Oncoplastic round block technique has comparable operative parameters as standard wide local excision: a matched case-control study
Introduction
Oncoplastic surgery is the use of plastic surgery techniques in breast cancer surgery to achieve resection of the tumor while maintaining a good cosmetic outcome. These oncoplastic techniques were broadly classified into levels I and II (1). Various level II techniques such as round block and inverted T etc. have been described with their specific indications. Although oncoplastic surgery has been used to resect larger tumors with lower re-excision rates compared to standard wide local excision (sWLE) (2), criticisms of oncoplastic surgery compared to sWLE include a longer, albeit often well-concealed scar (3), longer operating time and length of stay (4), possible increased complications such as necrosis of nipple areolar complex and wound dehiscence (5,6).
Round block technique, also known as Benelli or Doughnut mastopexy (7), has been reported to be a useful level II oncoplastic technique well suited for women with relatively smaller breast size and minimal ptosis (8,9). Being a slightly less complicated procedure compared to other level II oncoplastic techniques, round block may have fewer of the possible complications associated with oncoplastic surgery. We aim to determine if round block technique will result in comparable operative parameters, such as length of operation and hospital stay, with sWLE for breast cancer patients. This is one of the few studies, to our knowledge, which aims to contrast the operative parameters of the round block technique with the sWLE.
Methods
Breast cancer patients, with histologically proven malignancy on biopsy, who underwent a round block procedure by a single surgeon from 1st May 2014 till 31st January 2016, at a tertiary institution, were included in the study. These patients were then matched for the type of axillary procedure, on a one to one basis, with breast cancer patients, operated by the same surgeon, who had undergone sWLE from 1st August 2011 till 31st January 2016.
Eligibility for the round block technique included patients with a large tumor to breast ratio desiring breast conservation, patients with multifocal/multicentric breast tumors who would otherwise require mastectomy, and patients with slight breast asymmetry and tumor in the larger breast who wished to achieve breast symmetry post-surgery. Exclusions for the round block technique included patients unfit for surgery, heavy smokers, patients with severe ptosis or a central tumor involving the nipple areolar complex. In addition, patients undergoing other reconstructive procedures in the same setting as the round block technique were excluded from the study, as this would inevitably lengthen operating time. Patients undergoing wide local excision with local chest wall perforator flap reconstruction or requiring removal of the nipple areolar complex owing to a central tumor were excluded from the study.
Round block was performed by first de-epithelializing a rim of skin around the areola. The tumor was then accessed via an incision through the de-epithelialized skin, leaving the nipple areolar complex vascularized on the dermal pedicle. The breast tissue was then dissected as much as possible to allow complete resection of the tumor and remodeling to cover the tumor defect. A purse-string was then done to approximate the incision opening to match the size of the contralateral areola. The neo-areola was recentralized and fixed in the four quadrants. Skin closure was completed as described in the classic round block procedure. Contralateral symmetricalisation was not performed during the same setting. SWLE was performed via a periareolar approach, or via an incision in a cosmetically pleasing location such as an inframammary fold, if the periareolar approach was not possible. Shave margins were obtained in both groups of patients.
If sentinel lymph node biopsy was indicated, it would be performed prior to the sWLE or round block procedure so as to minimize the waiting time for the frozen section result. If the frozen section was positive for malignancy, an axillary clearance would be performed during the same setting.
Operative parameters such as operating time, length of hospital stay and surgical complications such as breast edema, hematoma, infection, wound dehiscence etc., patient’s demographics, pathologic characteristics, re-excision rates, clinical and cosmetic outcome of patients were collected. The cosmetic outcome was assessed by the surgeon and patients as excellent, good, fair or poor using Harris classification (10). If the patient had multicentric/multifocal disease, the tumor size was recorded as that of the largest foci of tumor. The adjuvant treatment of these patients was subsequently determined in a multidisciplinary meeting.
Statistical analysis was performed using SAS V9.4 (SAS Inc., Cary, NC, USA). Continuous variables were summarized using mean (SD) or median (IQR). Owing to the one-to-one patient matching, continuous variables were compared statistically using a paired t-test and medians using a Wilcoxon signed-rank test. In addition, the non-parametric Hodges-Lehmann estimate of location shift with exact 95% confidence interval was applied to the performance parameters, operating time and length of stay. McNemar’s exact test on variables with binary outcomes. Categorical baseline variables were compared using either McNemar’s exact test for binary outcomes or a generalized logit model taking into account the matching in the case of multinomial outcomes. Patients who were lost to follow up were excluded from analysis. Statistical significance was set at P≤0.05.
