Transoral endoscopic thyroidectomy vestibular approach (TOETVA) for Graves’ disease: a comparison of surgical results with open thyroidectomy
Introduction
Open thyroidectomy (OT) for patients with Graves’ disease, which requires a transverse cervical collar incision, is a safe and standard technique with low morbidity and mortality (1). However, the procedure still leaves a noticeable scar in the anterior region of the neck. Many of the patients with Grave’s disease who require an operation are young women. As such, they are often concerned about postoperative cosmetic appearance (2). Therefore, the need to improve postoperative quality of life, including cosmetics, has increased (3).
Endoscopic neck surgery for parathyroidectomy was first described by Gagner in 1996 (4) and techniques for remote-access thyroid surgery have been developed over the last two decades (5-9). The rapid development of endoscopic techniques and instruments has allowed surgeons to perform a thyroidectomy from a remote site, providing a scar-free outcome in the neck. Recently, natural orifice thyroid surgery has been developed due to its potential for surgery with scar-free results (10-13). The enhanced refinement of this transoral thyroidectomy technique was well-established and described by Anuwong as the transoral endoscopic thyroidectomy vestibular approach (TOETVA) with excellent clinical results (14). This successful experience with TOETVA led the authors of this paper to extend the indications for the procedure to include patients with Graves’ disease, for which there remains little data concerning the use of endoscopic thyroidectomy approaches (15-18).
Methods
A retrospective database of 97 patients who underwent thyroid surgery for Graves’ disease between January 2014 and November 2016 in the Department of Surgery, Police General Hospital was reviewed. All operations were performed by three experienced laparoscopic surgeons. The method for thyroidectomy was either conventional open or TOETVA based on the patients’ preferences. All participants were provided the particular details for their surgeries and informed consent obtained from each patient. The study was approved by the institutional ethics committee of Police General Hospital (No. Dh0818111/59).
Inclusion criteria comprised patients with well-controlled Graves’ disease and at least one out of five indications, including: Grave’s disease with suspicious nodules, toxic multinodular goiter, failure or recurrence after 2 years of anti-thyroid medication, local compressive symptoms, and patients with side effects from anti-thyroid medication.
Exclusion criteria comprised patients who (I) were unfit for surgery; (II) had previously had surgery or radiation of the neck; (III) could not tolerate general anesthesia; or had (IV) thyroid gland diameter larger than 10 cm.
Of the 97 patients in this work, 2 were excluded due to having a thyroid gland size larger than 10 cm from ultrasound (US). There were 49 patients allocated in the OT group and 46 patients in the TOETVA group.
Study protocol
All patients were sent to an endocrinologist for control of the thyroid hormones to euthyroid status before surgery. Lugol’s solution is not routinely used preoperatively. In the OT group, 1 g intravenous cefazolin was injected 30 minutes before the incision. No postoperative antibiotic was given to this group. In the TOETVA group, 1.2 g amoxicillin-clavulanic acid was injected 30 minutes before the incision. Subsequent to operation, intravenous antibiotics were continued for 2 days, after which an oral form was given for 7 days. Patients in both groups started an oral diet on day 1 postoperatively.
Pre- and post-operative vocal cords assessment was performed. Recurrent laryngeal nerve (RLN) injury was defined as postoperative impairment of motility in one or both of the vocal cords. Permanent RLN injury was defined as persistent impairment of vocal cord motility 1 year after surgery; otherwise, it was considered transient.
Serum levels of calcium and parathyroid hormone were measured postoperatively on days 1, 2 and 3. In cases of postoperative hypoparathyroidism, defined as a total serum calcium level lower than 8.0 mg/dL (normal range: 8.0–10.2 mg/dL), patients were supplemented with 1,000–2,000 mg of oral calcium. Hypoparathyroidism was considered permanent in patients who required calcium and vitamin D supplementation for longer than 1 year after surgery.
