
Survey of Korean head and neck surgeons and endocrinologists for the surgical extent of 1.5 and 2.5 cm papillary thyroid carcinoma
Introduction
Well-differentiated thyroid cancer has a good prognosis and survival rate. The American Thyroid Association (ATA), British Thyroid Association, National Comprehensive Cancer Network, and Korean Thyroid Association (KTA) have published various guidelines (1-4). Treatment methods for papillary thyroid carcinoma (PTC) have changed over time. According to the 2009 ATA guidelines, total thyroidectomy (TT) was recommended for thyroid cancers >1 cm (1). However, according to the 2015 ATA guidelines, both hemithyroidectomy (Hemi) and TT were possible for thyroid cancer of 1–4 cm (3). The extent of surgery has gradually changed to become less aggressive surgery, which reduces the risk of TT.
According to current ATA guidelines, the “gray zone” refers to the area where both Hemi and TT surgeries are possible in patients with 1–4 cm PTC. The surgical extent in 1–4 cm PTC is determined by tumor factors [location of tumor, degree of extrathyroidal extension (ETE), multifocality, lymph node metastasis, and status of opposite lobe, etc.], patient factors (systemic morbidity, radiation history, and family history, etc.), and surgeon factors (experience and preference). The extent of thyroidectomy and the usefulness of prophylactic central neck dissection (pCND) in patients with 1–4 cm PTC is debatable. Patients, endocrinologists, and surgeons who participated in discussions regarding the benefits and risks of surgery recommended a multidisciplinary decision (5). However, surgeons and endocrinologists can suggest different surgical methods for patients with 1–4 cm PTC. In addition, different surgical extents may be recommended according to the surgeon’s or endocrinologist’s experience. Consequently, patients are sometimes confused about the appropriate surgical methods. Communication amongst surgeons or between surgeons and endocrinologists may also be impaired.
We investigated the current management trends performed by Korean head and neck surgeons and endocrinologists to optimize the surgical extent for 1–4 cm PTC. PTC, with a size of 1–4 cm, has a wide range of surgical extent selection. Therefore, this survey was intended to help determine the preference in the extent of thyroidectomy and pCND by analyzing the surgical methods according to the condition of tumor. We present the following article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-326/rc).
Methods
The author developed a questionnaire using ‘Google Forms’, a web-based survey management software. The questionnaire was sent to 342 Korean Society of Head and Neck Surgery and 160 one branch of Korean Endocrine Society members from June to July 2021 by e-mail. To avoid duplication of responses, each name was registered in the questionnaire. After data collection was completed, the name was changed to unique ID and anonymized.
To evaluate surgeons and endocrinologists preference for surgical extent of thyroidectomy in patients with PTC, each scenario was of 55-year-old female diagnosed with a solitary, node-negative PTC with no history of radiation to head and neck, no family history and medication. Respondents were asked which treatment they would choose depending on factors such as tumor size, degree of ETE, and tumor location. Response options included Hemi, Hemi with pCND, TT and TT with pCND.
The detailed consists of each scenario are as follows. The surgical extent of 1–4 cm PTC is controversial. There are the reports of significant differences in ETE, recurrence, and survival according to tumor size in patients with >2 cm compared to <2 cm among 1–4 cm PTC (6,7). Therefore, in order to evaluate the preference according to the tumor size, 1.5 cm was set for less than 2 and 2.5 cm was set for greater than 2 cm. It is difficult to accurately identify minimal or gross ETE on preoperative ultrasonography (US). Also, preoperative US findings suspecting minimal or gross ETE may differ from doctor to doctor. So, in this study, the minimum ETE or gross ETE was set as the case where ETE was suspected when the respondent evaluated it on US. In addition, various nodules conditions were set in the contralateral lobe to determine the surgical extent according to the condition of the contralateral lobe.
We compared the proportion of respondents’ preference for each scenario. In addition, in order to compare the differences in preferences according to experience, surgeons were classified into high- and low- volume, and endocrinologists were classified into high- and low- experience.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was reviewed by the Institutional Review Board (IRB) of Pusan National University Hospital and determined to be exempt (IRB No. 2209-034-119) and informed consent was taken from the members participating in the survey.