This study was approved by SingHealth Centralised Institutional Review Board.
Results
A total of 11 patients who underwent round block technique were included in the study. These 11 patients were matched with another 11 patients who underwent sWLE by the type of axillary procedure being performed. 2 patients had no axillary procedure, 7 had sentinel lymph node biopsy alone, 1 had sentinel lymph node biopsy and axillary clearance and 1 patient had upfront axillary clearance.
The patients’ demographics such as age, American Society Anaesthesiologists Physical Status (ASA), site of tumor, Body Mass Index (BMI) and chemotherapy status were similar in both groups (Table 1). There was no smoker in either group.
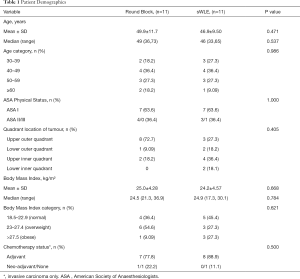
Full table
The 2 groups also had comparable pathologic parameters (Table 2) with majority of the patients having invasive ductal cancer (IDC). More patients in the round block group presented with multifocal/multicentric lesions (36.4%) than in the sWLE group (27.3%). The mean tumor size was comparable in the two groups (P=0.94) but the re-excision rate was higher in the sWLE group (18.2%) than in the round block group (9.1%). Completion mastectomy rate was similar in both groups (9.1%).
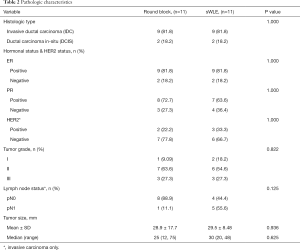
Full table
In the sWLE group, 6 patients had a periareolar incision with or without a radial extension, 2 patients had an incision over the tumor and the remaining patients had an axillary or inframammary incision. The median distance from the nipple to the tumor was 35mm (range: 19–75 mm) and 50 mm (range: 20–70 mm) in the round block and sWLE groups, respectively.
These two groups of patients were similar in their breast size and ptosis with the majority of patients (90.9%) having grade I-II ptosis. One patient with grade III ptosis underwent a round block as she had slight breast asymmetry and tumor in the larger breast who wanted to achieve breast symmetry post operation. Mean cosmetic outcome, assessed by the surgeon and patients, was rated to be excellent/good in 10 round block (90.9%) and 6 sWLE (54.6%) patients, respectively (P=0.149). The 5 sWLE patients with fair/poor cosmetic outcome were not given the option of oncoplastic breast conserving surgery, as the operating surgeon had not yet begun to do oncoplastic breast conserving surgery at the time of their operations. This could hence account for the difference in the cosmetic outcome between the two groups.
Operating time and length of hospital stay did not differ statistically between groups (Table 3) with mean operating time of 122 and 114 minutes for the round block and sWLE groups, respectively (P=0.64). Mean length of hospital stay was 1.6 and 2.2 days for the round block and sWLE groups, respectively (P=0.11). There was no reported surgical complications in either group.

Full table
Patients were followed up through October 2016. The follow-up time was calculated from the date of diagnosis to the last known date of follow up or upon recurrence or metastasis, whichever occurred first. Median follow-up time (range) for the round block and sWLE groups was 24 [11,29] and 50 [10,60] months, respectively. All patients had radiotherapy post operation except for the patients who had completion mastectomy. There was no recurrence in the round block group, and 2 patients in the sWLE group had locoregional recurrence.
Discussion
Our study demonstrated that the round block technique has comparable operating time and length of stay to sWLE with a lower re-excision rate and better cosmetic outcomes. While many studies (2,11,12) have compared oncological safety of oncoplastic surgery to sWLE, there are few publications comparing the operative parameters of round block surgery to sWLE.