All patients received follow up at 2 weeks, 3 months, 6 months, and annually. Follow-up tests included clinical examinations for hypoparathyroidism, vocal cord evaluation, and a thyroid function test. In cases where vocal cord injury was noted in a previous follow-up, the vocal cord was re-examined with video-assistance. In cases where hypoparathyroidism was noted in a previous examination, serum levels for calcium, phosphorus, and parathyroid hormone were also measured.
Operative techniques
The TOETVA surgical technique used in this study has been described previously (14). In brief, the patient was in a supine position with neck extended and under general anesthesia with nasotracheal intubation. The surgeon assumed a position standing above the patient’s head, while an assistant stood between both. The oral cavity was disinfected using 0.05% Hibitane in water. A 30-mL solution of 1 mg adrenaline diluted with 500 mL normal saline was injected into the oral vestibular area of the lower lip down to the anterior neck. The first 10 mm incision was made at the center of the oral vestibule, with a subsequent space created passing the mandibular area to the anterior neck using an electric scalpel and Kelly clamp forceps. A blunt-tipped 10-mm trocar was inserted for a 10-mm 30° laparoscope. The CO2 insufflation pressure was set at 6 mmHg. Two 5 mm trocars were inserted at the uppermost and lateral areas near the lower lip on both sides pointing down to the anterior neck. Additionally, a working space was created beneath the platysma. The upper border of the dissecting area was the larynx, while the lower border was the suprasternal notch and the lateral borders were the anterior borders of both sternocleidomastoid muscles. Strap muscles (SMs) were divided by cutting at the midline raphe. For better exposure, SMs were retracted laterally by external hanging sutures. Thyroid isthmus was dissected and transected. An ultrasonic device was used for the dissection and division of tissue and vessels. The middle thyroid vein, superior thyroid artery, and veins were ligated as close to the thyroid as possible. The upper pole of the gland was lifted up with insertion of the RLN at the larynx. Cutting the inferior thyroid artery and vein should be performed close to the gland, with subsequent removal of the rest of Berry’s ligament. All parathyroid glands were identified and preserved. The specimen was removed using an endobag via the 10-mm incision. A surgical drain was placed by adding a 5-mm port into the lateral neck to help the placement of the surgical drain. SMs were closed using absorbable sutures. The oral vestibule surgical wound was closed using absorbable sutures. A pressure dressing was applied around the chin for 24 hours.
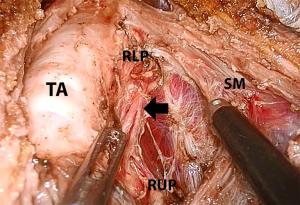
Conventional OT was performed using a 5–6 cm transverse collar incision on the anterior neck. After dissecting an adequate subplatysmal flap, the midline of the SM was divided to expose the thyroid gland. Thyroid vessels were ligated using an ultrasonic device close to the thyroid gland in order to preserve the superior laryngeal nerve and parathyroid glands. The entire cervical course of the ipsilateral RLN, as well as both parathyroid glands were traced and preserved (Figure 1). Total thyroidectomy was performed in both the OT and the TOETVA group.
Outcomes
The data recorded for each patient included the following: age, gender, size of thyroid (cm) by US, operative time (min), duration of hospitalization in days. The primary endpoint was peri and postoperative complications in the two study groups. Perioperative complications such as hematoma, seroma, infection, vocal cord palsy, and hypoparathyroidism were assessed. All patients received follow up based on the same manners as protocol.
Statistical analysis
The independent t-test for continuous variables and Fisher’s exact test were used for the categorical variables. All statistical tests with P value <0.05 were considered statistically significant. Statistical analysis was performed with IBM SPSS software version 20.0 (SPSS, Chicago, IL, USA) for Windows. All values were expressed as mean ± SD for continuous variables and n for categorical variables.