Statistical analysis
Statistical analyses were performed using SPSS software, version 22 (Chicago, IL, USA). Chi-squared and Fisher’s exact tests were used to analyze the relationship between the proportion of responders and the extent of surgery. They all reported two-sided P values.
Results
Demographic findings of respondents
Fifty-seven of 342 surgeons (16.7%) and twenty-seven of 160 (16.9%) endocrinologists responded to the questionnaire. Both surgeon and endocrinologist respondents mainly worked in tertiary hospitals (77% and 51.9%, respectively) (Table 1). The proportion of surgeons with more than 10 years of experience in thyroid surgery was 65%. The proportion of surgeons who performed thyroid surgery in >500 cases was 58%. The proportion of endocrinologists who had majored in endocrinology for >10 years was 48.1%. In endocrinologists, the proportion of thyroid patients among outpatients was 25–50% in many cases.
Table 1
| Respondents | Surgeon, n (%) | Endocrinologist, n (%) |
|---|---|---|
| Age (years) | ||
| <40 | 7 (12.0) | 7 (25.9) |
| 40–49 | 34 (60.0) | 13 (48.1) |
| 50–59 | 11 (19.0) | 5 (18.5) |
| ≥60 | 5 (9.0) | 2 (7.4) |
| Place of work | ||
| Tertiary hospital | 44 (77.0) | 14 (51.9) |
| General hospital | 9 (16.0) | 8 (29.6) |
| Clinic | 4 (7.0) | 5 (18.5) |
| Experience of surgeon or endocrinologist (years) | ||
| <5 | 6 (10.0) | 5 (18.5) |
| 5–10 | 14 (25.0) | 9 (33.3) |
| 10–20 | 26 (46.0) | 8 (29.6) |
| ≥20 | 11 (19.0) | 5 (18.5) |
| Number of cases of thyroidectomy | ||
| <100 | 8 (14.0) | – |
| 100–500 | 16 (28.0) | – |
| 500–1,000 | 14 (25.0) | – |
| 1,000–3,000 | 12 (21.0) | – |
| ≥3,000 | 7 (12.0) | – |
| Outpatient proportion of thyroid patients | ||
| <10% | – | 2 (7.4) |
| 11–25% | – | 4 (14.8) |
| 25–50% | – | 14 (51.9) |
| 50–75% | – | 7 (25.9) |
| ≥75% | – | 0 (0.0) |
Surgical methods for 1.5 or 2.5 cm PTC isolation on US
We asked surgeons and endocrinologists regarding the appropriate surgical method for 1.5 or 2.5 cm PTC, in which lymph node metastasis and ETE were not observed on US. Regardless of the size, the preferred extent of thyroidectomy for surgeons and endocrinologists was Hemi with pCND. Although there was a tendency to prefer Hemi at 1.5 and 2.5 cm, the tendency to prefer Hemi at 2.5 cm PTC decreased significantly with both surgeons and endocrinologists (Table 2) (P<0.05). There was no difference in preference for Hemi based on size between surgeons and endocrinologists. pCND was recommended in more than 50% of 1.5 or 2.5 cm PTCs without ETE. The preference for pCND showed no significant difference between surgeons and endocrinologists based on size (Table 3).