Round block has been shown to be well suited in women with smaller breasts and minimal ptosis (8,9). Though leaving a longer scar (3) compared to a periareolar approach in sWLE, the round block circumferential periareolar scar is often well concealed, making it cosmetically pleasing. Despite having a longer incision to suture and additional steps of de-epithelisation of the skin and purse-string of the neo-areolar opening (3) compared to sWLE, the round block technique can have comparable operating time to sWLE, as shown in our study. This could be attributable to the larger diameter of exposure provided by the de-epithelisation of the skin, allowing better access and visualization of the tumor, hence reducing the overall operating time.
The length of hospital stay was similar in both groups, as there were no surgical complications observed. Although the round block technique has been associated specifically with the disadvantage of late onset widening of the neo-areolar opening (13), this was minimized in our series by using a permanent suture for the purse-string of the neo-areola, and no cases have been reported in this study at the 1-year follow up.
The round block group also had a lower re-excision rate despite having more patients with multifocal/multicentric lesions. Although consistent with the literature that oncoplastic surgery has a lower re-excision rate than sWLE (2,11), the re-excision rate in our study is higher than the reported rate of 4% (2). We attribute this to the small sample size and associated uncertainty in the estimate. Our completion mastectomy rate was similar in both groups, although higher completion mastectomy rates have been reported for oncoplastic surgery in the literature (2).
In our study, mean maximum tumor size was similar in both groups, although it has been shown in literature that oncoplastic breast conserving surgery allows removal of a larger tumor compared to sWLE (2,11). This was partly because prior to oncoplastic breast conserving surgery being performed by the operating surgeon at our institution, those patients with a larger tumor to breast ratio, who were keen for breast conserving, were only offered sWLE. The sWLE patients with tumor size comparable to patients in the round block group inevitably had a poorer cosmetic outcomes than patients in the round block group. Only 45.5% of patients in the sWLE group reported a good/excellent cosmetic outcome whereas the percentage in patients with comparable tumor size in the round block group was 90.9%. This demonstrates the advantage of the oncoplastic technique to resect a larger tumor and yet achieve a good cosmetic outcome (14).
An additional advantage of the round block technique over sWLE was the ability to correct asymmetry in the breasts, especially in those patients whose tumor was in the larger breast—as occurred in 18.2% of our round block patients. The round block group also had more patients with multifocal/multicentric lesions which were considered a relative contraindication to breast conserving surgery (15).
Our study is the largest known to date comparing operative parameters of round block without contralateral symmetricalisation to sWLE. We encountered one other similar paper (3), which also found comparability in length of hospital stay and operating time in 7 round block patients without contralateral symmetricalisation. In that study however, all sWLE patients underwent direct incision over the tumor in contrast to the predominantly periareolar or cosmetically pleasing incision in our study which requires the additional step of raising the skin flap to access the tumor and hence results in a longer operating time. Also, tumor size in our study was larger. Despite these differences, our study reported comparable operating time between the two techniques.
Our study is not without limitations. It is a small retrospective series, and the follow up of the round block patients was relatively short compared to the sWLE group which could account for the fewer instances of recurrence in the round block group. Ideally, the exact operating time of the round block procedure should be contrasted directly with the operating time for the sWLE without taking into account the axillary procedure. This is not always possible as a practical matter. There are times when the axillary procedure and breast surgery are performed concurrently, and it is not possible to define a clear cutoff time for the breast surgery alone. This is especially true when the WLE is performed via the same incision as the axillary procedure by using the axillary crease for an upper outer breast cancer quadrant.
Although some may argue that the constitution of the scrub team members will alter the operating time (16,17), bias from this source was kept to a minimum as the scrub team members remained constant during the study period and comprised an anesthetist, a scrub nurse, a surgeon and an operating assistant. Also, bias was further reduced by having a single surgeon perform the series, which eliminated inter-surgeon operating experience (18) as a factor affecting operating time. In addition, patient demographic and clinical characteristics such as ASA and BMI, and tumor characteristics such as size and lymph node status, which could potentially affect the operating time, were similar in both groups, further reducing bias. Although results of this study were promising, they are best validated by larger, future prospective studies.
Conclusions
The round block technique has comparable operative parameters to sWLE with no evidence of increased surgical complications, contrary to the perceived disadvantages associated with oncoplastic surgery. A lower re-excision rate and better cosmesis were observed in the round block patients suggesting that the round block technique is not only comparable in general, but may have advantages to sWLE in selected cases.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by SingHealth Centralised Institutional Review Board, and written informed consent was obtained from all patients.