Results
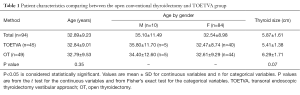
There were 49 OT patients (5 males and 44 females). The mean age was 32.79±9.53 years and the mean of thyroid size was 6.29±1.71 cm. There were 46 patients in the TOETVA group. However, one case had to be converted to open surgery due to excessive bleeding. Thus, 45 patients (5 males and 44 females) were enrolled in the TOETVA group. The mean age in this group was 32.84±9.01 years and the mean size for the thyroid was 5.41±1.38 cm. The characteristics between OT and TOETVA, including the number of patients, their ages, and thyroid size were similar (Table 1).
Full table
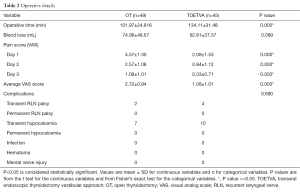
Operative time in the OT group was significantly shorter compared to the TOETVA group (P<<0.05). Blood loss was comparable. The visual analog scale (VAS) pain score was significant lower for the TOETVA group during all 3 days, including the average (P<<0.05) (Table 2).
Full table
In the TOETVA group, postoperative laryngoscopic examination revealed that 4 patients (8.89%) had unilateral vocal cord palsy and hoarseness. In the OT group, RLN palsy was revealed in 2 patients (4.01%). However, it was not significantly different between the two groups. After 3 months, hoarseness improved and the position of the vocal cords returned to normal. Postoperative transient hypocalcemia occurred in 10 patients (22.22%) and 7 patients (14.28%) in TOETVA and OT, respectively. None of the patients in either group was found to have permanent vocal cord palsy, permanent hypocalcemia, infection, hematoma, mental nerve injury or other complications (Table 2).
Discussion
At present, there is little data on the use of endoscopic or robotic thyroidectomy in Graves’ disease patients (15-18), possibly because of hypervascularity and the large size of the thyroid gland in these patients. Moreover, there is no report for use of the transoral thyroidectomy in Graves’ disease patients either. The important strategy in operating on Graves’ disease patients is how to control bleeding during dissection of the thyroid gland, particularly in the enlarged thyroid with high vascularity. Dissection and bleeding control may become difficult due to the relatively small working space and the highly vascular pattern of the gland. This is frequently the reason for conversion to open surgery (15,19). The use of TOETVA has helped to solve this problem because of birds-eye view through the use of magnified stereoscopic visualization and the movement of laparoscopic instruments being superior and improve dexterity and enable more meticulous bleeding control, resulting in a safer surgical procedure (14).
In this study, only one case required conversion to open surgery. That female patient had suffered from Graves’ disease for over 20 years and her thyroid had hypervascularity, big and engorged vessels. The diameter of the superior thyroid artery was 7 mm, which was cut by an ultrasonic device and caused unstoppable bleeding. The maximum diameter for safety of ultrasonic sealing is 5 mm. Therefore, vessels greater than 5 mm should be ligated using a clip before cutting rather than a pure ultrasonic cut to prevent excessive bleeding.
Regarding working space, adequate anterior neck working space was created via the vestibular area of the mouth. The working instrument went directly into the area of dissection, which is required a shorter dissection tunnel than other approaches (18,20). This approach effectively reduces operative time and makes the operation more comfortable. This technique can also be performed bilaterally and possibly extended to central node dissection with the same incision and port placement, which is more convenient and feasible than the axillary approach or other remote-access thyroid surgery techniques with the superior advantage of getting good cosmetic results.
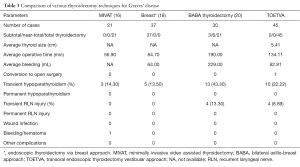
Comparing between TOETVA and OT, the operative time was longer in TOETVA patients than in the OT. This may because of the extra time needed to create the working space or port insertion. Because of the narrow working space, the operation was more difficult. When compared to endoscopic or robotic techniques, TOETVA requires less time than the bilateral axillo-breast approach (BABA), but comparable time to the breast approach (Table 3). Therefore, endoscopic or robot-assisted thyroidectomy usually requires more time than open surgery.
