Stacked and bipedicled abdominal free flaps for breast reconstruction: considerations for shaping
Introduction
The deep inferior epigastric perforator (DIEP) flap has been demonstrated as the preferred method of autologous-based breast reconstruction with minimal donor site morbidity and often an aesthetic improvement in the abdominal contour (1-4).
The situation is made more difficult when reconstructing a relatively large breasted patient who has a smaller abdomen. Methods to address this have included the use of an implant with an abdominal flap (5), secondary lipofilling (6), contralateral reductions (7) or the use of stacked or bipedicled flaps to retain the entire abdominal pannus (8-17).
The vascular anatomical considerations are well described to aid the surgeon in terms of pedicle combinations, the need of intra-flap anastomosis and potential recipient vessels (8,9,18) (Table 1). However, little has been described on the aesthetic considerations on moulding the abdominal tissue to best match the contralateral side. We describe the various ways in which this tissue can be divided and layered, folded or coned in order to best achieve symmetry.

Full table
Classification systems for the vascular anatomy have been well documented (8,18). However, we appreciate that patients will be concerned about their eventual aesthetic outcome and hence this is the focus of our paper in shaping the abdominal pannus.
Materials and methods
A classification and outcome study for all stacked and/or bipedicled cases of DIEP flap reconstruction was assessed via a retrospective review of all cases from the St Andrew’s Centre for Plastic Surgery and Burns. This comprised 1,070 autologous breast reconstructions, undertaken between 2009 to 2014, of which 25 patients underwent stacked abdominal flaps, each undertaken to ensure adequate volume and skin replacement.
Specific data from all microsurgical free tissue transfer were prospectively entered into a clinical database, including patient demographics and key variables. All patients preoperatively underwent CT angiography to aid surgical planning, which involved at least a two-team approach. The breast surgery team undertook the mastectomy, whilst the plastic surgery team synchronously raised the flaps. The recipient vessels preparation took place once the mastectomy was completed. A shorter pedicle was raised if suitable intercostal perforator recipients were present. The flaps were shaped on a side bench, and intra-flap anastomoses would be performed for stacked flaps, or left as two separate pedicles for bipedicle flaps.
Anatomical classification for stacked abdominal flaps
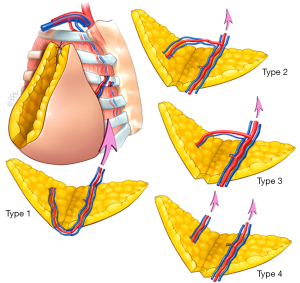
We utilized the classification of Murray and colleagues, who devised a simple classification for intra-flap anastomoses and pedicle combinations (Figure 1) (18). Choice in recipients vessels were in part related to the mastectomy surgeon, such that if an adequate intercostal perforator present and intact this would be the preferred first choice, as a short transfer could take place. For those undergoing an axillary clearance, the thoracodorsal axis is a good choice.
Shaping considerations for stacked DIEP flaps
There are four described ways to shape the abdominal pannus (Figures 2,3):

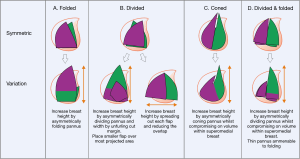
- Folded (Figure 2A):
- How: flap left undivided but folded in the midline (symmetrically) or off midline (asymmetrically). The later may be chosen if the breast height is longer than the hemi-abdominal length;
- Abdominal characteristics: for those with a think abdominal pannus with loose consistency and easily folded. Works well in those patients a narrower breas;
- Breast characteristics: tall, narrow breast with typically more volume in the inferior pole.
- Divided (Figure 2B):
- How: the abdominal pannus can be divided in the midline (symmetrically) or off midline (asymmetrically) and the skin paddles layered on top of each other;
- Abdominal characteristics: typically offer much more flexibility that simply folding the flap and can be used with any type of abdomen;
- Breast characteristics: flap division allows more flexibility to shape and match the contralateral breast size and shape. If the flaps are off set horizontally, an increased base width can be achieved. If a taller breast is required the abdominal tissue can be divided asymmetrically with placement of the smaller flap over the area of the greatest projection to match the contralateral side.
- Coned (Figure 2C):
- How: cranial margin of the abdominal tissue is sutured to itself and thus forms a cone. The coning can be performed symmetrically or asymmetrically;
- Abdominal characteristics: ideal circumstances to use this technique are when the caudal-medial abdominal pannus is modestly thick as this would form the inferior pole of the reconstructed breast. A thin pannus would form a flat shaped breast and would not be adequate for most reconstruction;
- Breast characteristics: useful for projected breasts with larger volumes in the inferior pole.
- Divided and folded (Figure 2D):
- How: the abdominal pannus is divided in the midline and each flap is folded in the horizontal plane;
- Abdominal characteristics: for those patients with a thin and pliable abdominal pannus;
- Breast characteristics: moderately projected breast shape. Divide the flap asymmetrically for those with taller breast size.
