
Radiofrequency ablation of an intrathyroidal parathyroid adenoma with intraoperative parathyroid hormone monitoring: a case report of a novel technique
Highlight box
Key findings
• This is the first report of successful treatment of persistent PHPT by RFA with IOPTH monitoring.
What is known and what is new?
• RFA has been used to manage PHPT.
• RFA with IOPTH can be used to manage patients with PHPT.
What is the implication, and what should change now?
• Our work adds to the growing literature suggesting minimally-invasive techniques, such as RFA with IOPTH, as a potential management option for treating parathyroid adenomas.
Introduction
Primary hyperparathyroidism (PHPT) is a common neuroendocrine disorder characterized by elevated serum calcium levels secondary to elevated parathyroid hormone (PTH). PHPT is more prevalent in women and the elderly, affecting almost 1% of all patients aged 69 and older (1). Parathyroidectomy is the mainstay management modality of PHPT, though other minimally-invasive techniques been reported with adequate efficacy considering the disease most often (in 80–85% of cases) arises in consequence of a single adenoma.
Radiofrequency ablation (RFA) is a minimally-invasive approach which delivers well-localized heat by means of a percutaneous catheter for thermal ablation of soft tissue (2). The technique induces thermal injury in the tissue and coagulative necrosis, with applications in the fields of cardiology, vascular surgery, and endocrine surgery. RFA has been demonstrated to effectively and safely treat benign (3), toxic (4), and malignant thyroid nodules (5). Recently, RFA has grown as an attractive alternative to parathyroidectomy, given its impressive safety profile, lack of transcervical incisional scar, and obviation of general anesthesia. The first-ever reported RFA of a parathyroid adenoma in the United States was reported by Hussain et al. in 2021 (6), though a handful of international works, mostly from Asia, have reported their experience with RFA in small cohort studies (20 to 50 patients) (7,8). Interestingly, the use of intraoperative parathyroid hormone (IOPTH) monitoring to confirm cure immediately post-operation during RFA has never been reported.
Persistent PHPT, defined as hypercalcemia within 6 months following parathyroidectomy/intervention, is often secondary to the presence of residual hyperfunctioning parathyroid tissue and occurs in about 1% of cases (9). To our knowledge, we report the first case of successful treatment of a parathyroid adenoma by RFA with IOTPH monitoring in a patient with persistent PHPT. We present this article in accordance with the CARE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-733/rc).
Case presentation
A 51-year-old female with a past medical history of resistant hypertension, hyperlipidemia, vitamin D deficiency, psoriasis, carpal tunnel syndrome, and hysterectomy presented to the endocrine surgery clinic for evaluation of PHPT with complaints of headache, fatigue, and bilateral elbow and leg bone pain. The patient was diagnosed with PHPT consistent with hypercalcemia (11.7 mg/dL), elevated PTH (92 pg/mL), and hypophosphatemia (2.3 mg/dL). Vitamin D levels were normal. 24-hour urine calcium levels were elevated (460 mmoL). The patient was not on calcium or Vitamin D supplements and had no history of nephrolithiasis or gallstones. A bone density scan noted osteoporosis.
Nuclear medicine Sestamibi scan (NM Sestimibi) could not localize a parathyroid adenoma. For financial concerns, the patient refused a neck computerized tomography (CT) scan. A comprehensive neck ultrasound (US) identified a 0.79 centimeter (cm) left central compartment lesion.
Parathyroid exploration led to the excision of the left central compartment lesion related to the upper pole. Following excision, IOPTH dropped from 259.9 to 217.9 pg/mL. Since Miami criterion was not met, which posits that a drop in IOPTH >50% from baseline within 10 minutes confirms procedural cure, neck exploration commenced (10). The left central compartment lesion related to the lower pole was explored but not identified. Right central compartment lesions related to the right upper pole and right inferior pole were identified. Following excision of the larger right superior parathyroid gland, IOPTH dropped to 204.7 pg/mL. Neither extensive neck dissection nor gamma probe scanning could elicit ectopic parathyroid tissue. The surgical pathology noted hypercellular left (60 mg) and normal right upper parathyroid glands. At the time, the lesion discovered on preoperative ultrasound was not suspected to be a parathyroid gland. Three months post operation, the patient’s calcium level was 10.6 mg/dL.
