Minimally invasive thyroidectomy: a ten years experience
Introduction
The conventional thyroidectomy is the most frequent surgical procedure for thyroidal surgical disease. From several years were introduced minimally invasive approaches to thyroid surgery.
These new procedures improved the incidence of postoperative pain, cosmetic results, patient’s quality of life, postoperative morbidity.
The surgical approaches are different: from traditional minicervicotomy [open mini-invasive thyroidectomy (OMIT)] to video-assisted procedure [minimally invasive video-assisted thyroidectomy (MIVAT)], from extra-cervical incision as anterior chest wall, transareolar approach, transoral approach [transoral video-assisted thyroidectomy (TOVAT)], endoscopic axillary approach to robotic thyroidectomy (1-5).
The MIVAT is a minimally invasive procedure that uses a minicervicotomy to treat thyroidal diseases. We present our experience on 497 consecutively treated patients with MIVAT technique.
Materials and methods
From July 2005 to June 2015 we have consecutively treated 497 patients with MIVAT in University Hospital of Parma. All the cases respected the inclusion criteria to MIVAT as reported in Table 1.
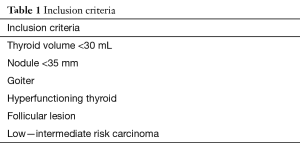
Full table
The MIVAT was performed in accord to video-assisted technique previously described by Miccoli (6); the surgical technique was performed by a minicervicotomy of 1.5–2 cm above the sternal notch and by a vertical dissection of prethyroidal muscles. The dedicated devices were used to identify the superior pedicle vessels using a 5-mm laparoscope at 30°. The section was conducted using titanium clips and/or Harmonic scalpel.
The camera grants a correct identification of parathyroids glands and the laryngeal nerves. We dissected the inferior pedicle vessels to remove the lobe.
Preoperative protocol included ultrasound evaluation to determine thyroid volume and locoregional nodal status, fine needle aspiration cytology (FNAC) in suspected thyroidal node in accord to Bethesda system (we revised the FNAC diagnosed before the Bethesda classification), serological evaluation [thyroid-stimulating hormone (TSH) reflex, calcitonin, thyreoglobulin, preoperative (parathyroid hormone) PTH], ENT evaluation in all patients before surgery.
We analyzed also the mean age, sex, mean operative time, rate of bleeding, hypocalcemia, transitory and definitive nerve palsy (6 months after the procedure), postoperative pain scale from 0 to 10 at 1 hour and 24 hours after surgery, mean hospital stay.
After the past 211 cases we excluded the patients affected by thyroiditis for the higher risk of nerve injury (7,8).
At 24 hours post thyroidectomy the serum calcium value has been recorded; in our experience a value lower than 8 mg/dL has been considered as hypocalcemia.
The adverse events rate in our experience matches with the incidence indicated by the Society of Endocrine Surgery Unit (www.clubdelleuec.it) in the accreditation society’s procedure (Table 2).
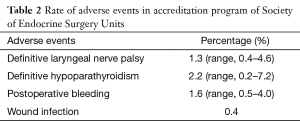
Full table
The values were evaluated with t student test (P<0.05 was statistically significant).
Results
On 497 cases the female/male ratio was 4:1, the mean age was 49.7 years.
The indications to treat were related to preoperative diagnosis: 182 THYR 5–6, 184 THYR 3–4, 27 plummer, 24 basedow, 28 toxic goiter, 52 goiter. The mean thyroid volume was 16.3±1.8 cm. The diameter of node THYR 3–6 was lower than 1 cm in 192 cases (52.4%) and between 1 and 3 cm in 174 cases (47.6%) (Table 3).
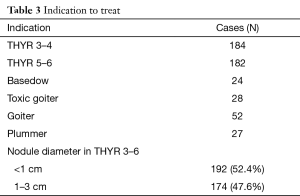
Full table
The mean surgical time “skin to skin” was 48±8.4 minutes. On 497 cases we have reported 1 case of bleeding (0.2%) that required a surgical revision through the same incision, 12 (2.4%) cases of transitory nerve palsy and 4 (0,8%) definitive nerve palsy. The rate of serologic hypocalcemia was 24.9% (124 cases) and clinical in 7.2% (36 cases); 1 case of hypoparathyroidism (0.2%) (Table 4).
