Cumulative sum analysis of the learning curve for robotic retroauricular thyroidectomy
Highlight box
Key findings
• The current study showed the two different phases of the learning curve using cumulative sum (CUSUM) analysis for robotic retroauricular thyroidectomy. The operation time decreased after a learning curve of approximately 15 cases.
What is known and what is new?
• Robotic retroauricular approach has many advantages in head and neck region compared to other remote approaches due to its versatility.
• Proficiency in docking and manipulating the instruments accelerate the learning curve.
What is the implication, and what should change now?
• Among the various remote approaches, robotic retroauricular approach could be favorable for surgeons to acquire proficient.
• We share experiences of docking and instrument manipulation that can reduce operation time.
Introduction
Since Kocher devised and standardized open cervical incision thyroidectomy in the late 1800s, open thyroidectomy has been recognized as the standard of thyroidectomy (1). However, open thyroidectomy may result in untoward scars, i.e., hypertrophic scars or keloids. Recently, the incidence of thyroid nodules, especially in young women, has increased, and various attempts have been made to minimize the scar attributable to surgery (2).
Various remote access thyroid surgeries, such as transaxillary, breast, axillo-breast, retroauricular, and transoral approaches using endoscopes and robotic systems, have been reported since the introduction of the concept of minimally invasive thyroid surgery (3-5). Among them, robotic facelift (retroauricular) thyroidectomy was first introduced by Terris (6). The retroauricular approach, accessed through an occipital hairline incision and facelift incision, is an anatomically easy approach for head and neck surgeons familiar with parotidectomy (7,8). In addition, compared with the transaxillary approach, the area required for dissection is small and the distance from the incision to the thyroid gland is short (9).
With the introduction of the da Vinci robotic surgical system (Intuitive Surgical Inc., Sunnyvale, CA, USA), sophisticated surgery became possible using a wristed instrument through a three-dimensional surgical field magnified over 10 times (10,11). In general, one rigid binocular stereoendoscope and three rigid instrument arms can be used in robotic surgery. However, using all four robotic arms is challenging in the retroauricular approach owing to the narrow working space (12,13). This is a burden for surgeons performing robotic thyroid surgery using the retroauricular approach; moreover, few reports exist on the learning curve of robotic thyroid surgery with the retroauricular approach.
We started performing robotic retroauricular thyroid surgery in 2018. As we gained experience, we discovered several techniques which enabled using all four robotic arms by adjusting the angle of the arm during the docking process, resulting in easier and more convenient surgical approach.
By using the Cumulative Sum (CUSUM) analysis method that can monitor minute changes in clinical data, we aimed to analyze the learning curve for robotic retroauricular thyroidectomy and share our experience (14). We present the following article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-365/rc).
Methods
Study population
The medical records of 36 patients who underwent robotic retroauricular thyroidectomy between March 2018 and March 2021 were reviewed retrospectively. The clinical features, operation time, duration of hospital stay, and complications according to the period were analyzed. All the procedures, including retroauricular skin incision, robot docking, and robot console manipulation, were performed by a single surgeon (WJJ) using the da Vinci Xi Surgical System robot (Intuitive Surgical, Inc., Sunnyvale, CA, USA).
Before surgery, thyroid nodules and cervical lymph nodes were evaluated using ultrasonography, fine needle aspiration cytology, and computed tomography. The inclusion criteria included benign thyroid nodule with a maximal diameter less than 5 cm and papillary thyroid carcinoma less than 2 cm. The exclusion criteria included patients with papillary thyroid carcinoma with clinically suspected extrathyroidal extension and patients with cervical lymph node metastasis or distant metastases on preoperative imaging.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board of the Seoul National University Bundang Hospital (No. B-2205-756-106). The requirement of informed consent from patients was waived owing to the retrospective nature of the study.