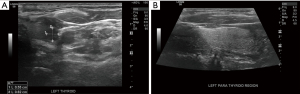
The patient returned one-year post operation with labs as follows: serum calcium 10.9 mg/dL, Vitamin D 37 ng/mL, and PTH 79 pg/mL. The patient was diagnosed with persistent PHPT. Neither a repeat NM Sestamibi scan nor neck 4D CT with contrast could identify a parathyroid adenoma. A neck US localized a suspicious hypoechoic sub-cm left thyroid nodule which measured 0.62 cm × 0.55 cm (Figure 1). Fine needle aspiration of the sub-cm nodule noted a follicular lesion of undetermined significance and PTH-washout revealed an elevated PTH level (2,108 pg/mL), suggestive of an intrathyroidal parathyroid adenoma.
After surgical counseling, the patient refused left thyroid lobectomy, citing concern for post-operative hypothyroidism and the increased risk of complication with redo neck surgery. RFA with IOPTH monitoring was subsequently proposed, to which the patient consented.
Two years following initial parathyroid exploration, the patient underwent IOPTH monitored RFA of the intrathyroidal parathyroid adenoma. Peripheral venous draw determined baseline IOPTH to be 270 pg/mL. US-guided (15-megahertz linear transducer) RFA with a short axis approach proceeded using a 5 mm STARmed probe. The energy level was 15 watts and impedance went up to 300 ohms. Two sessions were conducted in the same operating-room setting. The total ablation time was 3 minutes. Repeat peripheral venous draw ten minutes after final ablation determined IOPTH to be 39.1 pg/mL. The total procedure time lasted 21 minutes. The patient was observed for 30 minutes post-procedure. Post-operative bilateral mobile vocal cords were confirmed via laryngoscope. The patient tolerated the procedure well.
The patient’s only third-day post-operative complaints were of occasional numbness and tingling of her hands and feet. Serum calcium was 9.3 mg/dL. Three months post operation, the patient had normal PTH (49 pg/mL) and calcium (9.5 mg/dL) levels as well as a complete resolution of symptoms. Ultrasound could not detect the adenoma. At 7 months post operation, the patient had no complaints with normal PTH (35 pg/mL) and serum calcium (8.9 mg/dL) levels.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
PHPT is a common endocrine disorder commonly treated by parathyroidectomy. In patients with persistent PHPT following parathyroidectomy/intervention, minimally-invasive techniques such as RFA might be an acceptable and encouraged alternative considering the increased risk of complication in redo surgery. Here, we describe for the first time the successful treatment of persistent PHPT by RFA with IOPTH monitoring.
Parathyroidectomy was first introduced in 1926 by Felix Mandl, and has been the classic method of treating PHPT and persistent hyperparathyroidism. Since then, improved parathyroid imaging studies and intraoperative localization techniques have considerably enhanced the outcomes of modern-day parathyroidectomy. Importantly, the use of IOPTH monitoring has significantly improved success rates of parathyroidectomy, allowing surgeons an intraoperative method of predicting success with >95% accuracy. Patients who achieved a >50% drop from highest baseline IOPTH level at 10 minutes and final IOPTH level within the reference range had a 97% positive predictive value of cure (11). Interestingly however, our literature search of studies utilizing RFA for the treatment of PHPT found no studies which reported the use of IOPTH monitoring (Table 1). Our case demonstrates that the use of IOPTH in minimally-invasive techniques such as RFA is safe and may be encouraged.
Table 1
| Study | Year | Country | Patients (N) | Mean age (years) | Cure rate (%) | Complication |
|---|---|---|---|---|---|---|
| Ebrahiminik et al. (12) | 2022 | Iran | 27 | 63.2 | NR | None |
| *Peng et al. (13) | 2022 | China | 51 | 58.0 | 98.00 | Transient dysphonia [3] |
| *Chai et al. (14) | 2022 | China | 39 | 59.5 | 82.10 | Transient dysphonia [2] |
| *Wei et al. (15) | 2021 | China | 27 | 58.9 | 92.59 | Dysphonia [1] |
| *Wei et al. (7) | 2021 | China | 23 | 59.1 | 87.00 | Dysphonia [1] |
| Li et al. (16) | 2021 | China | 25 | 53.9 | 100.00 | None |
| Ha et al. (8) | 2020 | Korea | 11 | 64.8 | 63.64 | None |
| Korkusuz et al. (17) | 2018 | Germany | 9 | NR | NR | None |
| Sormaz et al. (18) | 2017 | Turkey | 5 | 60.3 | 60.00 | None |
| Xu et al. (19) | 2013 | China | 2 | 52 | NR | Transient dysphonia [1] |
*, Wei et al. 2021 (23 patients) and Wei et al. (27 patients) report on similar patient cohorts. Chai et al. (39 patients) and Peng et al. (51 patients) report on similar patient cohorts. NR, not reported; RFA, radiofrequency ablation.
