidism and underlying autoimmunity (4). Typically reported symptoms are nervousness, anxiety, disturbed sleep, palpitations, heat intolerance, increased sweating, easy fatigue, and weight loss. Common physical findings include tachycardia, distal tremors, warm and sweaty skin, goiter, and thyroid bruit (5,6). When goiter is present, diffuse thyroid enlargement is most frequent, but many patients who live in iodine-deficient regions have coexisting nodular goiter. In newly diagnosed Graves’ patients, goiter is absent in almost 50% of patients (7). Extrathyroidal manifestations of Graves’ disease include: Graves’ orbitopathy, the main signs being periorbital oedema, eyelid retraction and lag, proptosis, conjunctival injection and chemosis, and diplopia (8); thyroid dermopathy, characterized by localized thickening and mild pigmentation of the skin, mostly seen in the pretibial area; thyroid acropachy, resembling clubbing of the fingers or toes, only in patients with dermopathy and severe orbitopathy (9). At variance with younger patients, older patients are often mildly symptomatic (10), but they are more likely to develop cardiovascular complications, primarily atrial fibrillation (11), a known, independent predictor of the occurrence of congestive heart failure in hyperthyroid subjects (12).
The diagnosis of Graves’ hyperthyroidism is based on characteristic clinical features and biochemical abnormalities. In the presence of typical signs and symptoms, serum TSH should always be measured, given its highest sensitivity and specificity in the diagnosis of thyroid disorders (13). When TSH is low or suppressed, serum free thyroxine (FT4) and free triiodothyronine (FT3) assessment allows to distinguish between subclinical hyperthyroidism (with normal circulating thyroid hormones) and overt hyperthyroidism (with increased circulating thyroid hormones).
In order to assess the cause of thyrotoxicosis, American Thyroid Association (ATA) and American Association of Clinical Endocrinologists (AACE) guidelines recommended a thyroid radioactive iodine uptake test (RAIU), unless diagnosis of Graves’disease is established clinically (14). Measurement of TSH-receptor antibodies (TRAb) is considered as an alternative way to diagnose Graves’disease, especially when the RAIU is unavailable or contraindicated. Positive TRAb provide strong supporting evidence for Graves’ disease. Thyroid ultrasound has high accuracy in the detection of any thyroid nodules and is helpful in the diagnosis of Graves’ disease in patients with concomitant nodular goiter; color-flow Doppler ultrasound detects increased vascularity of the gland. The use of thyroid ultrasound and assessment of TRAb is the preferred diagnostic approach for European (3,15) and Asian (16) endocrinologists. As the recent 2016 American Thyroid Association Guidelines emphasize, the choice of diagnostic testing can include measurement of TRAb, determination of the RAIU, or thyroid ultrasonography “depending on available expertise and resources” (17).
Once the diagnosis of Graves’ disease has been established, patients with overt hyperthyroidism should be treated with any of three effective and relatively safe initial treatment options: antithyroid drugs (ATDs), radioactive iodine ablation (RAI), and surgery (16). The choice of treatment differs depending upon geographical areas (18). In uncomplicated cases, ATDs represent the first-line treatment in most countries outside of USA, especially in Europe (19), but also in Asia, Oceania, and Latin America (15). Radioiodine treatment is frequently used as the first-line therapy in North America (15), though an increasing use of ATDs has been observed in recent years (20). The role of thyroid surgery as first-line treatment is limited worldwide. A 2011 survey investigating clinical practice patterns of providers who care for patients with uncomplicated Graves’ disease found less than 1% of respondents prefer surgery (15). Nevertheless, surgical option may be important in countries where facilities for RAI administration are not easily available or costs of long-term ATDs therapy cannot be afforded (20). None of the available therapeutic options is the best for all patients. Putting the patient at the centre of healthcare, considering patient’s preference, after receiving adequate counselling, remains a fundamental factor in the selection of therapy (20).
Although ATDs and RAI are effective and widely used treatment options for Graves’ disease (14,15), surgery is the most successful definitive treatment (21). When surgery is selected, total thyroidectomy is recommended, since the frequency of successful outcomes is significantly higher than with subtotal thyroidectomy (21), with no significant differences in the frequency of complications (22). Total (or near-total) thyroidectomy is associated with a lower risk of recurrent hyperthyroidism, with a slightly higher risk of transient hypoparathyroidism, but not with an increased risk of permanent hypoparathyroidism, recurrent laryngeal nerve palsy, or bleeding (23). Whenever surgery is chosen as the treatment of choice, selection of an expert high-volume thyroid surgeon is fundamental, because this is associated with an average lower risk of complications (17,20).