Decision regarding the choice of which of the above moulding techniques would be employed was dependant on both the contralateral breast and abdominal tissue quality and distribution. The contralateral breast shape, distribution of fat within each quadrant, its projection all played a part. The distribution of fat within the abdominal pannus, its consistency and relative thickness also played a part. Lastly, the quality of the recipient vessels within the chest and axilla also determined which vascular arrangements were possible.
Results
Over the 5-year period, 25 patients underwent stacked DIEP flaps, of which three-quarter (77%) were immediate. The average age of the patients was 48 years (range, 32–68 years) with a median follow-up of 2 years 10 months.
Over half the patients (57%) had bipedicle flaps with two recipient donor vessels and the remaining 43% had stacked flaps with intra-flap anastomoses leading to a single recipient donor. The most common recipient sites are the thoracodorsal vessels (62%) and intercostal perforators (26%) with the internal mammary (6%), posterior circumflex humeral (3%) and thoracoacromial vessels (3%) being the least common.
The average pedicle length was 10.2 cm (SD: 2.9 cm) with a range of 6–15 cm, with the microsurgical anastomoses time 38 mins (SD: 14 mins). The average flap elevation took 109 mins (SD: 42 mins), with the average time for the first flap being 112 mins and second flap 94 mins. The average abdominal pannus weight was 610 grams (SD: 320 grams), with a hemi-abdominal weighting 305 grams.
Of the 25 patients, two patients had haematomas within the breast pocket, one of which lost their reconstruction. One patient suffered with venous congestion of the flaps, which was salvaged.
Flap mounding and shaping was determined intra-operatively depending on the thickness of the abdominal pannus and fat distribution within it. In addition, comparison is made to the contralateral breast shape, size, footplate and glandular tissue distribution. Results of each type of shaping are shown together with a variety of possible vascular configurations (Figure 2). The most common shaping technique was with folded flaps (15 patients) (Figure 2B), followed by divided flaps (7 patients) (Figure 2B). The least common shaping patterns were coned (2 patients) (Figure 2C) and divided and folded flaps (1 patient) (Figure 2D).
Discussion
Bipedicled or stacked abdominal flaps allow the all four zones of the abdominal tissue to be used in unilateral breast reconstruction. This is a more demanding procedure but has been shown to be effective by many groups. The vascular considerations have been well described by Hamdi et al., DellaCroce et al., and Murray et al., however, less attention has been given to shaping of the reconstruction (8,9,18,19). We present a series of configurations that allow the reader to improved shaping of the abdominal pannus to optimised symmetry from what is available.
The complications included two haematomas, one of which led to flap failure. Another patient had a congested flap, which was salvaged. Of interest, no fat necrosis was observed in this series. It is described that the DIEP flap, can suffer fat necrosis in zone III and beyond and perhaps with our bipedicled or stacked flaps the blood supply is improved (9,18,19). Overall, we have a low complication rate.
The approach of tailoring the abdominal flaps to match the contralateral breast reconstruction is largely an art form. The shaping considerations we describe aim to bring some meaningful system to aid the surgeon to achieve the best possible outcome with the components presented to them.
Stacked flaps and bipedicled flaps are more demanding, as they require successfully raising two flaps from the abdomen without damage to the pedicles (18). We have anecdotally noticed that there is less fat necrosis in this group of patients compared to a unilateral DIEP in which zone III may be utilised. Others have showed this, especially when medial row perforator-based DIEP flaps are raised (20,21). The complication rates are relatively low and in keeping with the literature (9,18).
Conclusions
Stacked and bipedicled flaps have become more reliable and reproducible (19). The approach described requires perioperative decision making to achieve a matched breast shape from the abdominal pannus. We hope that this guide will aid with decision making as to which options suit each patient.
