Sinusoidal hemangioma of the breast: diagnostic evaluation management and literature review
Introduction
Vascular tumors of the breast are rare and may pose a diagnostic challenge. Benign vascular tumors include hemangioma, lymphangioma and angiolipoma whereas malignant tumors include hemangiosarcoma and hemangiopericytoma (1). Hemangioma of the breast is a rare benign vascular tumor accounting for 0.4% of all breast tumors (2). It is found in approximately 1.2% of mastectomy specimens and in 11% of postmortem specimens in females (3,4). In a retrospective review of 10,000 breast biopsies performed within a 10-year period, Glazebrook et al. (5) found only 18 cases of benign vascular tumors. Fifteen of these cases were hemangiomas and three were angiolipomas. Breast hemangioma is usually very small and asymptomatic and is discovered incidentally in biopsies performed for unrelated reasons (6,7). Breast hemangioma presenting as a palpable tumor is a very rare clinical entity (8,9). We present here a very rare case of sinusoidal hemangioma of the breast in a postmenopausal patient with atypical imaging features that prompted surgical intervention. Diagnostic evaluation and management of the patient are discussed along with a review of the relevant literature.
Case presentation
A 59-year-old Caucasian female presented to our breast clinic with a 1-year history of a palpable right breast lump slowly increasing in size. She denied any other symptoms. Her past medical history was unremarkable and she had no family history of breast or ovarian cancer. She had menarche at the age 13, went through the menopause at age 55 and she had never used any type of oral contraceptives.
On clinical examination, a non-tender well-circumscribed mass measuring approximately 1 cm × 1 cm was palpated in the lower-inner quadrant of her right breast, associated with a mild bluish-red discoloration of the overlying skin. There was no nipple discharge whereas there were no palpable axillary or supraclavicular lymph nodes.
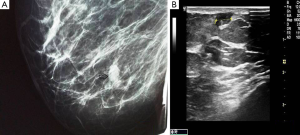
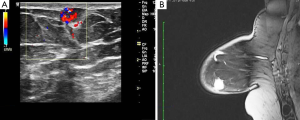
Mammography showed a relatively well-defined mass with sparse calcifications (Figure 1A), whereas ultrasonography revealed a circumscribed microlobulated hypoechoic mass measuring 1cm without posterior acoustic enhancement (Figure 1B). On color Doppler examination the mass exhibited marked hypervascularity (Figure 2A). A breast magnetic resonance imaging (MRI) was obtained and demonstrated a nodule measuring 1cm with partially irregular margins located 9 cm from the nipple in the lower inner quadrant of the right breast (Figure 2B). After contrast administration a rapid increase of the signal intensity was noted followed by a wash out curve in the delayed phase and thus the lesion was classified as BIRADS category 5. Cytology examination was not performed because a repeated aspiration of the nodule yielded only blood.
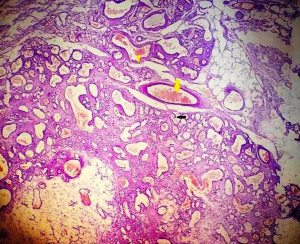
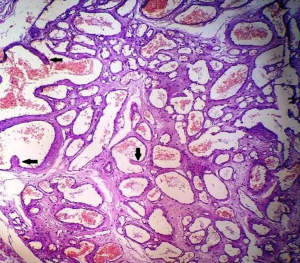
Based on MRI and ultrasonography findings and the increase in the lesion’s size a complete surgical resection of the mass was performed. On gross examination, a firm elastic brownish nodule with sponge-like cut surface was noted measuring 1.1 cm × 0.6 cm × 0.5 cm. Histological examination findings were suggestive of a sinusoidal breast hemangioma. No cellular atypia, necrosis or increased mitotic activity was noted. Histologically, the tumor was characterized by numerous thin-walled cystically dilated interconnecting vessels with monolayered endothelium. Pseudopapillary projections were observed in the channel of some vessels, whereas the stroma among the vessels was relatively scant (Figures 3,4). Surgical margins were tumor free.
The patient had an uncomplicated postoperative course. She is doing well, without any evidence of recurrence 29 months after surgery.
Discussion
Sinusoidal hemangioma was first reported by Calonje and Fletcher in 1991 as a distinctive variant of cavernous hemangioma (10). The authors described 12 cases that predominantly affected females and presented as solitary subcutaneous or deep dermal nodules. Only two of these lesions originated in the breast.