The main clinical situations that favor the choice of surgery as the treatment for Graves’ hyperthyroidism include: intolerance, ineffectiveness or recurrence after ATD treatment; conditions in which radioiodine therapy is contraindicated due to large goiter with or without symptomatic compression, relatively low uptake of radioactive iodine, documented or suspected thyroid malignancy, one or more large thyroid nodules, coexisting moderate-to-severe active Graves’ orbitopathy; major adverse effects to ATDs and liver disease; young patient age and women planning a pregnancy within 6 months; patients with periodic paralysis; coexisting primary hyperparathyroidism requiring surgery (14,17,24) (Table 1). In the above patients surgery is particularly recommended. Moreover, the surgical treatment selection, as any other therapeutic option, should take into account access to a high-volume thyroid surgeon, refuse or lack of facilities for RAI, and finally an individual preference for surgery (14). Patients choosing surgery consider that rapid and definitive control of hyperthyroidism, avoidance of exposure to radioactivity, and the potential, although rare, adverse reactions to ATDs are more important than surgical risks, and need for lifelong thyroid hormone replacement therapy (17).
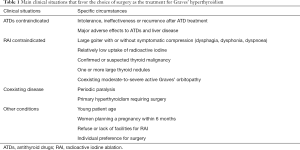
Full table
As regards the planning of surgery treatment, in the recent Consensus statement of the Italian Association of Endocrine Surgery Units (24), the waiting time for hospital admission is established within three months (“intermediate” priority) for hyperthyroidism unresponsive to medical treatment, and within twelve months (“low” priority) in stabilized hyperthyroid benign disease. In the event of coexisting suspicious or indeterminate nodules (nodular variant of Graves’ disease), the priority level should be “intermediate” (24).
When the patient is scheduled to undergo surgery, careful preoperative management is essential to optimize surgical outcomes. Pre-treatment with ATDs in order to promptly restore euthyroidism prior to surgery is recommended to minimize potential complications, particularly to avoid the risk of precipitating severe thyrotoxicosis (thyroid storm) during surgery. Thyroid storm is a rare disorder occurring in 1–5% of patients admitted to hospital for thyrotoxicosis, with a high mortality rate of 8–25% (25). Main triggering factors include thyroid or non-thyroid surgery and inappropriate use or discontinuation of ATDs, as well as acute illness, trauma, stress, and pregnancy. Diagnosis is based on the presence of hyperthyroidism in a patient with severe and life-threatening manifestations, such as hyperthermia, central nervous system effects (agitation, delirium, psychosis, extreme lethargy, seizure, coma), gastrointestinal and hepatic dysfunction (nausea and/or vomiting, abdominal pain, diarrhoea, jaundice), cardiovascular dysfunction (tachycardia, atrial fibrillation, and congestive heart failure) (26).
Available ATDs are methimazole, carbimazole (which is converted in methimazole, and not available in the United States), and propylthiouracil. These medications are actively transported into the thyroid, where they inhibit iodine organification and coupling of the iodothyronine residues, thus hampering thyroid hormone synthesis, and inhibit thyroid hormone release. Propylthiouracil in large doses also inhibits extrathyroidal deiodination of thyroxine (T4) to triiodothyronine (T3). Methimazole is the preferred drug in Graves’ disease, except during the first trimester of pregnancy and in patients with adverse reactions to methimazole. ATDs are generally well tolerated, although skin rash, urticaria, arthralgia, fever, nausea, abnormalities of taste and smell may occur in ≤5% of patients (17,26). Liver toxicity (more common with propylthiouracil; cholestatic for methimazole, and hepatocellular necrosis for propylthiouracil) and agranulocytosis are rare complications (≤0.1% and <0.2% respectively), usually occurring within the first few months of treatment, although they have been reported to occur at any time, particularly for propylthiouracil (26). Between the two regimens proposed for ATDs treatment, “titration” or “block and replace”, the former should be preferred as the first-line approach (17). In this case, the dose of ATD is titrated over time to the lowest dose needed for maintaining euthyroidism. The starting dose of methimazole, depending on the severity of the hyperthyroidism, ranges between 10–15 to 20–40 mg daily; the starting dose of propylthiouracil is usually 50–150 mg administered three times daily (17). For the majority of patients, euthyroidism is achieved after 6 weeks of treatment, and for almost all patients after 3 months. To assess efficacy of therapy and achievement of euthyroid state, serum T4 and T3 should be monitored, given that TSH might remain suppressed for several months. ATDs treatment should be stopped at the time of thyroidectomy (17).