We believe that future developments to improve the aesthetic outcomes will employ 3D virtual surgical planning. 3D photography will allow assessment of the breast shape, symmetry and volume. Abdominal CT scan reformatted in 3D will allow better visualisation of the vascular anatomy and guide the surgeon to potential donor site volume and tissue thickness as to which approach will lead to the most optimal result (22-24).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Blondeel N, Vanderstraeten GG, Monstrey SJ, et al. The donor site morbidity of free DIEP flaps and free TRAM flaps for breast reconstruction. Br J Plast Surg 1997;50:322-30. [PubMed]
- Blondeel PN. One hundred free DIEP flap breast reconstructions: a personal experience. Br J Plast Surg 1999;52:104-11. [PubMed]
- Nahabedian MY, Dooley W, Singh N, et al. Contour abnormalities of the abdomen after breast reconstruction with abdominal flaps: the role of muscle preservation. Plast Reconstr Surg 2002;109:91-101. [PubMed]
- Futter CM, Webster MH, Hagen S, et al. A retrospective comparison of abdominal muscle strength following breast reconstruction with a free TRAM or DIEP flap. Br J Plast Surg 2000;53:578-83. [PubMed]
- Figus A, Canu V, Iwuagwu FC, et al. DIEP flap with implant: a further option in optimising breast reconstruction. J Plast Reconstr Aesthet Surg 2009;62:1118-26. [PubMed]
- Locke MB, Zhong T, Mureau MA, et al. Tug 'O' war: challenges of transverse upper gracilis (TUG) myocutaneous free flap breast reconstruction. J Plast Reconstr Aesthet Surg 2012;65:1041-50. [PubMed]
- Cheng A, Losken A. Essential elements of the preoperative breast reconstruction evaluation. Gland Surg 2015;4:93-6. [PubMed]
- Rabey NG, Erel E, Malata CM. Double-pedicled abdominal free flap using an entirely new microvascular combination of DIEP and SIEA vascular pedicles for unilateral breast reconstruction: a novel addition to the Hamdi classification. Plast Reconstr Surg 2012;130:767e-769e. [PubMed]
- Hamdi M, Khuthaila DK, Van Landuyt K, et al. Double-pedicle abdominal perforator free flaps for unilateral breast reconstruction: new horizons in microsurgical tissue transfer to the breast. J Plast Reconstr Aesthet Surg 2007;60:904-12. [PubMed]
- Barabás AG, Shafighi M, Sassoon EM, et al. The bilateral DIEP flap: a method of bipedicled anastomosis to a single internal mammary artery and venae comitantes. J Plast Reconstr Aesthet Surg 2008;61:1249-51. [PubMed]
- Blondeel PN, Boeckx WD. Refinements in free flap breast reconstruction: the free bilateral deep inferior epigastric perforator flap anastomosed to the internal mammary artery. Br J Plast Surg 1994;47:495-501. [PubMed]
- Lam TC, Sellars GD. Free perforator crossover TRAM flap for breast reconstruction. Ann Plast Surg 2003;50:126-31. [PubMed]
- Tseng CY, Lang PO, Cipriani NA, et al. Pedicle preservation technique for arterial and venous turbocharging of free DIEP and muscle-sparing TRAM flaps. Plast Reconstr Surg 2007;120:851-4. [PubMed]
- Agarwal JP, Gottlieb LJ. Double pedicle deep inferior epigastric perforator/muscle-sparing TRAM flaps for unilateral breast reconstruction. Ann Plast Surg 2007;58:359-63. [PubMed]
- Schoeller T, Wechselberger G, Roger J, et al. Management of infraumbilical vertical scars in DIEP-flaps by crossover anastomosis. J Plast Reconstr Aesthet Surg 2007;60:524-8. [PubMed]
- Ali RS, Garrido A, Ramakrishnan V. Stacked free hemi-DIEP flaps: a method of autologous breast reconstruction in a patient with midline abdominal scarring. Br J Plast Surg 2002;55:351-3. [PubMed]
- Figus A, Fioramonti P, Ramakrishnan V. Stacked free SIEA/DIEP flap for unilateral breast reconstruction in a thin patient with an abdominal vertical midline scar. J Reconstr Microsurg 2007;23:523-5. [PubMed]
- Murray A, Wasiak J, Rozen WM, et al. Stacked abdominal flap for unilateral breast reconstruction. J Reconstr Microsurg 2015;31:179-86. [PubMed]
- DellaCroce FJ, Sullivan SK, Trahan C. Stacked deep inferior epigastric perforator flap breast reconstruction: a review of 110 flaps in 55 cases over 3 years. Plast Reconstr Surg 2011;127:1093-9. [PubMed]
- Lee KT, Lee JE, Nam SJ, et al. Is Holm Zone III safe from fat necrosis in medial row perforator-based deep inferior epigastric perforator flaps? Microsurgery 2015;35:272-8. [PubMed]
- Santanelli F, Longo B, Cagli B, et al. Predictive and protective factors for partial necrosis in DIEP flap breast reconstruction: does nulliparity bias flap viability? Ann Plast Surg 2015;74:47-51. [PubMed]
- Hummelink S, Hameeteman M, Hoogeveen Y, et al. Preliminary results using a newly developed projection method to visualize vascular anatomy prior to DIEP flap breast reconstruction. J Plast Reconstr Aesthet Surg 2015;68:390-4. [PubMed]
- Gacto-Sánchez P, Sicilia-Castro D, Gómez-Cía T, et al. Use of a three-dimensional virtual reality model for preoperative imaging in DIEP flap breast reconstruction. J Surg Res 2010;162:140-7. [PubMed]
- Pacifico MD, See MS, Cavale N, et al. Preoperative planning for DIEP breast reconstruction: early experience of the use of computerised tomography angiography with VoNavix 3D software for perforator navigation. J Plast Reconstr Aesthet Surg 2009;62:1464-9. [PubMed]