In comparison to conventional parathyroidectomy, RFA has several advantages (20). Foremost, RFA is typically a short procedure that requires only local anesthetic. Obviating the need for general anesthesia, RFA is an attractive option for elderly patients or those with significant comorbidities. Furthermore, RFA is a scarless procedure. Considering the typical PHPT patient who is female and middle-aged (similar to our patient), a 2–6 cm transcervical permanent scar is an appreciable cosmetic concern for a significant portion of patients (21). In a study of 120 patients who underwent thyroid or parathyroid surgery, Arora et al. found that 75% of the patients would have chosen to have undergone a scarless procedure had they been given the option (22). RFA can also be done as an outpatient procedure and is only minimally discomforting, especially when compared to conventional parathyroidectomy. In addition, unlike parathyroidectomy, RFA can be re-done with minimal to no increase in complication rate. RFA, however, does have important drawbacks. For example, considering the nature of the procedure, patients with parathyroid adenomas which cannot be localized by preoperative ultrasound should not be managed by RFA. In addition, patients who do not experience a drop in IOPTH during RFA are not automatically subject to bilateral neck exploration as in the case of case surgery.
A literature search of non-case report articles which describe the treatment of PHPT by RFA elicited 10 studies (7,8,12-19) (Table 1). All studies were conducted beyond the United States, with 6 works from China. A wide range of cure rates was reported across the studies, ranging from 60% to greater than 90% (15,18). The variability in cure rates could be due to the lack of formally adopted guidelines, which would assist clinicians and surgeons in providing standardized care. The use of IOPTH, as our study demonstrates, may improve this rate as well. Conceivably, the principal concern with the use of RFA for the parathyroid glands are their close proximity to the recurrent laryngeal nerve and the risk of injury due to thermal spread. For this reason, works utilized hydrodissection to mobilize the parathyroid gland to a safer location (6,8,15). Dysphonia was the only complication reported in the studies elicited from our literature search. Consistent with RFA of thyroid nodules, the studies reported consistently low rates of complication. There were no reports of permanent complication. Considering our study specifically, intrathyroidal parathyroid adenomas may be ideal targets for RFA given their location within the thyroid parenchyma which may provide a barrier to thermal spread. Of note, Li et al. reported the treatment of four patients with multiglandular disease. The authors reported that operative failure (defined as both PTH and serum calcium levels within normal limits at 6 months) was more frequent in patients with multiglandular disease (50% cure, N=2/4) as compared to single adenomas (90% cure, N=19/21, P=0.043) (16). Since RFA is a localized treatment and multiglandular disease would suggest multiple ablation attempts, patients with localized PHPT may be more suitable candidates for RFA.
Considering the novelty of parathyroid adenoma management by RFA, future investigations are warranted. For example, persistent or recurrent disease subsequently managed by parathyroidectomy may be more difficult given the potential for increased scar tissue, though this has been shown to be minimal and inconsequential with respect to thyroid nodules (23). In addition, a robust long-term study investigating the risk of long-term recurrence is warranted to better counsel patients.
Conclusions
To our knowledge, this is the first report of successful treatment of persistent PHPT by RFA with IOPTH monitoring. Our work adds to the growing literature suggesting minimally-invasive techniques, such as RFA with IOPTH, as a potential management option for treating parathyroid adenomas.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-733/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-733/coif). EK serves as an Editor-in-Chief of Gland Surgery from May 2017 to April 2024. EK also serves as a consultant of STARmed. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Siilin H, Lundgren E, Mallmin H, et al. Prevalence of primary hyperparathyroidism and impact on bone mineral density in elderly men: MrOs Sweden. World J Surg 2011;35:1266-72. [Crossref] [PubMed]
