Improving aesthetic outcomes in mastopexy with the “autoprosthesis” technique
Introduction
Mastopexy includes several types of skin incisions (inverted-T, vertical, circumareolar) and various types of parenchymal rearrangements.
Mastopexy could be also associated with breast augmentation to better fill the breast upper pole, being the combined procedure prone to higher complication rates and re-interventions.
Mastopexy represents a simple surgical procedure with low complication rates but long-term outcomes and upper pole adequate fullness have been questioned by some authors (1).
Several techniques have been developed trying to obtain better stability of the results and upper pole fullness, such as parenchymal redistribution, parenchymal fixation to the pectoralis fascia or under a loop of pectoralis major muscle, use of synthetic meshes or autoaugmentation (2-14).
Other authors also describe an autoaugmentation with the use of a deepithelialized flap from the lateral chest wall or upper abdomen (15).
No controlled studies compared those techniques in order to evaluate the safety and efficacy of any of them in association with skin-only mastopexy.
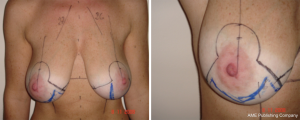
We present a parenchymal rearrangement technique allowing better upper pole fullness and nipple-areola-complex (NAC) projection when performing a mastopexy, with a combination of a superior pedicle for the NAC and an inferiorly-based parenchymal flap, the so-called “autoprosthesis”.
Methods
From January 2008 to June 2015, we performed the autoprosthesis technique for mastopexy in 184 patients. Mean patients’ age was 42 years (range, 26–65 years). We evaluated complications (seroma, hematoma, wound infection and/or dehiscence) with a mean follow-up of 39 months (range, 6–78 months).
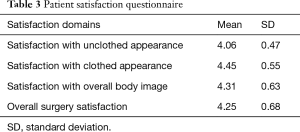
A questionnaire to evaluate patients’ satisfaction level was administered after the surgical procedure at a follow-up of 6–12 months, asking patients to grade their satisfaction with their unclothed appearance, clothed appearance, overall body image and overall surgery satisfaction on a scale from “not at all satisfied” =1 to “very satisfied” =5.
We considered the “autoprosthesis” technique for patients with moderate/severe ptotic breast (sternal notch-nipple distance >22 cm and nipple-inframammary fold distance >8 cm).
We firmly believe that the main driver towards the use or not of an implant in mastopexy is patient’s satisfaction with her breast volume when wearing a push-up bra: if satisfied with volume, the surgeon will be able to safely use the “autoprosthesis” technique (inferior dermoglandular flap), otherwise the use of an implant in order to achieve upper-pole fullness could be advisable.
Surgical technique
The technique can be performed using a superiorly based nipple-areola complex pedicle (superior, superomedial, and superolateral) with both vertical and Wise pattern techniques.
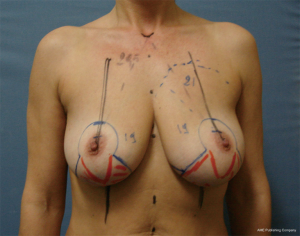
With the patient in an upright, symmetrically equal posture, pre-operative markings are signed the same way as for conventional Wise pattern or vertical reduction mammaplasty with the exception of drawing the inferior flap at the central part of the lower pole of the breast, in the portion to be usually resected in reduction techniques. Flaps of different sizes can be planned according to tissue availability and the grade of breast projection and upper pole fullness needed.
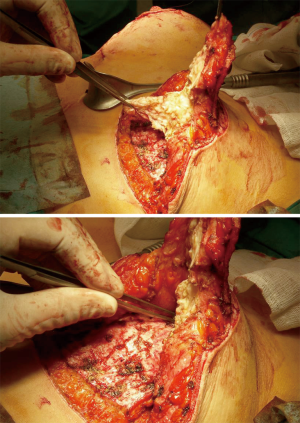
The inferiorly based dermoglandular flap is raised on the lower pole of the breast. The flap receives a reliable vascular supply from the fourth, fifth, and sixth intercostal perforating vessels of the internal mammary arteries. Venous drainage flows into the internal mammary vein.
The flap dermal layer represents a sustaining and pliable scaffold, allowing a durable suspension of the flap to the pectoralis fascia and a valuable reshaping of the flap according to the breast contour to address.
The fat/glandular layers accounts for the volume of the breast, ensuring soft-tissue envelope stretching with balanced upper and lower quadrants fullness and enduring breast mound projection.
As for any superior pedicle breast reduction, incisions are made raising a proximally based dermal flap holder of the nipple-areola complex at its edge, removing skin and a variable amount of breast tissue medially and laterally and raising the inferior thoracic flap directly perpendicular to the prepectoral fascia at its own two lateral sides.
The superior dissection is performed in a slightly oblique fashion under the nipple but onto the prepectoral fascia to ensure easy tunnelling of the flap, avoiding an excessive bulging effect after flap placement.
Dissection proceeds detaching the breast tissue superiorly off the prepectoral fascia, letting smooth flap placement underneath it, ensuring enough superior fullness (Figure 1).
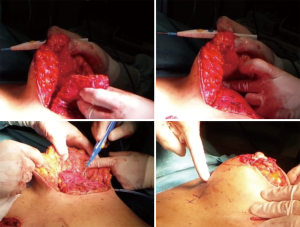
Referring to pre-operative skin markings, the breast parenchymal de-epithelialized flap is then sutured superiorly, supero-medially or supero-laterally to the prepectoral fascia with long absorbable or permanent sutures, according to the breast shape to address, in order to fill up the upper quadrants of the breast and to enhance projection of the breast mound.