Table 2
| Factors of tumor | Surgeon (N=57), n (%) | Endocrinologist (N=27), n (%) | Surgeon vs. endocrinologist (P value) |
|---|---|---|---|
| Isolation | |||
| 1.5 cm | 55 (96.0) | 26 (96.3) | NS |
| 2.5 cm | 38 (66.0) | 20 (74.1) | NS |
| 1.5 vs. 2.5 cm (P value) | 0.000 | 0.050 | |
| Suspected ant. minimal ETE | |||
| 1.5 cm | 49 (85.0) | 17 (63.0) | 0.023 |
| 2.5 cm | 31 (54.0) | 8 (29.6) | 0.038 |
| 1.5 vs. 2.5 cm (P value) | 0.000 | 0.014 | |
| Suspected ant. gross ETE | |||
| 1.5 cm | 21 (37.0) | 4 (14.8) | 0.044 |
| 2.5 cm | 14 (25.0) | 1 (3.6) | 0.000 |
| 1.5 vs. 2.5 cm (P value) | NS | NS | |
| Suspected post. gross ETE | |||
| 1.5 cm | 12 (24.0) | 3 (11.1) | NS |
| 2.5 cm | 7 (13.0) | 2 (7.4) | NS |
| 1.5 vs. 2.5 cm (P value) | NS | NS | |
| Isthmus, 1.5 cm | 47 (82.0) | 12 (44.5) | 0.000 |
NS, no specific; ant., anterior; ETE, extrathyroidal extension; post., posterior.
Table 3
| Factors of tumor | Surgeon (N=57), n (%) | Endocrinologist (N=27), n (%) | Surgeon vs. endocrinologist (P value) |
|---|---|---|---|
| Isolation | |||
| 1.5 cm | 35 (61.4) | 14 (51.9) | NS |
| 2.5 cm | 36 (63.2) | 20 (74.1) | NS |
| 1.5 vs. 2.5 cm (P value) | NS | NS | |
| Suspected ant. minimal ETE | |||
| 1.5 cm | 41 (71.9) | 26 (96.3) | 0.009 |
| 2.5 cm | 43 (75.4) | 26 (96.3) | NS |
| 1.5 vs. 2.5 cm (P value) | NS | NS | |
| Suspected ant. gross ETE | |||
| 1.5 cm | 48 (84.2) | 26 (96.3) | NS |
| 2.5 cm | 51 (89.5) | 26 (96.3) | NS |
| 1.5 vs. 2.5 cm (P value) | NS | NS | |
| Suspected post. gross ETE | |||
| 1.5 cm | 52 (91.2) | 27 (100.0) | NS |
| 2.5 cm | 54 (94.7) | 27 (100.0) | NS |
| 1.5 vs. 2.5 cm (P value) | NS | NS | |
| Isthmus, 1.5 cm | 37 (64.9) | 22 (81.5) | NS |
NS, no specific; ant., anterior; ETE, extrathyroidal extension; post., posterior.
Surgical methods for 1.5 or 2.5 cm PTC suspected of anterior minimal ETE on US
We asked surgeons and endocrinologists regarding the appropriate surgical method for 1.5 or 2.5 cm PTC with suspected anterior minimal ETE and no lymph node metastasis on US. Both surgeons and the endocrinologists preferred Hemi with pCND at a 1.5 cm PTC. However, for the 2.5 cm PTC, TT with pCND was preferred in both groups. Compared to the 1.5 cm PTC suspected of anterior minimal ETE, the ratio of Hemi in 2.5 cm PTC was significantly decreased in both endocrinologists and surgeons (Table 2) (P<0.05). In addition, in 1.5 or 2.5 cm PTC suspected of anterior minimal ETE, surgeons had a significantly higher hemi rate than endocrinologists (Table 2) (P<0.05). The ratio of pCND did not differ between the 1.5 and 2.5 cm PTC. However, in the case of a 1.5 cm PTC suspected of anterior minimal ETE, the preference for performing pCND by an endocrinologist rather than by a surgeon was significantly higher (Table 3) (P<0.05).
Surgical methods for 1.5 or 2.5 cm PTC suspected of anterior gross ETE on US
We asked surgeons and endocrinologists regarding the appropriate surgical method for 1.5 or 2.5 cm thyroid papillary cancer with suspected anterior gross ETE and no lymph node metastasis on US. There was no difference between 1.5 and 2.5 cm PTC in the ratio of Hemi preference. Regardless of the size, both surgeons and endocrinologists preferred TT with pCND. However, in 1.5 or 2.5 cm PTC suspected of anterior gross ETE, the rate of preference for Hemi was significantly lower in endocrinologists than in surgeons (Table 2) (P<0.05). This means that when anterior gross ETE is suspected, endocrinologists prefer TT compared with surgeons’ preference, regardless of size. Moreover, pCND was often preferred regardless of size, and there was no difference between surgeons and endocrinologists (Table 3).