Beta-blockers, such as propranolol (dosage 10–40 mg 3–4 times per day), can control the peripheral effects of excess thyroid hormones, in addition to slightly decreasing T4 to T3 conversion (17). For this reason, beta-blockers are often added effectively at the beginning of treatment to control hyperthyroid symptoms, particularly tachycardia, tremor, heat intolerance, and anxiety. Due to the longer half-life of T4, the beta-adrenergic blockers dose should be gradually weaned over the course of several days following surgery (17). Extreme caution and strict monitoring are recommended in patients with heart failure. Possible contraindications, such as asthma or bronchospasm, require special attention (17).
Thyroid gland in patients with Graves’ disease is very vascular, and thyroidectomy can be associated with higher rates of bleeding compared to thyroids not affected with Graves’ disease. Thus, using methods to reduce thyroid gland vascularity would be of benefit for thyroid surgeon. Inorganic iodide preoperatively reduces both thyroid hormone release and thyroid blood flow and vascularity, which in turn decreases intraoperative blood loss (27). Potassium iodide (short course of saturated solution of potassium iodide, SSKI) or potassium iodine (Lugol’s solution) have been used to prepare patients with Graves’ disease for surgery. In the past, a short course was used to control patient’s hyperthyroidism (the Wolff-Chaikoff effect) and decrease the likelihood and severity of an intra-operative or post-operative thyroid storm. Nowadays the rationale for their use preoperatively is to decrease the vascularity and friability of the thyroid gland, making thyroidectomy easier. In accordance with current American Thyroid Association (ATA) guidelines, a KI-containing preparation should be given before surgery in most patients with Graves’ disease (17). KI can be given as 5–7 drops (0.25–0.35 mL) of Lugol’s solution (8 mg iodide/drop) or 1–2 drops (0.05–0.1 mL) of SSKI (50 mg iodide/drop) three times daily mixed in water or juice for 10 days before surgery (17). Preparation to surgery with iodine drops (SSKI or Lugol’s solution) for 10–14 days prior to surgery seems, however, to be used by only one-third of respondents to a recent European survey (19).
Exceptional occurrences are the impossibility to achieve the euthyroid state before surgery, urgent need for thyroidectomy, or intolerance/allergy to ATDs. In all these cases, the patient should be adequately treated with beta-adrenergic blockade, KI, glucocorticoids, and potentially cholestyramine in the immediate preoperative period (17).
Glucocorticoids reduce T4 to T3 conversion and counteract the risk of adrenal insufficiency due to severe thyrotoxicosis (28). As in case of thyroid storm (17), hydrocortisone can be used, at a dose of 100 mg every 8 hours, after an intravenous loading dose of 300 mg, or dexamethasone at a dose of 2 mg twice a day, intravenously or orally (17).
Cholestyramine is an anionic exchange resin which has been shown to bind to iodothyronines in the gastrointestinal tract, lowering serum thyroid hormone concentrations when used in combination with thionamides and a β-adrenergic blocker. Thanks to its safety and efficacy, cholestyramine is a useful adjunctive therapy for preoperative preparation especially in patients with severe Graves’ disease that is resistant to conventional therapy (29). High-dose cholestyramine treatment (up to 12 g divided three times daily) has been also reported (30).
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1888-1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002;87:489-99. [Crossref] [PubMed]
- Zimmermann MB, Boelaert K. Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol 2015;3:286-95. [Crossref] [PubMed]
- Kahaly GJ, Bartalena L, Hegedüs L. The American Thyroid Association/American Association of Clinical Endocrinologists guidelines for hyperthyroidism and other causes of thyrotoxicosis: an European perspective. Thyroid 2011;21:585-91. [Crossref] [PubMed]
- Smith TJ, Hegedüs L. Graves' Disease. New Engl J Med 2016;375:1552-65. [Crossref] [PubMed]
- Devereaux D, Tewelde SZ. Hyperthyroidism and thyrotoxicosis. Emerg Med Clin North Am 2014;32:277-92. [Crossref] [PubMed]
- Goichot B, Caron P, Landron F, et al. Clinical presentation of hyperthyroidism in a large representative sample of outpatients in France: relationship with age, aetiology and hormonal parameters. Clin Endocrinol (Oxf) 2016;84:445-51. [Crossref] [PubMed]