Full table
The incidence of postoperative complications did not differ between the TOETVA and OT groups, which is also comparable to other studies (21-23). Infection is one of the important concerns in oral cavity surgery because TOETVA is defined as a clean-contaminated operation. However, no infective complication in TOETVA has been reported (14). The results in the study remained the same, even with longer operative time. The rate of infection is also comparable to other endoscopic techniques (15-18).
With this approach, dissection was performed in the cranio-caudal direction so the authors could identify RLNs from insertion at the cricothyroid muscle, which is easier when compared with other techniques that identify RLNs from the variable courses. The transient RLN palsy was 4 (8.89%) out of 45 cases and recovery time was 3 months, which was less than the OT groups (13.3%). However, the rates of transient and permanent RLN injury after conventional OT in literature ranged from 2.11% to 11.8% and from 0.2% to 5.9% (24), respectively.
Compared with other techniques, TOETVA has better cosmetic results because the incisions are invisible. However, small scars remain on the anterior region of the neck via video-assisted thyroidectomy (16), on the chest wall and nipples for the breast approach, and on the axilla via bilateral transaxillary approach (25) as well as the BABA (7,26,27). Interestingly, the average pain scores from the first to third operative day were lower in TOETVA patients than in OT patients (2.72±0.94 vs. 1.08±1.01, P<0.05). This data may imply the truly “minimally-invasive thyroidectomy” for patients who undergo thyroidectomy treatment when compared to other endoscopic or robotic thyroidectomy approaches (28).
Although prolonged operative time was observed in TOETVA, no patients had delayed recovery or additional complications compared to OT patients. The authors believe that it is worthwhile spending a longer time to accomplish the operation using this approach for a better cosmetic appearance of the neck and decreased postoperative pain, which improves postoperative quality of life.
Conclusions
TOETVA is a feasible and safe procedure for the surgical treatment of Graves’ disease with excellent clinical and cosmetic outcomes. It is recommended as an alternative option for patients with Graves’ disease who require surgical resection with excellent cosmetic outcomes.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional ethics committee of Police General Hospital (No. Dh0818111/59). All participants were provided the particular details for their surgeries and informed consent obtained from each patient.
References
- Liu ZW, Masterson L, Fish B, et al. Thyroid surgery for Graves' disease and Graves' ophthalmopathy. Cochrane Database Syst Rev 2015.CD010576. [PubMed]
- Dordea M, Aspinall SR. Short and long-term cosmesis of cervical thyroidectomy scars. Ann R Coll Surg Engl 2016;98:11-7. [Crossref] [PubMed]
- Arora A, Swords C, Garas G, et al. The perception of scar cosmesis following thyroid and parathyroid surgery: A prospective cohort study. Int J Surg 2016;25:38-43. [Crossref] [PubMed]
- Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg 1996;83:875. [Crossref] [PubMed]
- Miccoli P, Berti P, Conte M, et al. Minimally invasive surgery for thyroid small nodules: preliminary report. J Endocrinol Invest 1999;22:849-51. [Crossref] [PubMed]
- Ikeda Y, Takami H, Niimi M, et al. Endoscopic thyroidectomy by the axillary approach. Surg Endosc 2001;15:1362-4. [Crossref] [PubMed]
- Choe JH, Kim SW, Chung KW, et al. Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg 2007;31:601-6. [Crossref] [PubMed]
