Bilateral giant juvenile fibroadenomas of the breasts—a rare indication for bilateral skin reducing mastectomy
Introduction
Fibroadenoma is the most common benign tumor of the breast and typically occurs in women younger than 30 years old. Fibroadenomas are usually single, firm, rubbery masses with a well-circumscribed border (1). When they are found in children and adolescents they are called juvenile fibroadenomas (2). The majority of them grows slowly and usually attains a size of about 2 to 3 cm by the time they are detected by the patient (3). Those larger than 5 cm, weighting more than 500 g, or replacing at least 80% of the breast are called giant fibroadenomas (2).
Patients with bilateral giant juvenile fibroadenomas present a complex challenge to the attending surgeon, especially in the selection of the most appropriate surgical approach.
We describe a giant juvenile fibroadenoma case in an adolescent girl and we want to highlight the surgical approach.
Case representation
A 25-year-old white girl presented with a 2-year history of bilateral breast enlargement associated with dull pain (Figures 1,2). She had a case of menarche 10 years prior and was taking oral contraceptives. There was no family history of breast cancer.

Physical examination revealed enlarged breasts diffusely nodular with prominent veins in the tense and shiny overlying skin. The nodules are smooth and mobile, suggesting a benign disease. There was no discharge from the nipple, and axillary lymph-adenopathy was absent. The breasts and nipples are symmetric.
Ultrasonography of breast showed bilateral heterogeneous parenchymal pattern.
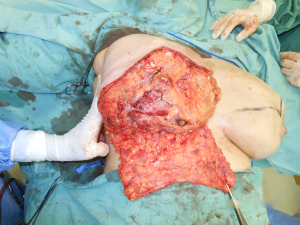
The patient was planned for bilateral skin reducing mastectomy using the inferior dermal flap, implant, and free nipple graft. Preoperative marking allowed for a standard Wise pattern incision with a 9 cm vertical incision (4). The vertical lines were drawn as close to the areola as possible and converged in the sulcus projection in the hemiclavicular line. Prior to the mastectomy, the nipple was removed as a full-thickness graft and set aside in saline solution. Incisions were made along the Wise pattern markings and the skin inferior to the markings was deepithelialized to the inframammary fold. A standard mastectomy was then performed by the mastologist. On exploration, both the breasts were found to be extensively studded with nodules of varying sizes with minimal normal tissue between the nodules (Figure 3). The right breast weighted 1.750 g and the left breast 1.525 g. Once the breast was removed from the pectoral fascia, the pectoralis major was raised superiorly and sutured to the inferior dermal flap. A 380 cc low profile textured round implant was placed in the pocket. The lateral edge of the dermal flap and of the pectoralis major muscle was then sutured to the serratus anterior muscle to cover the lateral edge of the implant (Figure 4). One suction drain was placed deep to the inferior dermal flap. The nipple donor site was centered 7 cm superior to the inframammary fold at the apex of the vertical incision. The nipple host site was deepithelialized and the nipple was sutures in place with a tie-over dressing.

The follow-up regimen was standardized, with wound review at 4 days and pathology result at 2 weeks, followed by further wound checks if necessary, but otherwise by review every 6 months until now. The histopathological examination showed diffuse fibroepitelial neoplasms, apocrine metaplasia, ductal ectasy and microcalcifications type 2. The surgery resulted in a very good cosmesis and the patient is very satisfied (Figures 5,6).
Discussion
Most fibroadenomas present as a single unilateral firm non-tender masses that may enlarge with relation to the menstrual cycle (5). Those larger than 5 cm, weighting more than 500 g, or replacing at least 80% of the breast are termed giant fibroadenomas (2). They are classified as either adult or juvenile type, later being rare (6). A giant juvenile fibroadenoma represent only 0.5% of all fibroadenomas (7) and when bilateral are much more rare.