- Bartalena L, Masiello E, Magri F, et al. The phenotype of newly diagnosed Graves'disease in Italy in recent years is milder then in the past:results of a large observational longitudinal study. J Endocrinol Invest 2016;39:1445-51. [Crossref] [PubMed]
- Bartalena L, Baldeschi L, Dickinson AJ, et al. Consensus statement of the European group on Graves' orbitopathy (EUGOGO) on management of Graves' orbitopathy. Thyroid 2008;18:333-46. [Crossref] [PubMed]
- Bartalena L, Fatourechi V. Extrathyroidal manifestations of Graves' disease: a 2014 update. J Endocrinol Invest 2014;37:691-700. [Crossref] [PubMed]
- Boelaert K, Torlinska B, Holder RL, et al. Older subjects with hyperthyroidism present with a paucity of symptoms and signs:a large cross-sectional study. J Clin Endocrinol Metab 2010;95:2715-26. [Crossref] [PubMed]
- Sawin CT, Geller A, Wolf PA, et al. Low serum thyrotropin concentration as a risk factor for atrial fibrillation in older persons. N Engl J Med 1994;331:1249-52. [Crossref] [PubMed]
- Siu CW, Yeung CY, Lau CP, et al. Incidence,clinical characteristics and outcome of congestive heart failure as the initial presentation in patients with primary hyperthyroidism. Heart 2007;93:483-7. [Crossref] [PubMed]
- Vaidya B, Pearce SH. Diagnosis and management of thyrotoxicosis. BMJ 2014;349:g5128. [Crossref] [PubMed]
- Bahn CR, Burch HB, Cooper DS, et al. American thyroid association and American association of clinical endocrinologists. Hyperthyroidism and other causes of thyrotoxicosis:management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid 2011;21:593-646. [Crossref] [PubMed]
- Burch HB, Burman KD, Cooper DS. A. 2011 survey of clinical practice patterns in the management of Graves' disease. J Clin Endocrinol Metab 2012;97:4549-58. [Crossref] [PubMed]
- Yamashita S, Amino N, Shong YK. The American thyroid association/American association of clinical endocrinologists guidelines for hyperthyroidism and other causes of thyrotoxicosis:viewpoints from Japan and Korea. Thyroid 2011;21:577-80. [Crossref] [PubMed]
- Ross DS, Burch HB, Cooper DS, et al. 2016 American thyroid association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid 2016;26:1343-421. [Crossref] [PubMed]
- Bartalena L. Diagnosis and management of Graves’ disease: a global overview. Nat Rev Endocrinol 2013;9:724-34. [Crossref] [PubMed]
- Bartalena L, Burch HB, Burman KD, et al. A 2013 European survey of clinical practice patterns in the management of Graves' disease. Clin Endocrinol (Oxf) 2016;84:115-20. [Crossref] [PubMed]
- Bartalena L, Chiovato L, Vitti P. Management of hyperthyroidism due to Graves’disease: frequently asked questions and answers (if any). J Endocrinol Invest 2016;39:1105-14. [Crossref] [PubMed]
- Genovese BM, Noureldine SI, Gleeson EM, et al. What is the best definitive treatment for Graves' disease? A systematic review of the existing literature. Ann Surg Oncol 2013;20:660-7. [Crossref] [PubMed]
- Bojic T, Paunovic I, Diklic A, et al. Total thyroidectomy as a method of choice in the treatment of Graves’ disease – analysis of 1432 patients. BMC Surg 2015;15:39. [Crossref] [PubMed]
- Guo Z, Yu P, Liu Z, et al. Total thyroidectomy vs bilateral subtotal thyroidectomy in patients with Graves’disease: a meta-analysis of randomized clinical trials. Clin Endocrinol (Oxf) 2013;79:739-46. [PubMed]
- Rosato L, De Crea C, Bellantone R, et al. Diagnostic, therapeutic and health-care management of the Italian Association of Endocrine Surgery Units (U.E.C. CLUB). J Endocrinol Invest 2016;39:939-53. [Crossref] [PubMed]
- Klubo-Gwiezdzinska J, Wartofsky L. Thyroid emergencies. Med Clin North Am 2012;96:385-403. [Crossref] [PubMed]
- De Leo S, Lee SY, Braverman LE. Hyperthyroidism. Lancet 2016;388:906-18. [Crossref] [PubMed]
- Erbil Y, Ozluk Y, Giris M, et al. Effect of lugol solution on thyroid gland blood flow and microvessel density in the patients with Graves'disease. J Clin Endocrinol Metab 2007;92:2182-9. [Crossref] [PubMed]
- Tsatsoulis A, Johnson EO, Kalogera CH, et al. The effect of thyrotoxicosis on adrenocortical reserve. Eur J Endocrinol 2000;142:231-5. [Crossref] [PubMed]
- Sebastian-Ochoa A, Quesada-Charneco MA, Reyes-Garcia R, et al. Dramatic response to cholestyramine in a patient with Graves'disease resistant to conventional therapy. Thyroid 2008;18:1115-7. [Crossref] [PubMed]
- Yang Y, Hwang S, Kim M, et al. Refractory Graves'disease successfully cured by adjunctive cholestyramine and subsequent total thyroidectomy. Endocrinol Metab (Seoul) 2015;30:620-5. [Crossref] [PubMed]