Operative procedure
A retroauricular incision was performed along the occipital hairline, starting from the retroauricular fold. The skin flap was elevated over the fascia of the sternocleidomastoid (SCM) and progressed to the subplatysmal plane. During flap elevation, the great auricular nerve was identified and preserved by leaving it intact on the SCM fascia. Flap elevation was continued until the anterior border of the SCM was identified. The omohyoid muscle was identified, and the strap muscles were dissected from the thyroid gland until the contralateral thyroid lobe was visible. The omohyoid muscle and strap muscles were raised using an external retractor. A 30° dual-channel down viewing scope was used in center arm 3, bipolar fenestrated forceps were used in the non-dominant arms 1 and 2, and a monopolar spatula was used in the dominant arm. The console work was started once the robot arm was entirely docked. The isthmus of the thyroid gland was divided by assessing the midline of the trachea. The upper thyroid pole was dissected from the inferior constrictor muscle, and the superior thyroid vessels were ligated. The superior parathyroid gland was identified and preserved with a magnified surgical view. The thyroid gland was retracted medially to identify the recurrent laryngeal nerve in the tracheoesophageal groove. A space between the thyroid gland and the nerve was secured, and the thyroid gland was carefully dissected. The inferior parathyroid gland was identified and preserved, and the inferior thyroid vessels were ligated. The ligament of Berry was dissected from the trachea, and the thyroid gland was retrieved.
Docking method of the four robotic arms with minimal intraoperative collision
- Placement of the four robotic arms;
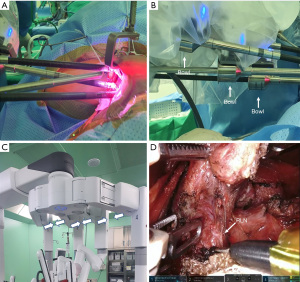
The camera cannula is inserted in the center in a direction parallel to the external retractor, and the cannula is placed upward at the bottom of the incision. A bipolar fenestrated forceps is placed on the left side of the non-dominant side, and a permanent monopolar spatula is placed on the right dominant side, at both the edges of the incision. Another bipolar fenestrated forceps is inserted at the top of the incision parallel to the external retractor. Externally, at the incision site, the camera cannula and the cannula of the two instruments’ robot arms form an inverted triangle, and internally, the tip of each instrument forms a normal triangle (Figure 1A).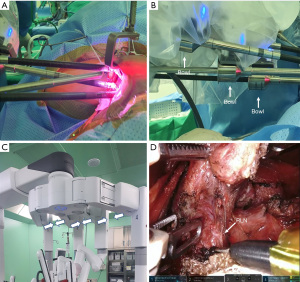 Figure 1 Docking procedure to prevent collisions while using four arms. (A) Internally, the instrument tips form a triangle, and externally, the camera cannula and the cannula of the two instruments’ robot arms form an inverted triangle to minimize collision during the surgical procedure. (B) Alternate the bowls of the cannula forward and backward rather than collinearly. (C) Narrowly spacing flex joint of the patient cart (white arrows). (D) Surgical view. RLN, recurrent laryngeal nerve.
Figure 1 Docking procedure to prevent collisions while using four arms. (A) Internally, the instrument tips form a triangle, and externally, the camera cannula and the cannula of the two instruments’ robot arms form an inverted triangle to minimize collision during the surgical procedure. (B) Alternate the bowls of the cannula forward and backward rather than collinearly. (C) Narrowly spacing flex joint of the patient cart (white arrows). (D) Surgical view. RLN, recurrent laryngeal nerve. - Bowls of cannula;
Bowls, which are the wide parts of the cannula, collide with each other in many cases. Therefore, it is important to alternate the cannulas forward and backward rather than collinearly (Figure 1B). - Narrowly spacing flex joint of the patient cart;
It is easy to speculate that spreading the flex joint of the patient cart is advantageous in preventing collision between the instruments. However, when the flex joint is spread, the instrument arms come closer together. Therefore, it is important to increase the gap between the instrument arms by appropriately narrowing the flex joint (Figure 1C). Securing an appropriate gap between the instrument arms enables to avoid collision of arms during surgery (Figure 1D).
CUSUM analysis and statistical analysis
The CUSUM method was used to analyze the learning curve for robotic retroauricular thyroidectomy. The CUSUM method is used to analyze minute data changes using the difference between the individual data values that change over time and the average value of all the data (15).
Thirty-six cases of robotic thyroid surgery were ordered chronologically according to the date of operation. The operation time in each case was defined as “Xi” and the average operating time as “µ”. The cumulative sum of sequential “n” cases is defined as CUSUMoptime“n”, and CUSUMoptime“n” in each case is defined as follows:
For example, the cumulative sum of the first surgery, “CUSUMoptime_1”, is 27.6 by subtracting the average total operation time of 177.4 minutes from the first patient’s operation time of 205 minutes. “CUSUMoptime_2” is 25.2 by adding −2.4 to 27.6 by subtracting the average operation time of 177.4 minutes from the operation time of the second patient of 175 minutes.