The exact etiology of pathogenesis of giant fibroadenomas is still not understood completely. A major contributing factor is thought to be hormonal influence on adolescent breast. Excessive estrogen stimulation and/or receptor sensitivity or reduced levels of estrogen antagonist during puberty have been implicated (8,9).
In the treatment of typical fibroadenomas, a conservative approach is generally favored because they are not a known risk factor for breast cancer, and about 10% to 40% of cases resolve spontaneously (3). However, a giant juvenile fibroadenoma should be excised as its increasing size distort the shape of breast and can cause symptoms such as pain (6). Mastectomy as a treatment modality has been reported rarely (3,10-12).
For the rare cases requiring mastectomy as the initial form of excision, patients are likely to undergo reconstructive surgery. In our patient, we planned a bilateral skin reducing mastectomy using the inferior dermal flap, implant, and free nipple graft because of the large ptotic breast bilaterally. The preoperative marking allowed for a standard Wise pattern incision, preserving the breast envelope and creating an aesthetic and symmetric breast shape. The reconstructed breast had a pleasant medium-sized appearance, owing to the large room provided for the lower pole of the implant by the combined dermal-adipose pouch. Covering completely the implant with vascularized tissue (pectoralis muscle superiorly, deepithelialized dermal-adipose flap inferiorly and serratus muscle laterally) is very safe, diminishing the extrusion risk of the implant in case of skin necrosis, especially at the “T” junction that is as common as 30% (13).
Acknowledgements
None
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Amin AL, Purdy AC, Mattingly JD, et al. Benign breast disease. Surg Clin North Am 2013;93:299-308. [Crossref] [PubMed]
- Jayasinghe Y, Simmons PS. Fibroadenomas in adolescence. Curr Opin Obstet Gynecol 2009;21:402-6. [Crossref] [PubMed]
- Kaur N, Saini S, Somasekhar S, et al. Bilateral Florid Juvenile Fibroadenomas of the Breast in an Adolescent: A Rare Indication for Subcutaneous Mastectomy. J Pediatr Adolesc Gynecol 2015;28:e135-7. [Crossref] [PubMed]
- Wise RJ. A preliminary report on method of planning the mammaplasty. Plast Reconstr Surg (1946) 1956;17:367-75. [PubMed]
- Cerrato F, Labow BI. Diagnosis and management of fibroadenomas in the adolescent breast. Semin Plast Surg 2013;27:23-5. [Crossref] [PubMed]
- Gaurav K, Chandra G, Neelam K, et al. A pre-pubertal girl with giant juvenile fibroadenoma: A rare case report. Int J Surg Case Rep 2015;16:87-9. [Crossref] [PubMed]
- Sosin M, Pulcrano M, Feldman ED, et al. Giant juvenile fibroadenoma: a systematic review with diagnostic and treatment recommendations. Gland Surg 2015;4:312-21. [PubMed]
- Musio F, Mozingo D, Otchy DP. Multiple, giant fibroadenoma. Am Surg 1991;57:438-41. [PubMed]
- Issam M. Giant fibroadenoma. Case report and review of literature. Basrah J Surg 2006;12:1-4.
- Silfen R, Skoll PJ, Hudson DA. Florid juvenile (cellular) fibroadenomatosis in the adolescent: a case for subcutaneous mastectomy? Aesthetic Plast Surg 1999;23:413-5. [Crossref] [PubMed]
- Aygit AC, Altan A, Afşar Y. Breast reconstruction after subcutaneous mastectomy for extensive benign masses. Breast J 2004;10:163-4. [Crossref] [PubMed]
- Kanaan N, Goffin E. Multiple bilateral fibroadenomas of the breasts requiring mastectomy in a renal transplant patient. Clin Nephrol 2004;61:151-4. [Crossref] [PubMed]
- Salgarello M, Farallo E. Immediate breast reconstruction with definitive anatomical implants after skin-sparing mastectomy. Br J Plast Surg 2005;58:216-22. [Crossref] [PubMed]