Surgical methods for 1.5 or 2.5 cm PTC suspected of posterior gross ETE on US
We asked surgeons and endocrinologists regarding the appropriate surgical method for 1.5 or 2.5 cm PTC with suspected posterior gross ETE and no lymph node metastasis in US. Regardless of size, both surgeons and endocrinologists preferred TT with pCND, and there was no difference in the extent preferred between the two groups (Table 2). There was no significant difference in the rate of pCND, either in size or between the two groups (Table 3).
Surgical extent for 1.5 cm PTC located isthmus on US
We asked surgeons and endocrinologists regarding the appropriate surgical method for a 1.5 cm PTC located at the isthmus without ETE or lymph node metastasis on US. Surgeons preferred Hemi with CND in 56% of cases. Hemi was preferred in 82% of cases by surgeons and in 44.5% of cases by endocrinologists (Table 2). The percentage of surgeons who preferred Hemi was significantly higher than that of endocrinologists (P<0.05). The rate of pCND was higher in the endocrinologist group, but there was no significant difference in the pCND between the two groups (Table 3).
Status of the contralateral lobe changing from Hemi to TT
Surgeons performed TT in more than 50% of cases where the contralateral lesion was taller than wide hypoechoic nodules (<5 mm), single benign thyroid nodules >3 cm, or multiple benign nodules (largest <3 cm) (Table 4). When the contralateral lesion is taller than wide hypoechoic nodules (<5 mm), hypoechoic nodules (5–10 mm), single benign thyroid nodules >3 cm, or multiple benign nodules (largest <3 cm), endocrinologists recommend TT in more than 50% of cases. There was no significant difference between the two groups (Table 4).
Table 4
| Contralateral lobe | Surgeon (N=39), n (%) | Endocrinologist (N=23), n (%) | Surgeon vs. endocrinologist (P value) |
|---|---|---|---|
| Taller than wide hypoechoic nodule (<5 mm, no cytology performed) | 21 (55.3) | 16 (69.6) | NS |
| 0.5–10 mm hypoechoic nodule (non-diagnosis in cytology) | 17 (44.7) | 13 (56.5) | NS |
| Single benign nodule, <1 cm | 2 (5.3) | 0 (0.0) | NS |
| Multiple benign nodules, largest <1 cm | 6 (15.8) | 1 (4.3) | NS |
| Single benign nodule, 1–2 cm | 7 (18.4) | 2 (8.7) | NS |
| Multiple benign nodules, largest <2 cm | 17 (44.8) | 8 (34.8) | NS |
| Single benign nodule, 2–3 cm | 13 (34.2) | 6 (26.1) | NS |
| Multiple benign nodules, largest <3 cm | 20 (62.6) | 12 (52.2) | NS |
| Single benign nodule, >3 cm | 26 (68.4) | 17 (73.9) | NS |
Hemi, hemithyroidectomy; TT, total thyroidectomy; NS, no specific.
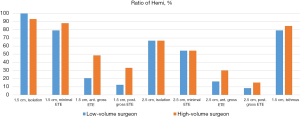
Proportion of Hemi between low- and high-volume surgeons
To evaluate the differences by surgeon volume, respondents were categorized as low-volume if they performed 500 or fewer thyroidectomies, and high-volume if they performed greater than 500 thyroidectomies. The preference between high-volume and low-volume surgeons showed no difference in all scenarios. In PTC with anterior gross ETE, the proportion of hemi in the high volume surgeon was 48.5%, which was higher than that of the low volume surgeon (20.8%), but there was no statistical significance (P>0.05) (Figure 1).
