Prosthetic breast reconstruction: indications and update
Introduction
In 2010, breast cancer was the most common cancer amongst Australian women, with 14,181 new diagnoses (1). Breast cancer comprises 28% of all new cancers in women and the risk of developing breast cancer before the age of 85 is 1 in 8 (1). Approximately 35-40% of women diagnosed with breast cancer undergo a total mastectomy, a trend which is increasing (2). Fewer than 33% of those who are suitable undergo breast reconstruction (2) despite 82% of women reporting psychosocial improvement following reconstruction (3).
Although reconstruction using a transverse rectus abdominis musculocutaneous (TRAM) flap or a deep inferior epigastric artery perforator (DIEP) flap offers women the option of autologous reconstruction, prosthetic reconstruction is still widely used. Data from the United States indicate that between 1998 and 2008, there was an 11% increase in the use of implants per year, whereas autologous reconstruction rates remained stable (4,5). Indeed, the data shows that prior to 2002, autologous reconstructions were the more frequently chosen method of reconstruction compared with the use of prostheses. However, after 2002, this relationship was reversed and in 2008 implants outnumbered autologous reconstructions by a ratio of 2:1 (258 vs. 120 per 1,000 mastectomies) (4). Albornoz et al. (4) suggests a number of reasons behind this change in trend; the longer time it takes to perform autologous reconstruction, a cultural shift towards acceptance of breast implants, and the way in which reconstruction is funded. In the US Medicare funding for autologous implants decreased between 1998 and 2008. Also private insurance companies increased payment for implant reconstruction by 64%, while reimbursement for autologous reconstruction was unchanged (4).
In the 1960s silicone breast implants were introduced, launching the era of modern breast reconstruction. Radovan (6) pioneered the use of tissue expanders in the early 1980s which has allowed for further reconstructive options. Since then, there have been great advances in the both the technique of expander/implant breast reconstruction and in the prostheses themselves (7).
The decision for autologous vs. prosthetic reconstruction is a decision that requires a long discussion between the patient and surgeon which must take into account many factors. There are many advantages and disadvantages that autologous reconstruction has over prosthetic reconstruction which is outside the scope of this article. Once the decision has been made to pursue prosthetic breast reconstruction, the aim of this article is to provide a summary of the current data to assist the clinician in the complex decision making process that follows.
In considering prosthetic breast reconstruction, a number of factors need to be considered by both surgeon and patient. The indications and selection of patients for prosthetic reconstruction will be discussed as will the timing of reconstruction following mastectomy. Integral to this is determining whether or not adjunctive therapy is required as this can greatly affect the outcome of prosthetic reconstruction.
Methods
The current study comprises a systematic review of the literature focusing on the evidence for prosthetic breast reconstruction.
Study identification
Multiple databases were searched independently by two authors (TQ and GM), including: Ovid Medline (1950 to present), EMBASE (1980 to 2015), PubMed and Cochrane Database of Systematic Reviews.
The following search terms and Boolean operators were used: (I) “breast reconstruction” or “breast neoplasm,” or “breast implants” or “breast” and (II) “alloplastic” or “prosthesis” or “implants”. Additional searches were conducted using (I) and (II) and “tissue expansion devices” or tissue expander”; (I) and (II) and “surgical flaps” or “mammoplasty” or “mastectomy” as well as (I) and (II) and “reconstructive surgical procedure”.
Inclusion criteria
Inclusion criteria for studies reviewed included: (I) meta-analyses or review articles; (II) adult patients aged 18 years or over undergoing post-mastectomy alloplastic breast reconstruction (i.e., tissue expander or implant based); (III) studies including outcome measures; (IV) case series with more than 10 patients; (V) published since 1 January 2000; and (VI) English language.
Data extraction
A systematic review was conducted using the PRISMA 2009 statement. Data was extracted by two authors (TQ and GM), and included author, year, journal, study design, level of evidence, outcome details, number of patients (if applicable), and follow up period. Differences in data extraction were corrected via discussion.
Literature search results
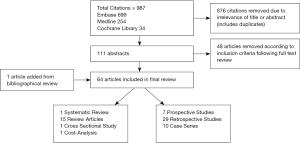
The search was conducted on April 10, 2015, resulting in 987 articles, managed using Endnote X7TM (Thomson Reuters, Philadelphia, PA). A summary of the literature review process is shown in Figure 1. After the authors independently assessed the titles a total of 876 articles were removed for irrelevance or duplication. The abstracts for the remaining articles were then reviewed based on the inclusion criteria, leaving a total of 111 articles for full review. A further one article was added based on review of bibliographies. Fifty studies were eliminated after full review (due to publication date prior to the year 2000, inadequate outcome measures, and case series fewer than 10 patients). After full text review, analysis and data extraction was conducted for a total of 62 articles, summarized in Table S1.

Full table
Outcomes on the 62 articles that met the inclusion criteria were summarized and analyzed. The breakdown of the types of articles included was 1 systematic review, 14 reviews, 7 prospective studies, 26 retrospective studies, 10 case series, 1 cost-analysis, and 3 cross-sectional studies).