- Wang C, Feng Z, Li J, et al. Endoscopic thyroidectomy via areola approach: summary of 1,250 cases in a single institution. Surg Endosc 2015;29:192-201. [Crossref] [PubMed]
- Park JO, Kim SY, Chun BJ, et al. Endoscope-assisted facelift thyroid surgery: an initial experience using a new endoscopic technique. Surg Endosc 2015;29:1469-75. [Crossref] [PubMed]
- Witzel K, von Rahden BH, Kaminski C, et al. Transoral access for endoscopic thyroid resection. Surg Endosc 2008;22:1871-5. [Crossref] [PubMed]
- Wilhelm T, Metzig A. Endoscopic minimally invasive thyroidectomy (eMIT): a prospective proof-of-concept study in humans. World J Surg 2011;35:543-51. [Crossref] [PubMed]
- Nakajo A, Arima H, Hirata M, et al. Trans-Oral Video-Assisted Neck Surgery (TOVANS). A new transoral technique of endoscopic thyroidectomy with gasless premandible approach. Surg Endosc 2013;27:1105-10. [Crossref] [PubMed]
- Wang C, Zhai H, Liu W, et al. Thyroidectomy: a novel endoscopic oral vestibular approach. Surgery 2014;155:33-8. [Crossref] [PubMed]
- Anuwong A. Transoral Endoscopic Thyroidectomy Vestibular Approach: A Series of the First 60 Human Cases. World J Surg 2016;40:491-7. [Crossref] [PubMed]
- Yamamoto M, Sasaki A, Asahi H, et al. Endoscopic subtotal thyroidectomy for patients with Graves' disease. Surg Today 2001;31:1-4. [Crossref] [PubMed]
- Berti P, Materazzi G, Galleri D, et al. Video-assisted thyroidectomy for Graves' disease: report of a preliminary experience. Surg Endosc 2004;18:1208-10. [Crossref] [PubMed]
- Maeda S, Uga T, Hayashida N, et al. Video-assisted subtotal or near-total thyroidectomy for Graves' disease. Br J Surg 2006;93:61-6. [Crossref] [PubMed]
- Li ZY, Wang P, Wang Y, et al. Endoscopic thyroidectomy via breast approach for patients with Graves' disease. World J Surg 2010;34:2228-32. [Crossref] [PubMed]
- Sasaki A, Nitta H, Otsuka K, et al. Endoscopic subtotal thyroidectomy: the procedure of choice for Graves' disease? World J Surg 2009;33:67-71. [Crossref] [PubMed]
- Kwon H. Bilateral axillo-breast approach robotic thyroidectomy for Graves' disease: an initial experience in a single institute. World J Surg 2013;37:1576-81. [Crossref] [PubMed]
- Cho MJ, Park KS, Cho MJ, et al. A comparative analysis of endoscopic thyroidectomy versus conventional thyroidectomy in clinically lymph node negative thyroid cancer. Ann Surg Treat Res 2015;88:69-76. [Crossref] [PubMed]
- Wang Y, Liu K, Xiong J, et al. Total endoscopic versus conventional open thyroidectomy for papillary thyroid microcarcinoma. J Craniofac Surg 2015;26:464-8. [Crossref] [PubMed]
- Yang CH, Chew KY, Solomkin JS, et al. Surgical site infections among high-risk patients in clean-contaminated head and neck reconstructive surgery: concordance with preoperative oral flora. Ann Plast Surg 2013;71 Suppl 1:S55-60. [PubMed]
- Calò PG, Pisano G, Medas F, et al. Identification alone versus intraoperative neuromonitoring of the recurrent laryngeal nerve during thyroid surgery: experience of 2034 consecutive patients. J Otolaryngol Head Neck Surg 2014;43:16. [Crossref] [PubMed]
- Miyano G, Lobe TE, Wright SK. Bilateral transaxillary endoscopic total thyroidectomy. J Pediatr Surg 2008;43:299-303. [Crossref] [PubMed]
- Lee KE, Choi JY, Youn YK. Bilateral axillo-breast approach robotic thyroidectomy. Surg Laparosc Endosc Percutan Tech 2011;21:230-6. [Crossref] [PubMed]
- Choi JY, Lee KE, Chung KW, et al. Endoscopic thyroidectomy via bilateral axillo-breast approach (BABA): review of 512 cases in a single institute. Surg Endosc 2012;26:948-55. [Crossref] [PubMed]
- Lee MC, Park H, Choi IJ, et al. Comparative study of a gasless transaxillary approach versus a bilateral axillo-breast approach for endoscopic thyroidectomy in a single institute. Head Neck 2014;36:702-8. [Crossref] [PubMed]