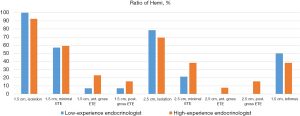
Proportion of Hemi between low- and high-experience endocrinologists
To evaluate the differences by endocrinologists’ experience, respondents were categorized as low-experience if they worked for 10 years or less, and high-experience if they worked for more than 10 years. The preference for Hemi did not differ between high-experience and low-experience endocrinologists in all scenarios (Figure 2).
Discussion
The 2009 ATA guidelines recommend TT as an appropriate surgery for patients with PTC >1 cm (1). However, in a study that adjusted for risk factors (patient comorbidities, tumor multifocality, ETE, nodal disease, distant metastases, and completeness of resection) for thyroid cancer, the surgical extent had no effect on patient survival in 1–4 cm PTC (8). Therefore, in the 2015 ATA guidelines, both Hemi and TT are possible for 1–4 cm PTC (3). In a meta-analysis of 1–4 cm PTC, the oncological outcomes of Hemi and TT were comparable (9). However, in another meta-analysis of 1–4 cm PTC, Hemi was associated with a higher mortality in 2.0 to 4.0 cm PTC patients (10). The surgical extent of 1–4 cm PTC is still controversial. Several survey studies support this by showing slightly different trends from guidelines for thyroid surgery (11-13). Because of this, real clinical practice may differ from guidelines and this may confuse the patients.
In this survey, surgeons and endocrinologists had a high rate of Hemi preference in 1.5 and 2.5 cm PTC without ETE. However, the rate of Hemi at 2.5 cm compared to 1.5 cm without ETE was significantly decreased. Endocrinologists also frequently recommend Hemi for 1.5 and 2.5 cm PTC suspected isolation. For both surgeons and endocrinologists, the Hemi ratio decreased with increasing size. It was found that the 1–4 cm PTC do not belong to a single group, and different surgical methods are applied in real clinical practice based on the size. Several studies have shown that aggressive therapy is needed because the prognosis is poor when the tumor is greater than 2 cm (6,7,14). For this reason, it is considered that the ratio of TT at 2.5 cm is higher than 1.5 cm.
ETE is an important risk factor. ETE can be divided into minimal (microscopic) and gross (massive). Compared to the situation in the past, the importance of minimal ETE as a prognostic factor has been greatly reduced, and gross ETE is known to be an important risk factor (15,16). In this survey, surgeons had a high rate of Hemi in 1.5 and 2.5 cm PTC with suspected anterior minimal ETE. However, the rate of Hemi at 2.5 cm compared with that at 1.5 cm under the same conditions also significantly decreased. Endocrinologists also frequently recommend Hemi for 1.5 cm PTC with suspected anterior minimal ETE. However, the rate of Hemi recommended by the endocrinologists at 2.5 cm, where anterior minimal ETE is suspected, was lower than that by the surgeons. In 1.5 and 2.5 cm PTC with anterior minimal ETE, Korean endocrinologists preferred more aggressive surgery than the Korean head and neck surgeons.
Suspected anterior gross ETE indicated that anterior strap muscle invasion was suspected on US. Gross strap muscle invasion (T3b) is associated with a higher risk of positive resection margins, larger tumor size, higher recurrence rate, and lower disease survival rate (17-19). Therefore, when anterior gross ETE is suspected, both surgeons and endocrinologists recommend TT in many cases. However, the rate of recommending Hemi in the surgeon group was significantly higher than that in the endocrinologist group at 1.5 and 2.5 cm PTC with suspected anterior gross ETE. It is thought that some surgeons have confidence in the surgical margin because invasion of the strap muscle can be surgically removed. This is related to a recent report by Yoon et al. that gross ETE invading the strap muscle is not related to disease-specific survival (20). However, the rate of TT was high in both surgeons and endocrinologists at 1.5 and 2.5 cm PTC with posterior gross ETE. There was no difference in the rate of TT recommendations between the two groups. It is thought that TT is preferred in case of posterior gross ETE because the tumor could be easily invaded the nerve, esophagus, and trachea (21).