The flap could also be tailored with sutures in a conical shape when further projection is required. Another useful surgical trick in order to emphasize projection is the split of the superior pedicle (Figure 2).
With the patient in the seated position (60 to 90 degrees), the breast mound is then synthesized, with the suture of the medial and lateral pillars to each other above the inferior flap.
Results
All patients in the study underwent a superior or supero-medial pedicle mastopexy in association with the “autoprosthesis” to better fill the upper pole and to improve breast projection (patient characteristics reported in Table 1) (Figures 3-7).
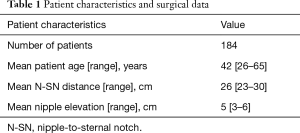
Full table



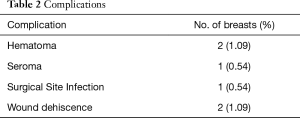
Complications (seroma, hematoma, surgical site infection, wound dehiscence) at a mean follow-up of 39 months (range, 6–78 months) are summarized in Table 2.
Full table
Patients’ satisfaction was high among the patients who underwent bilateral mastopexy with the autoprosthesis technique regarding the satisfaction with their clothed and unclothed appearance and overall body image (Table 3).
Full table
Discussion
An inferiorly-based parenchymal flap to reach breast upper pole fullness and to improve breast projection was first described by Ribeiro and Backer in 1973 (16).
The flap, as described by Ribeiro, is fit out at the level of the lower pole of the breast that is usually resected in a superior pedicle breast reduction and is designed as an autologous implant to be fixed to the pectoralis major muscular plane.
It represents a lightweight flap with good outcomes in the long-term follow-up not being affected by bottoming out, improving upper pole fullness and breast projection.
No controlled studies are available in literature comparing different surgical methods for mastopexy, most being small case series or case reports, that is level IV or V evidences, so we cannot conclude data augmentation to be more reliable in terms of stability of results when compared with skin-only mastopexy procedures or other parenchymal rearrangement or fixation techniques. A meta-analysis by Swanson concluded about the absence of superiority of any mastopexy method in terms of breast upper pole fullness and projection (2).
The stability of the result, in particular in relation of breast upper pole fullness is the greatest challenge when performing a mastopexy. We firmly believe that the autoprosthesis technique could allow the plastic surgeon to partially win the struggle with gravity, thanks to the inferiorly-based parenchymal flap that is fixed to the pectoralis major muscle, improving breast projection and reaching long-lasting upper-pole fullness.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: No institutional ethics committee approval was required for our study being the technique already validated. Written informed consent was obtained from all patients.
References
- Goulian D Jr. Dermal mastopexy. Plast Reconstr Surg 1971;47:105-10. [Crossref] [PubMed]
- Swanson E. A retrospective photometric study of 82 published reports of mastopexy and breast reduction. Plast Reconstr Surg 2011;128:1282-301. [Crossref] [PubMed]
- Flowers RS, Smith EM Jr. "Flip-flap" mastopexy. Aesthetic Plast Surg 1998;22:425-9. [Crossref] [PubMed]
- de la Plaza R, de la Cruz L, Moreno C. Mastopexy utilizing a dermoglandular hammock flap. Aesthet Surg J 2005;25:31-6. [Crossref] [PubMed]
- Ritz M, Silfen R, Southwick G. Fascial suspension mastopexy. Plast Reconstr Surg 2006;117:86-94. [Crossref] [PubMed]
- Colwell AS, Driscoll D, Breuing KH. Mastopexy techniques after massive weight loss: an algorithmic approach and review of the literature. Ann Plast Surg 2009;63:28-33. [Crossref] [PubMed]
- Lejour M. Vertical mammaplasty and liposuction of the breast. Plast Reconstr Surg 1994;94:100-14. [Crossref] [PubMed]
- Kim P, Kim KK, Casas LA. Superior pedicle autoaugmentation mastopexy: a review of 34 consecutive patients. Aesthet Surg J 2010;30:201-10. [Crossref] [PubMed]
- Hall-Findlay EJ. Pedicles in vertical breast reduction and mastopexy. Clin Plast Surg 2002;29:379-91. [Crossref] [PubMed]
- Foustanos A, Zavrides H. A double-flap technique: an alternative mastopexy approach. Plast Reconstr Surg 2007;120:55-60. [Crossref] [PubMed]
- Graf R, Biggs TM. In search of better shape in mastopexy and reduction mammoplasty. Plast Reconstr Surg 2002;110:309-17. [Crossref] [PubMed]
- Graf R, Reis de Araujo LR, Rippel R, et al. Reduction mammaplasty and mastopexy using the vertical scar and thoracic wall flap technique. Aesthetic Plast Surg 2003;27:6-12. [Crossref] [PubMed]
- Hammond DC, Alfonso D, Khuthaila DK. Mastopexy using the short scar periareolar inferior pedicle reduction technique. Plast Reconstr Surg 2008;121:1533-9. [Crossref] [PubMed]
- Bonomi S, Salval A, Settembrini F, et al. Inferiorly based parenchymal flap mammaplasty: a safe, reliable, and versatile technique for breast reduction and mastopexy. Plast Reconstr Surg 2012;130:116e-25e. [Crossref] [PubMed]
- Losken A, Holtz DJ. Versatility of the superomedial pedicle in managing the massive weight loss breast: the rotation-advancement technique. Plast Reconstr Surg 2007;120:1060-8. [Crossref] [PubMed]
- Ribeiro L, Backer E. Mastoplastia com pediculo de siguridad. Rev Esp Cir Plast 1973;16:223-7.