Histologically, breast hemangiomas are characterized by the presence of interconnecting dilated thin-walled vascular channels lined by flat endothelial cells, in the absence of atypia (1,3,10). Depending on the size of the vessels involved breast hemangiomas can be classified into capillary and cavernous types (1,11). Cavernous hemangiomas are the most common subtype (12).
The exact pathogenesis of breast hemangiomas is unknown (13), but estrogens may be implicated in the development (14). The tumor affects most commonly women (2,11) and occurs over a wide age range (18 months to 82 years) (4,11,15). Men are very rarely affected (5).
The most common clinical presentation of a palpable breast hemangioma includes a firm non-tender slow growing nodule (13,16). Discoloration of the overlying skin may be present (14). In most cases the tumor is superficial and rarely is intraparenchymal (5,7).
Breast hemangiomas do not have pathognomonic imaging features (2,5,7,8) and thus imaging studies can be misleading in some cases (2,9,16,17). There are no imaging modalities that can reliably differentiate between vascular benign tumors and angiosarcomas (3,7,14).
At mammography, breast hemangioma may appear as a well-defined, circumscribed or microlobulated mass isodense to the surrounding breast parenchyma (4,11). In some cases, the tumor may be difficult to be seen on craniocaudal or mediolateral oblique views and thus a tangential view may be necessary for evaluation (7). Mammography may have additional limitations, especially in young patients, due to the dense parenchymal pattern (2). The mass may rarely contain microcalcifications (1,3,5,6) of fine, punctuate or phlebolith pattern (3). The presence of microcalcifications on both mammogram and ultrasonography is a factor that may suggest a malignant process (9).
On ultrasonography, breast hemangioma may have a variable appearance. It most commonly appears as a superficially located oval mass with parallel orientation and circumscribed margins. Internal echostructure is variable and the tumor can be hypoechoic, isoechoic or hyperechoic (1,3-5,11). Compressibility of the tumor may be detected only in the absence of thrombosis (7). In some cases an isoechoic tumor cannot be clearly displayed from the surrounding adipose tissue (5). Although the vascularity of the tumor has not been reported to have diagnostic value (2), the presence of hypervascularity may indicate a suspicious of malignancy tumor (7).
There are only a few reports of MRI features of breast hemangioma (9,12,16,18). The tumor appears as an ovoid mass that is isointense to surrounding fibroglandular tissue on T1-weighted images and hyperintense on T2-weighted images (12). Early enhancement following contrast administration may indicate a suspicious lesion (3). However, the MRI findings are variable depending on the possibility of internal thrombosis (1).
Preoperative diagnosis of breast hemangioma is difficult. Only 3 out of 27 patients reviewed by Funamizu et al. (2) had been preoperatively diagnosed. Core needle biopsy and aspiration biopsy cytology have limitations since it has been reported that in up to 40.7% of the patients the obtained specimens were found to contain only hematic material (2). In addition, bleeding may complicate a core biopsy of a vascular breast tumor (1,5,9).
Differential diagnosis of breast hemangioma should include fibroadenoma, hematoma, sebaceous cyst and mucinous carcinoma (7,8). The main differential is however angiosarcoma (4). Angiosaracoma is a very rare clinical entity accounting for 0.004% of all malignant breast tumors and 8% of breast sarcomas (19), and should always be kept in mind when dealing with a vascular breast mass. A high degree of clinical suspicion is required for early diagnosis (17), given that despite its rarity, the breast is one of the more common locations in which angiosarcoma may arise (1,19). Angiosarcomas tend to be of intraparenchymal location and are usually larger than 3 cm (5).
Complete surgical excision is the treatment of choice for breast hemangioma (4,13,17,20). However, in carefully selected cases the surgical intervention can be avoided, when the imaging features are classic and an imaging guided biopsy has been adequately performed, as the latter appears to be sufficiently reliable to exclude a malignant process (11).
In any other case where the imaging and pathologic features are not classic, a complete surgical resection of the tumor is necessary in order to exclude the possibility of an underlying angiosarcoma (1,4,20). In the case presented here, we decided to proceed with a complete surgical resection because of the suspicious MRI findings, the slow but steady increase in the tumors size and the inconclusive aspiration cytology findings.
In conclusion, breast hemangioma is a rare benign vascular tumor that lacks pathognomonic imaging features. In carefully selected cases with classic imaging findings and a definitive diagnosis of breast hemangioma, established by imaging guided core biopsy, conservative management with follow up imaging may be a safe approach. However, in any other case with atypical radiological and pathological findings, a complete surgical resection of the vascular lesion is mandatory in order to exclude the possibility of an underlying angiosarcoma.