Isthmus PTC may be more likely to invade adjacent organs and strap muscles due to their anatomical location. Although some meta-analyses have shown that PTC occurring in the isthmus has a higher chance of multiple foci, invasion of the thyroid capsule, central metastasis, and recurrence compared with PTC occurring in other sites, the appropriate surgical extent (TT vs. less than TT) in isthmus PTC remains controversial (22,23). In this survey, surgeons preferred Hemi and endocrinologists preferred TT for a 1.5 cm PTC located in the isthmus. Korean endocrinologists prefer more aggressive surgery than surgeons for PTC located in the isthmus.
The usefulness of pCND remains controversial. It reduces the risk of locoregional recurrence; however, it increases the risk of postoperative complications, such as hypocalcemia or vocal palsy (24,25). According to the 2015 ATA guidelines, pCND should be considered in patients with advanced primary tumors (T3 or T4), or clinically involved lateral neck nodes (cN1b), or if the information will be used to plan further steps in therapy (3). Although pCND in low-risk PTC is not recommended by the ATA guidelines, in this study, pCND was preferred in more than 50% of isolated PTC group without ETE. These results are similar to the previous survey on the treatment method of the Korean head neck surgeons for microPTC (12), Korean head and neck surgeons and endocrinologists prefer pCND because they tend to think that removing the central lymph node with a high occult metastasis rate reduces the recurrence (26,27), and that unilateral CND has less effect on postoperative hypoparathyroidism or nerve injury.
Surgical extent of thyroidectomy can be affected by the surgeon’s or endocrinologist’s experience. In a survey of surgeons conducted in the United States, high-volume surgeons recommended lobectomy more frequently than low-volume surgeons for 1–3 cm PTC (13). However, in the survey on the preference of the surgical treatment of microPTC, there was no significant difference in most scenarios between the high- and low-volume surgeons (28). In this study, there was no significant difference in surgical extent according to experience as shown in Figures 1,2. Therefore, it will be necessary to conduct further research on the effect of endocrinologists and surgeons experience on the surgical extent.
The preferences of endocrinologists and surgeons for surgical extents vary slightly depending on the survey. In Turkey’s study comparing endocrinologists and surgeons preference for microPTC, endocrinologists also showed that the ratio of TT and pCND was higher than that of surgeons (29). However, in a survey conducted on low-risk PTC in the United States, in many scenarios, surgeons and endocrinologists recommended similar surgical extent, but in some scenarios, surgeons preferred more aggressive treatment than endocrinologists (30). In this survey, in the case of anterior minimal ETE, anterior gross ETE, and tumor in isthmus, endocrinologists preferred more aggressive treatment than surgeons (P<0.05). Therefore, it is thought that the preferences of endocrinologists and surgeons for thyroid surgery vary from country to country.
Various factors influence the surgical extent of thyroidectomy. In this study, it was confirmed that even with the same tumor and patient factor, different surgical methods were recommended according to surgeons and endocrinologists. If endocrinologists and surgeons recommend different surgical methods in the same patient, it may confuse the patient and lead to distrust of the doctor. Therefore, it is desirable to discuss in depth the risks and benefits of surgery through the multidisciplinary decision in which endocrinologists, surgeons, and patients participate before surgery.
This survey compared the surgical extent preferred between surgeons and endocrinologists according to PTC size, degree of ETE, and tumor location in 1.5 and 2.5 cm PTC. This study has limitations. First, the low response rates of surgeons and endocrinologists to the survey may have affected the results (57/342, 27/160, respectively). However, in Korea, 342 head and neck surgeons include retired professors or private clinic members who do not perform thyroid surgery. Currently, there are about 150 active head and neck surgeons in Korea, and it is estimated that about 50% of them are surgeons performing thyroid surgery. Therefore, it is thought that most Korean head and neck surgeons who perform thyroid surgery responded in this survey. Second, a nationwide survey was conducted on head and neck surgeons, but there is a limitation in that it was conducted locally only for endocrinologists. The total population of the local branch is about 8 million, with 160 endocrinologists working. Among them, only 27 endocrinologists answered, but most of them are treating thyroid disease. The response rate of endocrinologists was low, but the trend of treatment recommendations for 1–4 cm PTC could be identified through this survey. Although it cannot represent all current trends in Korea, the results of this study are thought to be helpful in comparing the preference between endocrinologists and surgeons.