The CUSUM curves were constructed using Microsoft Excel 2010 (Microsoft, Redmond, USA). The slope of the CUSUM curve shows the trend of the learning outcomes, and the inflection point is considered a breakthrough in the learning curve (16). For categorical variables, the differences were analyzed using the Pearson chi-square test or Fisher’s exact test. The continuous variables were analyzed using Student’s t-test. IBM SPSS statistical software (version 19.0; IBM Corp., Armonk, NY, USA) was used for data analysis. All the continuous data are presented as mean ± standard deviation (SD). A P value <0.05 was considered statistically significant.
Results
Robotic retroauricular thyroidectomy was successfully performed in all the patients without conversion to open thyroidectomy. In all 36 patients, ipsilateral lobectomy was performed and no additional neck dissection was performed.
The mean age of the 36 patients who underwent robotic retroauricular thyroidectomy was 40.7±11.4 years (range, 17–61 years). The mean tumor size was 1.3±1.0 cm (range, 0.3–4.5 cm). The CUSUM curve of the operation time shows an ascending slope until the fifteenth case, after which the slope decreases (Figure 2). Therefore, the slope could be divided into two phases. Thus, the first to fifteenth cases were defined as phase I, and the 16th to 36th cases were defined as phase II; various surgical outcomes between the two phases were compared.

Upon comparing the differences in the clinical features between phases I and II, no significant difference in age, sex, postoperative pathology, and nodule size was observed (Table 1). The postoperative pathology of phase II was papillary thyroid cancer in 16 cases, follicular adenoma in three cases, Hürthle cell adenoma in one case, and nodular hyperplasia in one case. Table 2 shows the differences in the surgical outcomes between phases I and II. The total operation time of phase I was 199±41.0 minutes (range, 160–310 minutes) and the total operation time of phase II was 161.9±23.4 minutes (range, 125–215 minutes), which was significantly shorter than that of phase I (P=0.002). The flap elevation and docking time and console time were significantly shorter in phase II than that in phase 1 (P=0.037, P=0.020). The closure time, including hemostasis, drainage placement, and skin suturing after the robot was out, was also shorter in phase II than that in phase I; however, it was not statistically significant (Table 2).
Table 1
| Variable | CUSUM phase | P value | |
|---|---|---|---|
| Phase I (Case 1–15) | Phase II (Case 16–36) | ||
| Sex, female | 14 (93.3) | 19 (90.5) | 1.000 |
| Age, years | 40.4±10.5 | 41.0±12.3 | 0.889 |
| Tumor size, cm | 1.2±1.0 | 1.3±1.0 | 0.687 |
| Pathologic type | 0.062 | ||
| Papillary thyroid carcinoma | 15 (100.0) | 16 (76.2) | |
| Benign | 0 (0.0) | 5 (23.8) | |
Values are presented as mean ± standard deviation or number (%). CUSUM, cumulative sum.
Table 2
| Variable | CUSUM phase | P value | |
|---|---|---|---|
| Phase I (Case 1–15) | Phase II (Case 16–36) | ||
| Total operation time, min | 199.0±41.0 | 161.9±23.4 | 0.002* |
| Flap dissection & docking time, min | 90.0±21.5 | 77.1±14.3 | 0.037* |
| Console time, min | 50.3±17.8 | 36.5±16.2 | 0.020* |
| Closure time, min | 58.6±15.9 | 48.3±15.5 | 0.060 |
| Drain, mL | 79.5±42.1 | 108.6±68.2 | 0.153 |
| Hospital day | 3.1±0.64 | 3.6±1.1 | 0.140 |
| Permanent RLN injury | 0 (0.0) | 0 (0.0) | 1.000 |
| Temporary vocal cord paralysis | 0 (0.0) | 1 (4.8) | 1.000 |
| Neck or auricular paresthesia | 0 (0.0) | 2 (9.5) | 0.500 |
| Hematoma/Seroma | 1 (6.7) | 0 (0.0) | 0.417 |
| Extrathyroidal parathyroids with specimen | 3 (20.0) | 3 (14.3) | 0.677 |
| Completion of intended approach | 15 (100.0) | 21 (100.0) | 1.000 |
Values are presented as mean ± standard deviation or number (%). *, P value <0.05. CUSUM, cumulative sum; RLN, recurrent laryngeal nerve.