Acknowledgements
The author would like to thank Dr. Katikaridis Ilias and Dr. Sambaziotis Dimitrios, from the Department of Pathology for providing the histology slides.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Jesinger RA, Lattin GE Jr, Ballard EA, et al. Vascular abnormalities of the breast: arterial and venous disorders, vascular masses, and mimic lesions with radiologic-pathologic correlation. Radiographics 2011;31:E117-36. [Crossref] [PubMed]
- Funamizu N, Tabei I, Sekine C, et al. Breast hemangioma with difficulty in preoperative diagnosis: a case report. World J Surg Oncol 2014;12:313. [Crossref] [PubMed]
- Adwani A, Bees N, Arnaout A, et al. Hemangioma of the breast: clinical, mammographic, and ultrasound features. Breast J 2006;12:271. [Crossref] [PubMed]
- Lee SJ, Mahoney MC. Benign findings in Breast MRI. In: Molleran VM, Mahoney MC. editors. Breast MRI. Philadelphia: Elsevier Saunders, 2014:62.
- Glazebrook KN, Morton MJ, Reynolds C. Vascular tumors of the breast: mammographic, sonographic, and MRI appearances. AJR Am J Roentgenol 2005;184:331-8. [Crossref] [PubMed]
- Mariscal A, Casas JD, Balliu E, et al. Breast hemangioma mimicking carcinoma. Breast 2002;11:357-8. [Crossref] [PubMed]
- Tilve A, Mallo R, Pérez A, et al. Breast hemangiomas: correlation between imaging and pathologic findings. J Clin Ultrasound 2012;40:512-7. [Crossref] [PubMed]
- Conde DM, de Paula ÉC, Jales RM, et al. A clinically palpable cavernous hemangioma of the breast in an 80-year old woman. Eur J Obstet Gynecol Reprod Biol 2013;167:236-7. [Crossref] [PubMed]
- Kim SJ, Han HS, Kim JS, et al. Cavernous hemangioma of the breast parenchyma with unusual features. J Ultrasound Med 2006;25:1343-6. [Crossref] [PubMed]
- Calonje E, Fletcher CD. Sinusoidal hemangioma. A distinctive benign vascular neoplasm within the group of cavernous hemangiomas. Am J Surg Pathol 1991;15:1130-5. [Crossref] [PubMed]
- Mesurolle B, Sygal V, Lalonde L, et al. Sonographic and mammographic appearances of breast hemangioma. AJR Am J Roentgenol 2008;191:W17-22. [Crossref] [PubMed]
- Kim SM, Kim HH, Shin HJ, et al. Cavernous haemangioma of the breast. Br J Radiol 2006;79:e177-e180. [Crossref] [PubMed]
- Jghaimi F, Baallal H, Fakhri A, et al. Curious vascular tumor. Case Rep Dermatol Med 2012;2012:542594.
- Chung SY, Oh KK. Mammographic and sonographic findings of a breast subcutaneous hemangioma. J Ultrasound Med 2002;21:585-8. [Crossref] [PubMed]
- Hoda SA, Cranor ML, Rosen PP. Hemangiomas of the breast with atypical histological features. Further analysis of histological subtypes confirming their benign character. Am J Surg Pathol 1992;16:553-60. [Crossref] [PubMed]
- Ameen R, Mandalia U, Marr AA, et al. Breast Hemangioma: MR Appearance with Histopathological Correlation. J Clin Imaging Sci 2012;2:53. [Crossref] [PubMed]
- Frey JD, Levine PG, Darvishian F, et al. Angiosarcoma of the breast masquerading as hemangioma: exploring clinical and pathological diagnostic challenges. Arch Plast Surg 2015;42:261-3. [Crossref] [PubMed]
- Hayasaka K, Tanaka Y, Saitoh T, et al. Gadolinium-enhanced dynamic MRI of breast hemangioma. Comput Med Imaging Graph 2003;27:493-5. [Crossref] [PubMed]
- Shin SJ, Lesser M, Rosen PP. Hemangiomas and angiosarcomas of the breast: diagnostic utility of cell cycle markers with emphasis on Ki-67. Arch Pathol Lab Med 2007;131:538-44. [PubMed]
- Rosen PP. Vascular tumors of the breast. V. Nonparenchymal hemangiomas of mammary subcutaneous tissues. Am J Surg Pathol 1985;9:723-9. [Crossref] [PubMed]