Conclusions
TT was frequently preferred in tumors with a large size or gross ETE, and pCND was frequently preferred in cases of suspected gross ETE. This study shows as the extent of thyroid surgery may differ between endocrinologists and surgeons and this could be confusing to patient and affect the patient outcomes. Therefore, individualized multidisciplinary approach considering the extent of surgery for thyroid cancer is recommended.
Acknowledgments
We are grateful to the members of the Korean Society of Head and Neck Surgery and the Korean Endocrine Society who participated in this survey. And we would like to thank Editage (https://www.editage.co.kr/) for English language editing.
Funding: This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) [NRF-2022R1A2C2006697].
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-326/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-326/dss
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-326/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-326/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was reviewed by the Institutional Review Board (IRB) of Pusan National University Hospital and determined to be exempt (IRB No. 2209-034-119) and informed consent was taken from the members participating in the survey.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009;19:1167-214. [Crossref] [PubMed]
- Yi KH, Lee EK, Kang HC, et al. 2016 Revised Korean Thyroid Association Management Guidelines for Patients with Thyroid Nodules and Thyroid Cancer. Int J Thyroidol 2016;9:59-126. [Crossref]
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;26:1-133. [Crossref] [PubMed]
- Perros P, Boelaert K, Colley S, et al. Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf) 2014;81:1-122. [Crossref] [PubMed]
- Agrawal N, Evasovich MR, Kandil E, et al. Indications and extent of central neck dissection for papillary thyroid cancer: An American Head and Neck Society Consensus Statement. Head Neck 2017;39:1269-79. [Crossref] [PubMed]
- Shin CH, Roh JL, Song DE, et al. Prognostic value of tumor size and minimal extrathyroidal extension in papillary thyroid carcinoma. Am J Surg 2020;220:925-31. [Crossref] [PubMed]
- Kim JW, Roh JL, Gong G, et al. Recurrence in patients with clinically early-stage papillary thyroid carcinoma according to tumor size and surgical extent. Am J Surg 2016;212:419-425.e1. [Crossref] [PubMed]
- Adam MA, Pura J, Gu L, et al. Extent of surgery for papillary thyroid cancer is not associated with survival: an analysis of 61,775 patients. Ann Surg 2014;260:601-5; discussion 605-7. [Crossref] [PubMed]
- Gartland RM, Lubitz CC. Impact of Extent of Surgery on Tumor Recurrence and Survival for Papillary Thyroid Cancer Patients. Ann Surg Oncol 2018;25:2520-5. [Crossref] [PubMed]
- Zhang C, Li Y, Li J, et al. Total thyroidectomy versus lobectomy for papillary thyroid cancer: A systematic review and meta-analysis. Medicine (Baltimore) 2020;99:e19073. [Crossref] [PubMed]
- Lee YS, Nam KH, Chung WY, et al. Practical management of well differentiated thyroid carcinoma in Korea. Endocr J 2008;55:1015-24. [Crossref] [PubMed]
- Lee YS, Lee BJ, Hong HJ, et al. Current trends of practical issues concerning micropapillary thyroid carcinoma: The Korean Society of Thyroid-Head and Neck Surgery. Medicine (Baltimore) 2017;96:e8596. [Crossref] [PubMed]
- McDow AD, Saucke MC, Marka NA, et al. Thyroid Lobectomy for Low-Risk Papillary Thyroid Cancer: A National Survey of Low- and High-Volume Surgeons. Ann Surg Oncol 2021;28:3568-75. [Crossref] [PubMed]
