An unusual finding of the auriculotemporal nerve: possible risk factor during preauricular skin incisions
Introduction
The auriculotemporal nerve (ATN) is one of the branches of the mandibular division (V3) of the trigeminal nerve. Clinically, branches of the ATN have been implicated as an etiology of some migraine headaches potentially via compression by the superficial temporal artery (1) and Frey’s syndrome is a known postoperative complication of parotidectomy (2). Although there have been papers describing the anatomy of the ATN (3-5) and it the superficial temporal branches (STb), to our knowledge, none of these has mentioned a duplicated ATN. Herein, we report an extremely rare case of a duplicated ATN and discuss potential clinical implications. The protocol for the present study included no specific tissue requiring approval by our institutional ethics committees, and was performed in accordance with the requirements of the Declaration of Helsinki (64th WMA General Assembly, Fortaleza, Brazil, October 2013).
Case presentation
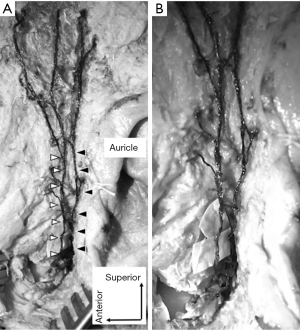
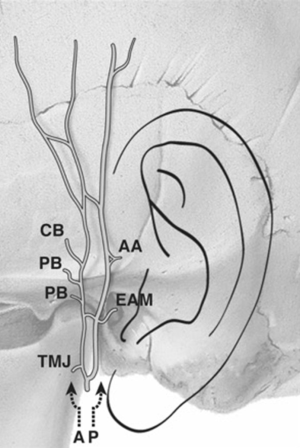
During the dissection of a cadaver that was 87-year-old at death, the left ATN was demonstrated (Figure 1) and found to bifurcate into two main trunks (anterior and posterior). This occurred just behind the base of the condylar process where each main trunk emerged from the superficial layer at approximately 10 mm above the middle of the tragus. The anterior trunk ascended in a similar way as the superficial temporal artery and gave off branches to the temporomandibular joint, parotid gland, external acoustic meatus, temporal region and a communicating branch with the posterior trunk of the ATN (Figure 2). The posterior trunk ascended via the subcutaneous layer 1 mm anterior to the auricle and gave rise to branches to the anterior auricular region, temporal region and a communicating branch with the anterior trunk of the ATN. In addition, two main trunks interconnected anterior to the auricle (Figures 1,2). The diameter of the anterior and posterior trunks was 1.35 and 1.73 mm, respectively. Branches to the zygoma were not observed.
Discussion
The ATN is described as giving rise to branches to the temporomandibular joint, parotid gland, external acoustic meatus, anterior auricle, zygoma and superficial temporal region (1,6). Komarnitki (3,4) classified the branches based on the root system and relationships of the ATN and middle meningeal artery. Kwak (5) and Tansatit (7) noted communicating branches between the ATN and facial nerve. The STb of the ATN has been investigated by Andersen (8) who found that the most superficial part of the STb is located 8 and 20 mm anterior to the root of the helix and is found at a depth of 2–10 mm at the middle part of the tragus. In the present case, the posterior trunk ascended 1 mm anterior to the external ear in the subcutaneous tissues. Andersen (8) also mentioned that on 4 of 19 sides (21%), the ATN had only one main branch and that in 11 cases, the nerve was divided into smaller branches while in another four cases, it had a diffuse branching pattern. However, none of these authors mentioned two main trunks of the ATN that bifurcate in the infratemporal fossa. It is very important anatomical variation for clinical consideration. If the patient whose ATN ascends in a similar way as the posterior trunk of the present case or has two main trunks like our case, a preauricular skin incision might easily injure the ATN. Surgeons should be aware of this variation in order to avoid iatrogenic injury of the ATN.
Acknowledgements
The authors wish to thank all those who donate their bodies and tissues for the advancement of education and research.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Janis JE, Hatef DA, Ducic I, et al. Anatomy of the auriculotemporal nerve: variations in its relationship to the superficial temporal artery and implications for the treatment of migraine headaches. Plast Reconstr Surg 2010;125:1422-8. [Crossref] [PubMed]
- Motz KM, Kim YJ. Auriculotemporal Syndrome (Frey Syndrome). Otolaryngol Clin North Am 2016;49:501-9. [Crossref] [PubMed]
- Komarnitki I, Andrzejczak-Sobocińska A, Tomczyk J, et al. Clinical anatomy of the auriculotemporal nerve in the area of the infratemporal fossa. Folia Morphol (Warsz) 2012;71:187-93. [PubMed]
- Komarnitki I, Tomczyk J, Ciszek B, et al. Proposed classification of auriculotemporal nerve, based on the root system. PLoS One 2015;10:e0123120. [Crossref] [PubMed]
- Kwak HH, Park HD, Youn KH, et al. Branching patterns of the facial nerve and its communication with the auriculotemporal nerve. Surg Radiol Anat 2004;26:494-500. [Crossref] [PubMed]
- Tubbs RS, Shoja MM, Loukas M. Bergman’s Comprehensive Encyclopedia of Human Anatomic Variation. Hoboken, New Jersey: John Wiley & Sons Inc., 2016:999.
- Tansatit T, Apinuntrum P, Phetudom T. Evidence Suggesting that the Buccal and Zygomatic Branches of the Facial Nerve May Contain Parasympathetic Secretomotor Fibers to the Parotid Gland by Means of Communications from the Auriculotemporal Nerve. Aesthetic Plast Surg 2015;39:1010-7. [Crossref] [PubMed]
- Andersen NB, Bovim G, Sjaastad O. The frontotemporal peripheral nerves. Topographic variations of the supraorbital, supratrochlear and auriculotemporal nerves and their possible clinical significance. Surg Radiol Anat 2001;23:97-104. [Crossref] [PubMed]