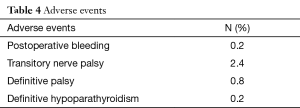
Full table
The postoperative pain values were 2.3±1.2 after 1 hour and 1.06±0.56 after 24 hours (P<0.01).
In 27 cases we used Intraoperative neuromonitoring started by October 2014 (Figure 1).

The cosmetic results were defined as excellent in 434 patients, good in 55 cases and sufficient in 8 patients. We converted in CT 24 cases (4.8%): 13 for thyroiditis, 11 thyroid volume. The mean hospital stay was 1.3 days.
Discussion
Minimally invasive procedures have changed the surgical approach to surgical diseases in the last 20 years.
Regarding the thyroid surgery different techniques are described from different surgical teams. We consider as minimally invasive approach not only a mini incision but also the tissue’s dissection.
The MIVAT is in our experience a good and safe minimally invasive approach for thyroidectomy in accord to inclusion criteria modified by the experience. The MIVAT can be safely utilized in patients with, follicular proliferation, low or intermediate risk differentiated thyroid cancer (DTC), goiter with euthyroidal or hyperfunctionally hormone status. We have excluded after the first 211 cases (7) the patients affected by DTC in thyroiditis for the higher risk of dysphonia related to the risk of excessive traction during laryngeal nerve identification.
Others minimally invasive procedures are reported but all the procedures regarding the extra-cervical incision are related to higher rate of adverse events particularly pneumothorax, chest paresthesia, brachial plexus injury, local wound infection, perforation, chest pain, Horner’s syndrome. The robotic thyroidectomy is penalized by the cost higher than conventional cervical or MIVAT.
In 2015 Hinson et al. (9) analyzing the trends in robotic surgery in the United States reported that the majority of volume of robotic procedure in thyroid surgery are performed in lower volume centers and that it may be associated to higher complication rates.
The robotic thyroidectomy was improved in South Korea where the reimbursement for robotic thyroidectomy is quadruple than conventional thyroidectomy. In our Health National System the reimbursement for conventional thyroidectomy is just enough to repay the hospital costs.
The use of MIVAT vs. conventional thyroidectomy is reported also in randomized controlled trials that highlighted as the two procedures have similar short terms outcomes (10). We highlighted as the adverse events are similar between conventional technique and MIVAT; however the postoperative hypocalcemia or the intraoperative parathyroid identification are better than conventional thyroidectomy. Zheng et al. demonstrated that the degree of immunosuppression was lower in MIVAT minimizing the trauma (11).
The MIVAT is comparable to conventional thyroidectomy also regarding the costs because the laparoscopic column is today present in all the operative rooms as the 30° 5 mm degree camera.
The disposable devices are used routinely in endocrine surgery. The use of intraoperative neurophysiological monitoring (IONM) is safe as in our 27 cases consecutively treated patients with MIVAT. Dionigi et al., reported a real benefit in video-assisted procedure, the surgeon is more comfortable during nerve identification (12,13).
We have recently published our study on the use of MIVAT in papillary thyroid cancer (14); Miccoli (15,16) reported that this procedure can be utilized in PTC with intermediate risk and Lombardi (17) highlighted that in selected cases of PTC the central compartment dissection with video-assisted technique is comparable to conventional treatment.
The last guidelines are highlighting the possibility to treat the DTC with a more conservative surgical approach (18,19). These cases may be ideal to treat with minimally invasive procedures according the inclusion criteria.
We think that the difference between this minimally invasive procedure and the others reported is the reproducibility, lower tissue dissection and safety.