- Cheng SP, Chien MN, Wang TY, et al. Reconsideration of tumor size threshold for total thyroidectomy in differentiated thyroid cancer. Surgery 2018;164:504-10. [Crossref] [PubMed]
- Woo CG, Sung CO, Choi YM, et al. Clinicopathological Significance of Minimal Extrathyroid Extension in Solitary Papillary Thyroid Carcinomas. Ann Surg Oncol 2015;22:S728-33. [Crossref] [PubMed]
- Harries V, McGill M, Yuan A, et al. Does macroscopic extrathyroidal extension to the strap muscles alone affect survival in papillary thyroid carcinoma? Surgery 2022;171:1341-7. [Crossref] [PubMed]
- Jin BJ, Kim MK, Ji YB, et al. Characteristics and significance of minimal and maximal extrathyroidal extension in papillary thyroid carcinoma. Oral Oncol 2015;51:759-63. [Crossref] [PubMed]
- Dionigi G, Ieni A, Ferraù F, et al. Pitfalls in the 2017 TNM Classification of Thyroid Carcinoma. J Endocr Surg 2018;18:98-109. [Crossref]
- Park SY, Kim HI, Kim JH, et al. Prognostic significance of gross extrathyroidal extension invading only strap muscles in differentiated thyroid carcinoma. Br J Surg 2018;105:1155-62. [Crossref] [PubMed]
- Yoon JK, Lee J, Kim EK, et al. Strap muscle invasion in differentiated thyroid cancer does not impact disease-specific survival: a population-based study. Sci Rep 2020;10:18248. [Crossref] [PubMed]
- Song E, Lee YM, Oh HS, et al. A Relook at the T Stage of Differentiated Thyroid Carcinoma with a Focus on Gross Extrathyroidal Extension. Thyroid 2019;29:202-8. [Crossref] [PubMed]
- Lyu YS, Pyo JS, Cho WJ, et al. Clinicopathological Significance of Papillary Thyroid Carcinoma Located in the Isthmus: A Meta-Analysis. World J Surg 2021;45:2759-68. [Crossref] [PubMed]
- Seo HW, Song CM, Ji YB, et al. Surgical Outcomes and Efficacy of Isthmusectomy in Single Isthmic Papillary Thyroid Carcinoma: A Preliminary Retrospective Study. J Invest Surg 2021;34:1129-34. [Crossref] [PubMed]
- Zhao W, You L, Hou X, et al. The Effect of Prophylactic Central Neck Dissection on Locoregional Recurrence in Papillary Thyroid Cancer After Total Thyroidectomy: A Systematic Review and Meta-Analysis: pCND for the Locoregional Recurrence of Papillary Thyroid Cancer. Ann Surg Oncol 2017;24:2189-98. [Crossref] [PubMed]
- Canu GL, Medas F, Conzo G, et al. Is prophylactic central neck dissection justified in patients with cN0 differentiated thyroid carcinoma? An overview of the most recent literature and latest guidelines. Ann Ital Chir 2020;91:451-7. [PubMed]
- Zhan S, Luo D, Ge W, et al. Clinicopathological predictors of occult lateral neck lymph node metastasis in papillary thyroid cancer: A meta-analysis. Head Neck 2019;41:2441-9. [Crossref] [PubMed]
- Lee YC, Na SY, Park GC, et al. Occult lymph node metastasis and risk of regional recurrence in papillary thyroid cancer after bilateral prophylactic central neck dissection: A multi-institutional study. Surgery 2017;161:465-71. [Crossref] [PubMed]
- Wu AW, Wang MB, Nguyen CT. Surgical practice patterns in the treatment of papillary thyroid microcarcinoma. Arch Otolaryngol Head Neck Surg 2010;136:1182-90. [Crossref] [PubMed]
- Makay Ö, Özdemir M, Şenyürek YG, et al. Surgical approaches for papillary microcarcinomas: Turkey's perspective. Turk J Surg 2018;34:89-93. [Crossref] [PubMed]
- McDow AD, Roman BR, Saucke MC, et al. Factors associated with physicians' recommendations for managing low-risk papillary thyroid cancer. Am J Surg 2021;222:111-8. [Crossref] [PubMed]


