Thermal injury in TAPIA breast reconstruction—thermal injury to thoracodorsal artery perforator flap
Introduction
A recently published paper describes the TAPIA method for delayed breast reconstruction (1). When this technique is used the patients mobilize quickly following the reconstruction and postoperative complications seem scarce. However, in two cases thermal injury to the reconstructed breast has been an unforeseen consequence of indirect sun exposure.
Thermal injuries after flap-based breast reconstruction are described in the literature (2-11). This is mainly due to the patients lacking the ability to detect nociceptive stimuli from the denervated flap and thereby act appropriately. We report the first two cases of thermal injury in a TAP-flap occurring in the early period after delayed breast reconstruction.
Case presentation
Case 1
In 2004 a 61-year-old woman received a right-sided mastectomy and axillary lymph node for invasive ductal carcinoma. No adjuvant therapy was offered her. The patient was a non-smoker without comorbidity.
In 2013 she was referred for delayed breast reconstruction. She was found eligible for reconstruction by the TAPIA method using a 375 cc silicone implant. The procedure was performed in late May and the postoperative course was uneventful. The patient was discharged after eight days and scheduled for a clinical control 15 days postoperative.
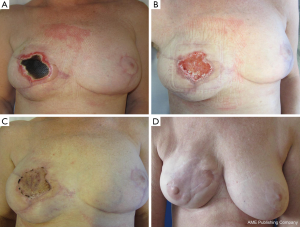
In the outpatient clinic the patient presented with a full-thickness skin burn on the medial part of flap, measuring 8 cm × 4 cm (Figure 1A,B). This burn had occurred whilst the patient had been sitting outside in warm weather wearing a black T-shirt. The flap had not been exposed to direct sunlight. The full-thickness skin burn was debrided revealing viable tissue underneath, enabling the defect to be covered with a split-thickness skin graft (Figure 1C). The healing was uneventful. The patient has since refrained from nipple areola complex reconstruction and is satisfied with the result (Figure 1D).

Case 2
A 48-year-old woman diagnosed with invasive ductal carcinoma in 2001 was treated by a right-sided mastectomy without adjuvant therapy. The patient was a non-smoker and apart from well-treated hypertension she had no comorbidity. She was reconstructed by the TAPIA method in April 2013 using a 365 cc Becker implant. She was discharged day 11 after an uneventful postoperative course.
The patient presented with a satisfying result at the first postoperative control in the outpatient clinic three weeks after surgery. However, one week later she presented with a full-thickness skin burn, measuring 8 cm × 6 cm (Figure 2A). She too had been exposed to the sun in hot weather wearing a dark shirt not exposing the flap to direct sunlight. The defect was debrided, revealing a viable flap underneath (Figure 2B). We applied negative pressure wound therapy for 14 days and then covered the defect with a full-thickness skin graft (Figure 2C). The nipple areola complex have since been reconstructed using a skate-flap and a tattoo (Figure 2D).
Discussion
Thermal injury following breast reconstructions is a rare incident. The first case was reported more than two decades ago and since only few cases have been reported and compiled in two literary reviews (9,11). Most of the published material covers complete autologous reconstructions using either DIEP or TRAM flaps.
The most frequent cause of thermal injury to the flaps seems to be heat exposure due to sunlight most often when the patient has been wearing dark clothes or bathing suits (3,9). The extent of the injury varies but most published cases have been treated conservatively. Approximately 16% required surgical revision and application of a skin graft (11).
The etiology behind the increased risk of thermal injury is multi factorial. It is well documented that the sensibility of a reconstructed breast is scarce, especially in the initial period following reconstruction (9). The reconstruction seems to be most susceptible to thermal injury in the early postoperative period. However, the flaps tend to regain some autoregulation and sensitivity over time, however the duration may depend on the type of flap (3).
The impaired or absent sensation may be the most important factor leading to increased risk of thermal injury. However, other thermoregulative capacities of the flaps such as sweating and vasodilation is probably also inhibited due to an affected or absent autonomic regulation. This adds to the increased susceptibility to thermal injury (3). Furthermore the thickness of the flap is invers correlated to the risk of thermal injury, thus a thinner flap is at greater risk of thermal injury (10). The type of flap and its properties may perhaps also affect the overall susceptible to thermal damage.
Thermal injuries to the Latissimus Dorsi flap (LD-flap) seem less frequent than those of the abdominal flaps and caused by more severe or direct heat exposure, such as application of an electric heat pad or hot water bottle (7). This may be due to the flaps general properties with some degree of preserved innervation, a solid blood supply and the mere thickness of the LD-flap.
When the TAP-flap is used for total breast reconstruction it is harvested as a pedicled propeller perforator-based flap, which in most cases leaves the flap totally denervated. The thermoregulative capabilities are not only compromised by the denervation and limited blood flow through the perforator(s), but also due to the rather thin flap design. In comparison to the LD-flap the TAP-flap may be more prone to thermal injury due to all of these factors.
As a consequence we find that patients should be informed of the risk of thermal injury following total breast reconstruction using a TAP flap. We recommend that they avoid heat exposure in the initial three months following reconstruction.
Conclusions
When using the TAPIA technique for breast reconstruction it is important to inform patients of the risks of thermal injury. The patients should be instructed to avoid heat exposure in the initial period after the reconstruction.
Acknowledgements
None.
Footnote
Conflicts of Interest: These authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Børsen-Koch M, Gunnarsson GL, Udesen A, et al. Direct delayed breast reconstruction with TAP flap, implant and acellular dermal matrix (TAPIA). J Plast Reconstr Aesthet Surg 2015;68:815-21. [Crossref] [PubMed]
- Maxwell GP, Tornambe R. Second- and third-degree burns as a complication in breast reconstruction. Ann Plast Surg 1989;22:386-90. [Crossref] [PubMed]
- Alexandrides IJ, Shestak KC, Noone RB. Thermal injuries following TRAM flap breast reconstruction. Ann Plast Surg 1997;38:335-41. [Crossref] [PubMed]
- Beckenstein MS, Beegle PH, Hartrampf CR Jr. Thermal injury to TRAM flaps: a report of five cases. Plast Reconstr Surg 1997;99:1606-9. [Crossref] [PubMed]
- Aslam A, Khoo CT. No sense; no sensibility--a tale of two adult hairdrier burns. Burns 1997;23:454-7. [Crossref] [PubMed]
- Nahabedian MY, McGibbon BM. Thermal injuries in autogenous tissue breast reconstruction. Br J Plast Surg 1998;51:599-602. [Crossref] [PubMed]
- Agarwal SK, Williams MR. Burn injuries after latissimus dorsi breast reconstruction in a cold climate. Breast 2002;11:270-2. [Crossref] [PubMed]
- Delfino S, Brunetti B, Toto V, et al. Burn after breast reconstruction. Burns 2008;34:873-7. [Crossref] [PubMed]
- Enajat M, Rozen WM, Audolfsson T, et al. Thermal injuries in the insensate deep inferior epigastric artery perforator flap: case series and literature review on mechanisms of injury. Microsurgery 2009;29:214-7. [Crossref] [PubMed]
- Delfino S, Brunetti B, Toto V, et al. Does tissue expansion increase skin susceptibility to thermal injury? A physical model. Burns 2009;35:1054-5. [Crossref] [PubMed]
- Mohanna PN, Raveendran SS, Ross DA, et al. Thermal injuries to autologous breast reconstructions and their donor sites--literature review and report of six cases. J Plast Reconstr Aesthet Surg 2010;63:e255-60. [Crossref] [PubMed]