There was no significant difference between the two phases in the total amount of drainage, duration of hospital stay, and neck paresthesia after the surgery. Although there was no significant difference, there was one case of hematoma in phase I and one case of temporary vocal cord paralysis in phase II. The parathyroid glands were found in the specimen in three cases each in phases I and II (Table 2).
Discussion
Among the various approaches of robotic thyroid surgery, the retroauricular approach is anatomically familiar to head and neck surgeons. In addition, they are interested in the retroauricular approach since it can be applied to other head and neck surgeries, including salivary gland tumors and neck dissection.
However, few reports exist on the surgical outcomes of the retroauricular approach compared with that of the transaxillary and transaxillo-breast approaches. Most reports are on principled surgical methods. There have been few reports on the learning curves.
We noticed that as the number of cases performed increased, the operating time was shortened, and the operation became easier. We aimed to evaluate the learning curve for robotic retroauricular thyroidectomy using CUSUM analysis and share our experiences.
Currently, robotic surgery is recognized as the standard in visceral surgery in gynecology and urology (17). The advantages of robotics in head and neck surgery include the avoidance of scarring on the face and neck, and the possibility of performing precise surgery in a narrow anatomic region where major vessels and cranial nerves are complexly clustered. In the future, as robot technology develops and the number of cases increases, the use of robots in head and neck surgery will also increase.
A robotic surgical system in thyroidectomy is useful for the identification and preservation of the recurrent laryngeal nerve and parathyroid glands owing to the magnified surgical view and wristed instruments. In particular, if the surgeon becomes proficient in thyroid surgery using the retroauricular approach, a wide range of head and neck surgeries can be performed through the same approach. Therefore, it may be considered advantageous for novice surgeons who desire to begin performing robotic head and neck surgery to begin with the retroauricular approach.
CUSUM analysis is a method developed to monitor industrialization problems and has been previously used to monitor the changes in medical skills and clinical values in other clinical studies (14-16,18). Unlike the moving average line, the CUSUM method accumulates and quantifies the range of fluctuations based on a predetermined threshold value, such as an average, and represents it in the form of a graph (Figure 3). The CUSUM analysis can better reflect the degree of change because the range of variation is accumulated even for small changes between sequentially proceeding event values and a predetermined threshold value.

Studies have been conducted to analyze the learning curve for surgery using the CUSUM analysis, which has such advantages. Park et al. reported that surgeons became competent in performing this procedure after 12 cases of video-assisted mini-laparotomy partial nephrectomy using CUSUM analysis (19). In addition, Gezer et al. reported that surgeons became proficient in video-assisted thoracoscopic lobectomy after 27 cases (20). Using the CUSUM analysis, it is possible to detect subtle trend changes in the operative outcomes, which do not result in much difference; therefore, various variables between distinguished phases can be compared and information concerning the learning curve can be provided.
Several reports exist on the analysis of the learning curve for various approaches of endoscopic or robotic thyroid surgery. Lee et al. reported that in endoscopic hemithyroidectomy, the retroauricular approach had a shorter operative time than that of the transaxillary approach, and the learning curve was stabilized earlier (21). Sun et al. reported that the surgical time significantly decreased after 30–35 cases of robotic thyroidectomy via bilateral axillo-breast approach (22). Park et al. evaluated the learning curve for robotic thyroidectomy using the transaxillary approach of surgeons without experience in endoscopic thyroid surgery. The learning curve was stabilized after 20 cases; thus, the authors suggest that no major obstacle exists in starting robotic surgery even without endoscopic surgery experience (23). Kandil et al. evaluated the learning curve using the CUSUM analysis for robotic thyroid and parathyroid surgery performed by a single surgeon performing various approaches for 10 years using CUSUM analysis (24). Similar to the findings of our study, the retroauricular approach demonstrated that the learning curve was divided based on approximately 20 cases. In contrast, the learning curve was divided based on 69 cases for the transaxillary approach. Kuo et al. performed the CUSUM analysis on the operating time and reported that the transoral endoscopic thyroidectomy vestibular approach (TOEVA) became competent in 35 cases with the accumulation of proficiency (25). As a result of analyzing the learning curve for TOEVA using the CUSUM analysis, Luo et al. also reported that the operation time was stabilized after 40–50 cases (26). Chen et al. reported that in a study comparing TOEVA and transoral robotic thyroidectomy (TORT), a definite learning curve was not observed in the TOEVA group, whereas the learning curve for TORT was 25 cases (27). Although the reported data are heterogeneous, it can be hypothesized that compared with other approaches, the retroauricular approach is advantageous for surgeons in attaining competency.