Conclusions
The MIVAT is a safe approach to surgical thyroid disease, the cost are similar to CT as the adverse events. The cosmetic results are better and the use in experienced hands is indicated also to treat intermediated DTC. The minicervicotomy is really a minimally invasive tissue dissection.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Shimizu K, Akira S, Jasmi AY, et al. Video-assisted neck surgery: endoscopic resection of thyroid tumors with a very minimal neck wound. J Am Coll Surg 1999;188:697-703. [Crossref] [PubMed]
- Gagner M, Inabnet WB 3rd. Endoscopic thyroidectomy for solitary thyroid nodules. Thyroid 2001;11:161-3. [Crossref] [PubMed]
- Ikeda Y, Takami H, Sasaki Y, et al. Endoscopic neck surgery by the axillary approach. J Am Coll Surg 2000;191:336-40. [Crossref] [PubMed]
- Lee J, Yun JH, Nam KH, et al. The learning curve for robotic thyroidectomy: a multicenter study. Ann Surg Oncol 2011;18:226-32. [Crossref] [PubMed]
- Terris DJ, Duke WS. Robotic and remote access thyroidectomy: a time to pause. World J Surg 2013;37:1582-3. [Crossref] [PubMed]
- Miccoli P, Berti P, Conte M, et al. Minimally invasive surgery for thyroid small nodules: preliminary report. J Endocrinol Invest 1999;22:849-51. [Crossref] [PubMed]
- Del Rio P, Arcuri MF, Pisani P, et al. Minimally invasive video-assisted thyroidectomy (MIVAT): what is the real advantage? Langenbecks Arch Surg 2010;395:323-6. [Crossref] [PubMed]
- Del Rio P, Arcuri MF, Cataldo S, et al. Are we changing our inclusion criteria for the minimally invasive videoassisted thyroidectomy? Ann Ital Chir 2014;85:28-32. [PubMed]
- Hinson AM, Kandil E, O'Brien S, et al. Trends in Robotic Thyroid Surgery in the United States from 2009 Through 2013. Thyroid 2015;25:919-26. [Crossref] [PubMed]
- Pisanu A, Podda M, Reccia I, et al. Systematic review with meta-analysis of prospective randomized trials comparing minimally invasive video-assisted thyroidectomy (MIVAT) and conventional thyroidectomy (CT). Langenbecks Arch Surg 2013;398:1057-68. [Crossref] [PubMed]
- Zheng C, Liu S, Geng P, et al. Minimally invasive video-assisted versus conventional open thyroidectomy on immune response: a meta analysis. Int J Clin Exp Med 2015;8:2593-9. [PubMed]
- Dionigi G, Boni L, Rovera F, et al. Neuromonitoring and video-assisted thyroidectomy: a prospective, randomized case-control evaluation. Surg Endosc 2009;23:996-1003. [Crossref] [PubMed]
- Deniwar A, Kandil E, Randolph G. Electrophysiological neural monitoring of the laryngeal nerves in thyroid surgery: review of the current literature. Gland Surg 2015;4:368-75. [PubMed]
- Del Rio P, Maestroni U, Sianesi M, et al. Minimally invasive video-assisted thyroidectomy for papillary thyroid cancer: a prospective 5-year follow-up study. Tumori 2015;101:144-7. [Crossref] [PubMed]
- Miccoli P, Matteucci V. Video-assisted surgery for thyroid cancer patients. Gland Surg 2015;4:365-7. [PubMed]
- Miccoli P, Biricotti M, Matteucci V, et al. Minimally invasive video-assisted thyroidectomy: reflections after more than 2400 cases performed. Surg Endosc 2015. [Epub ahead of print]. [Crossref] [PubMed]
- Lombardi CP, Raffaelli M, De Crea C, et al. Video-assisted versus conventional total thyroidectomy and central compartment neck dissection for papillary thyroid carcinoma. World J Surg 2012;36:1225-30. [Crossref] [PubMed]
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines); Thyroid Carcinoma,Version 2.2015. Available online: http://www.nccn.org/professionals/physician_gls/pdf/thyroid.pdf
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;26:1-133. [Crossref] [PubMed]