- Hadedeya D, Attia AS, Shihabi AN, et al. Technique and Procedural Aspects of Radiofrequency Ablation of Thyroid Nodules. Curr Otorhinolaryngol Rep 2021;9:200-6. [Crossref]
- Kandil E, Omar M, Aboueisha M, et al. Efficacy and Safety of Radiofrequency Ablation of Thyroid Nodules: A Multi-institutional Prospective Cohort Study. Ann Surg 2022;276:589-96. [Crossref] [PubMed]
- Kandil E, Omar M, Attia AS, et al. Radiofrequency ablation as a novel modality in the USA for treating toxic thyroid nodules: case series and literature review. Gland Surg 2022;11:1574-83. [Crossref] [PubMed]
- van Dijk SPJ, Coerts HI, Gunput STG, et al. Assessment of Radiofrequency Ablation for Papillary Microcarcinoma of the Thyroid: A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg 2022;148:317-25. [Crossref] [PubMed]
- Hussain I, Ahmad S, Aljammal J. Radiofrequency Ablation of Parathyroid Adenoma: A Novel Treatment Option for Primary Hyperparathyroidism. AACE Clin Case Rep 2021;7:195-9. [Crossref] [PubMed]
- Wei Y, Peng CZ, Wang SR, et al. Effectiveness and Safety of Thermal Ablation in the Treatment of Primary Hyperparathyroidism: A Multicenter Study. J Clin Endocrinol Metab 2021;106:2707-17. [Crossref] [PubMed]
- Ha EJ, Baek JH, Baek SM. Minimally Invasive Treatment for Benign Parathyroid Lesions: Treatment Efficacy and Safety Based on Nodule Characteristics. Korean J Radiol 2020;21:1383-92. [Crossref] [PubMed]
- Schneider DF, Mazeh H, Chen H, Sippel RS. Predictors of recurrence in primary hyperparathyroidism: an analysis of 1386 cases. Ann Surg 2014;259:563-8. [Crossref] [PubMed]
- Irvin GL 3rd, Solorzano CC, Carneiro DM. Quick intraoperative parathyroid hormone assay: surgical adjunct to allow limited parathyroidectomy, improve success rate, and predict outcome. World J Surg 2004;28:1287-92. [Crossref] [PubMed]
- Chiu B, Sturgeon C, Angelos P. Which intraoperative parathyroid hormone assay criterion best predicts operative success? A study of 352 consecutive patients. Arch Surg 2006;141:483-8. [Crossref] [PubMed]
- Ebrahiminik H, Chegeni H, Mosadegh Khah A, et al. Radiofrequency ablation of parathyroid adenomas causing primary hyperparathyroidism: A report of 27 patients. J Clin Ultrasound 2022;50:540-6. [Crossref] [PubMed]
- Peng CZ, Chai HH, Zhang ZX, et al. Radiofrequency ablation for primary hyperparathyroidism and risk factors for postablative eucalcemic parathyroid hormone elevation. Int J Hyperthermia 2022;39:490-6. [Crossref] [PubMed]
- Chai HH, Zhao Y, Zeng Z, et al. Efficacy and Safety of Ultrasound-Guided Radiofrequency Ablation for Primary Hyperparathyroidism: A Prospective Study. Korean J Radiol 2022;23:555-65. [Crossref] [PubMed]
- Wei Y, Peng CZ, Wang SR, et al. Microwave ablation versus radiofrequency ablation for primary hyperparathyroidism: a multicenter retrospective study. Int J Hyperthermia 2021;38:1023-30. [Crossref] [PubMed]
- Li X, Tufano RP, Russell JO, et al. Ultrasound-Guided Radiofrequency Ablation for the Treatment of Primary Hyperparathyroidism: An Efficacy and Safety Study. Endocr Pract 2021;27:1205-11. [Crossref] [PubMed]
- Korkusuz H, Wolf T, Grünwald F. Feasibility of bipolar radiofrequency ablation in patients with parathyroid adenoma: a first evaluation. Int J Hyperthermia 2018;34:639-43. [Crossref] [PubMed]
- Sormaz IC, Poyanlı A, Açar S, et al. The Results of Ultrasonography-Guided Percutaneous Radiofrequency Ablation in Hyperparathyroid Patients in Whom Surgery Is Not Feasible. Cardiovasc Intervent Radiol 2017;40:596-602. [Crossref] [PubMed]
- Xu SY, Wang Y, Xie Q, et al. Percutaneous sonography-guided radiofrequency ablation in the management of parathyroid adenoma. Singapore Med J 2013;54:e137-40. [Crossref] [PubMed]
- Issa PP, Omar M, Issa CP, et al. Radiofrequency Ablation of Indeterminate Thyroid Nodules: The First North American Comparative Analysis. Int J Mol Sci 2022;23:11493. [Crossref] [PubMed]
- Brown BC, McKenna SP, Siddhi K, et al. The hidden cost of skin scars: quality of life after skin scarring. J Plast Reconstr Aesthet Surg 2008;61:1049-58. [Crossref] [PubMed]
- Arora A, Swords C, Garas G, et al. The perception of scar cosmesis following thyroid and parathyroid surgery: A prospective cohort study. Int J Surg 2016;25:38-43. [Crossref] [PubMed]
- Dobrinja C, Bernardi S, Fabris B, et al. Surgical and Pathological Changes after Radiofrequency Ablation of Thyroid Nodules. Int J Endocrinol 2015;2015:576576. [Crossref] [PubMed]