One rigid binocular stereoscopic endoscope and three robotic arms, a total of four robotic arms, can be used in the da Vinci robotic surgical system. However, unlike the transaxillary approach, docking four robotic arms is challenging using the retroauricular approach owing to the narrow working space. Even if four robot arms are docked via retroauricular incision, if the angle and distance are inappropriate, collisions between the robot arms continuously occur during the surgery, which interfere with the accurate manipulation of the instrument. In the beginning, when the surgeon is inexperienced, these problems are difficult to overcome, and surgery is performed using only three robotic arms. If all four robot arms can be used, traction-counter traction is possible during the surgical procedure, making the dissection much easier, shortening the operation time, and improving safety. A method was devised to insert all four arms through a retroauricular incision with minimal intraoperative collision of instruments. The specific method is described in detail in the materials and methods section (Figure 1). Devising a way to introduce four robotic arms at an appropriate angle and distance between the arms was an important change resulting in shortening of the operation time. This would be helpful for surgeons who are starting out with robotic retroauricular thyroid surgery.
The current study has several limitations. First, since this study was a retrospective observational study, the analysis was performed only on the available data. Second, the study included the analysis of data from a single institution and a single surgeon, and since the surgeon has 10 years of thyroid surgery experience and also has experience with a transaxillary approach, caution is warranted in the interpretation of the learning curve of this study. Third, long-term oncological outcomes were not analyzed in this study. Fourth, in addition to the clinical characteristics presented in this study, it is possible that different anatomical or oncological characteristics of each patient may have influenced the learning curve. Fifth, in this study, only the retroauricular approach was analyzed; therefore, a comparison with other approaches could not be made. Sixth, in this study, the learning curve is analyzed only based on the operation time; hence, it is necessary to analyze the learning curve comprehensively using other parameters in a follow-up study with an increased number of cases. Despite these limitations, few reports exist on the learning curve for robotic retroauricular thyroid surgery compared with that of other approaches. We were able to visualize the initial learning process for robotic retroauricular thyroid surgery using CUSUM analysis and share our experiences with unavoidable challenges through this study. Further studies involving multiple surgeons using multiple approaches are warranted to reach more precise conclusions.
Conclusions
The learning curve of robotic retroauricular thyroidectomy demonstrated a decrease in the operation time after initially performing 15 cases. Docking the robot to minimize collision between the robot arms contributes to reducing the operation time.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-365/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-365/dss
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-365/prf
Conflicts of Interest: All the authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-365/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board of the Seoul National University Bundang Hospital (No. B-2205-756-106). The requirement of informed consent from patients was waived as this was a retrospective study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hegner CF. A History of Thyroid Surgery. Ann Surg 1932;95:481-92. [Crossref] [PubMed]
- Colonna M, Guizard AV, Schvartz C, et al. A time trend analysis of papillary and follicular cancers as a function of tumour size: a study of data from six cancer registries in France (1983-2000). Eur J Cancer 2007;43:891-900. [Crossref] [PubMed]
- Lee KE, Rao J, Youn YK. Endoscopic thyroidectomy with the da Vinci robot system using the bilateral axillary breast approach (BABA) technique: our initial experience. Surg Laparosc Endosc Percutan Tech 2009;19:e71-5. [Crossref] [PubMed]