References
- Clough KB, Kaufman GJ, Nos C, et al. Improving breast cancer surgery: A classification and quadrant per quadrant atlas for oncoplastic surgery. Ann Surg Oncol 2010;17:1375-91. [Crossref] [PubMed]
- Losken A, Dugal CS, Styblo TM, et al. A meta-analysis comparing breast conservation therapy alone to the oncoplastic technique. Ann Plast Surg 2014;72:145-9. [Crossref] [PubMed]
- Giacalone PL, Dubon O, Roger P, et al. Doughnut mastopexy lumpectomy versus standard lumpectomy in breast cancer surgery: a prospective study. Eur J Surg Oncol 2007;33:301-6. [Crossref] [PubMed]
- Lima DE, Veiga Filho J, Ribeiro LM, et al. Oncoplastic approach in the conservative treatment of breast cancer: analysis of costs. Acta Cir Bras 2012;27:311-4. [Crossref] [PubMed]
- Clough KB, Lewis J, Couturaud B, et al. Oncoplastic techniques allow extensive resections for breast-conserving therapy of breast carcinomas. Ann Surg 2003;237:26-34. [Crossref] [PubMed]
- Iwuchukwu OC, Harvey JR, Dordea M, et al. The role of oncoplastic therapeutic mammoplasty in breast cancer surgery-a review. Surg Oncol 2012;21:133-41. [Crossref] [PubMed]
- Benelli L. A new periareolar mammaplasty: the “round block technique’’. Aesthetic Plast Surg 1990;14:93-100. [Crossref] [PubMed]
- Yang JD, Bae SG, Chung HY, et al. The usefulness of oncoplastic volume displacement techniques in the superiorly located breast cancers for Korean patients with small to moderate-sized breasts. Ann Plast Surg 2011;67:474-80. [Crossref] [PubMed]
- Lim G, Pineda LA. Applicability of Oncoplastic Breast Conserving Surgery in Asian Breast Cancer Patients. Asian Pac J Cancer Prev 2016;17:3325-8. [PubMed]
- Harris JR, Levene MB, Svensson G, et al. Analysis of cosmetic results following primary radiation therapy for stages I and II carcinoma of the breast. Int J Radiat Oncol Biol Phys 1979;5:257-61. [Crossref] [PubMed]
- Chakravorty A, Shrestha AK, Sanmugalingam N, et al. How safe is oncoplastic breast conservation? Comparative analysis with standard breast conserving surgery. Eur J Surg Oncol 2012;38:395-8. [Crossref] [PubMed]
- Fitoussi AD, Berry MG, Fama F, et al. Oncoplastic breast surgery for cancer: Analysis of 540 consecutive cases. Plast Reconstr Surg 2010;125:454-62. [Crossref] [PubMed]
- Zaha H, Onomura M, Unesoko M. A new scarless oncoplastic breast-conserving surgery: modified round block technique. Breast 2013;22:1184-8. [Crossref] [PubMed]
- Adimulam G, Challa VR, Dhar A, et al. Assessment of cosmetic outcome of oncoplastic breast conservation surgery in women with early breast cancer: a prospective cohort study. Indian J Cancer 2014;51:58-62. [Crossref] [PubMed]
- Gentilini O, Botteri E, Rotmensz N, et al. Conservative surgery in patients with multifocal/multicentric breast cancer. Breast Cancer Res Treat 2009;113:577-83. [Crossref] [PubMed]
- Gillespie BM, Chaboyer W, Fairweather N. Factors that influence the expected length of operation: Results of a prospective study. BMJ Qual Saf 2012;21:3-12. [Crossref] [PubMed]
- Xu R, Carty MJ, Orgill DP, et al. The teaming curve: A longitudinal study of the influence of surgical team familiarity on operative time. Ann Surg 2013;258:953-7. [Crossref] [PubMed]
- Maruthappu M, Duclos A, Zhou CD, et al. The impact of team familiarity and surgical experience on operative efficiency: A retrospective analysis. J R Soc Med 2016;109:147-53. [Crossref] [PubMed]