- Kang SW, Lee SC, Lee SH, et al. Robotic thyroid surgery using a gasless, transaxillary approach and the da Vinci S system: the operative outcomes of 338 consecutive patients. Surgery 2009;146:1048-55. [Crossref] [PubMed]
- Tae K. Complications of Transoral Thyroidectomy: Overview and Update. Clin Exp Otorhinolaryngol 2021;14:169-78. [Crossref] [PubMed]
- Terris DJ, Singer MC, Seybt MW. Robotic facelift thyroidectomy: II. Clinical feasibility and safety. Laryngoscope 2011;121:1636-41. [Crossref] [PubMed]
- Song CM, Jung YH, Sung MW, et al. Endoscopic resection of the submandibular gland via a hairline incision: a new surgical approach. Laryngoscope 2010;120:970-4. [Crossref] [PubMed]
- Grover N, D'Souza A. Facelift approach for parotidectomy: an evolving aesthetic technique. Otolaryngol Head Neck Surg 2013;148:548-56. [Crossref] [PubMed]
- Terris DJ, Singer MC. Qualitative and quantitative differences between 2 robotic thyroidectomy techniques. Otolaryngol Head Neck Surg 2012;147:20-5. [Crossref] [PubMed]
- Choi YS, Hong YT, Yi JW. Initial Experience With Robotic Modified Radical Neck Dissection Using the da Vinci Xi System Through the Bilateral Axillo-Breast Approach. Clin Exp Otorhinolaryngol 2021;14:137-44. [Crossref] [PubMed]
- Song CM, Cho YH, Ji YB, et al. Comparison of a gasless unilateral axillo-breast and axillary approach in robotic thyroidectomy. Surg Endosc 2013;27:3769-75. [Crossref] [PubMed]
- Terris DJ, Singer MC, Seybt MW. Robotic facelift thyroidectomy: patient selection and technical considerations. Surg Laparosc Endosc Percutan Tech 2011;21:237-42. [Crossref] [PubMed]
- Singer MC, Terris DJ. Robotic facelift thyroidectomy. Otolaryngol Clin North Am 2014;47:425-31. [Crossref] [PubMed]
- Steiner SH, Cook RJ, Farewell VT, et al. Monitoring surgical performance using risk-adjusted cumulative sum charts. Biostatistics 2000;1:441-52. [Crossref] [PubMed]
- Bokhari MB, Patel CB, Ramos-Valadez DI, et al. Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc 2011;25:855-60. [Crossref] [PubMed]
- Park EJ, Kim MS, Kim G, et al. Long-term oncologic outcomes of laparoscopic right hemicolectomy during the learning curve period: comparative study with cases after the learning curve period. Surg Laparosc Endosc Percutan Tech 2015;25:52-8. [Crossref] [PubMed]
- Boehm F, Graesslin R, Theodoraki MN, et al. Current Advances in Robotics for Head and Neck Surgery-A Systematic Review. Cancers (Basel) 2021.
- de Leval MR, François K, Bull C, et al. Analysis of a cluster of surgical failures. Application to a series of neonatal arterial switch operations. J Thorac Cardiovasc Surg 1994;107:914-23; discussion 923-4.
- Park JS, Ahn HK, Na J, et al. Cumulative sum analysis of learning curve for video-assisted mini-laparotomy partial nephrectomy in renal cell carcinoma. Medicine (Baltimore) 2019;98:e15367. [Crossref] [PubMed]
- Gezer S, Avcı A, Türktan M. Cusum analysis for learning curve of videothoracoscopic lobectomy. Open Med (Wars) 2016;11:574-7. [Crossref] [PubMed]
- Lee DY, Oh DJ, Kang KR, et al. Comparison of Learning Curves for Retroauricular and Transaxillary Endoscopic Hemithyroidectomy. Ann Surg Oncol 2016;23:4023-8. [Crossref] [PubMed]
- Sun HX, Gao HJ, Ying XY, et al. Robotic thyroidectomy via bilateral axillo-breast approach: Experience and learning curve through initial 220 cases. Asian J Surg 2020;43:482-7. [Crossref] [PubMed]
- Park JH, Lee J, Hakim NA, et al. Robotic thyroidectomy learning curve for beginning surgeons with little or no experience of endoscopic surgery. Head Neck 2015;37:1705-11. [Crossref] [PubMed]
- Kandil E, Akkera M, Shalaby H, et al. A Single Surgeon's 10-Year Experience in Remote-Access Thyroid and Parathyroid Surgery. Am Surg 2021;87:638-44. [Crossref] [PubMed]
- Kuo TC, Duh QY, Wang YC, et al. Practice Patterns and Learning Curve in Transoral Endoscopic Thyroidectomy Vestibular Approach With Neuromonitoring. Front Endocrinol (Lausanne) 2021;12:744359. [Crossref] [PubMed]
- Luo JH, Xiang C, Wang P, et al. The Learning Curve for Transoral Endoscopic Thyroid Surgery: A Single Surgeon's 204 Case Experience. J Laparoendosc Adv Surg Tech A 2020;30:163-9. [Crossref] [PubMed]
- Chen YH, Kim HY, Anuwong A, et al. Transoral robotic thyroidectomy versus transoral endoscopic thyroidectomy: a propensity-score-matched analysis of surgical outcomes. Surg Endosc 2021;35:6179-89. [Crossref] [PubMed]