Discussion
Indications and patient selection
Most patients who undergo mastectomy for breast cancers are candidates for prosthetic reconstruction. There are factors that limit a patient’s ability to undergo autologous reconstruction. This may include general medical health, an unsuitable donor site, lifestyle factors and availability of resources. Prosthetic breast reconstruction, however, can be a safe and viable option, even for older patients. Indeed, Hershman et al. [2012] reported that the immediate in-hospital complication rate was significantly higher in patients who underwent autologous reconstruction when compared to those who had prosthetic reconstruction (8).
The choice of whether or not to undergo reconstruction can be a complex. This has been studied by Reaby et al. [1998] (9) and by Ng et al. [2014] (10). Many patients choose not to undergo reconstruction. This may be because they lack information about the procedures, do not feel that it was necessary for their physical or emotional well-being or that due to fears that it would mask cancer recurrence (9). Of the approximately 33% (2), however that do choose reconstruction, they report that they did so because they could get rid of external prostheses, be able to wear many types of clothing, regain their femininity and to feel “whole” again after the surviving breast cancer (9). In the areas of social functioning and emotional wellbeing, it has been reported that patients who underwent reconstruction did better than those who did not have reconstruction (11). Some patients may have unclear and potentially inaccurate expectations of the appearance of, and physical sensation, in particular the “unnatural feel”, firmness and lack of movement, associated with prosthetic breast reconstruction which can lead to dissatisfaction with the outcome (12).
Definitive reconstruction with an implant can be done either at the time of the mastectomy, referred to in this article as immediate breast reconstruction (IBR), or as a two-stage reconstruction with a tissue expander followed by a permanent implant and most of the time with intervening (13) adjuvant therapy, a process referred to in this article as delayed breast reconstruction (DBR). Clinicopathological features which are considered when making decision regarding the type of reconstruction include cancer stage, status of the sentinel node, smoking, body habitus, pre-existing scars and prior radio or chemotherapy (14).
Immediate reconstruction is preferred where possible because of the psychological and physical benefits attained from restoration of mammary volume and shape (15) and is associated with a high level of patient satisfaction (16). Prosthetic breast reconstruction has the advantages of shorter procedure time, hospital stay and recovery as well as being lower cost (17) and not having an additional donor site associated with an autologous reconstruction (18). Unfortunately, having prosthetic IBR is associated with requiring unplanned surgery in the future to revise the reconstruction (19,20) and a higher complication rate related to prosthesis failure (21). Patients with small, minimally ptotic breasts are ideal candidates for single-stage reconstruction (22) as are patients who have a good cancer prognosis, who are sentinel node negative and therefore do not require axillary surgery and have late local recurrence (LR) in a previously treated breast (23). Patients with larger and/or ptotic breasts are not ideal candidates for IBR as they often need contralateral balancing procedures to achieve symmetry which can be difficult to judge at the time of immediate reconstruction (24).
Delayed or two-stage reconstruction with a tissue expander followed by a permanent implant is an alternative pathway for prosthetic reconstruction. Tissue expansion is simple, safe and allows for preservation of the skin envelope and allows for better matched color, texture and hair-bearing qualities of the skin (25). It also allows for implantation of synthetic materials underneath the expanded tissue as the skin flaps are vascularized (25). Tissue expansion is recommended in patients who require adjuvant radiotherapy as radiotherapy can adversely affect the aesthetic outcome, and tissue expanders can impede effective and safe radiation delivery to the internal mammary and axillary lymph nodes (26).
Breast reconstruction in the elderly
Despite the recent increase in the rate of immediate reconstruction, many older women choose not to undergo breast reconstruction following mastectomy due to the fear of complications and the perception that they are “too old” for the procedure (9).
The literature indicates that older patients tolerate breast reconstruction well. Walton et al. [2011] reports similar complication rates in older compared to younger patients but that autologous reconstruction result in better outcomes than implant reconstruction (11). August et al. [1994] reported, in a patient cohort of 242, that there were significantly fewer complications in women over the age of 60 following both IBR and DBR. It was also noted that older women tended to require fewer operations to achieve the final results compared to their younger counterparts (27).
Risks and complications of prosthetic reconstruction
The most common complications associated with prosthetic reconstruction include capsular contracture, hematoma and infection (28). The complication rate was significantly lower when implants were inserted for cosmetic reasons (6.5% at 1 year and 12% at 5 years) compared to those who had expanders inserted either following prophylactic mastectomy (17.3% at 1 year and 30.4% at 5 years) or mastectomy for cancer (21.8% at 1 year and 34% at 5 years) (28). In a systematic review of 14 observational studies, which included more than 3,000 breasts, Tsoi et al. [2014] concluded that reconstructive failure and surgical site infection was higher in patients who had prosthetic reconstruction compared to those who underwent autologous reconstruction (29).
Wound complications are associated with large breast volume (greater than 750 g) and sternal notch to nipple length of greater than 26 cm (30). Significant risk factors for reconstructive failure include smoking (31), obesity (32), incomplete muscle coverage (31), implant volume >400 mL (31), type 2 diabetes mellitus (32), higher grade tumors and nodal involvement (33). Although not a statistically significant risk factors for complications, older age was associated with a borderline increased risk of complications in both IBR and DBR (31). Tamoxifen, an oestrogen receptor antagonist use is associated with a borderline risk of complications but a significant risk of reconstructive failure in patients who undergo expander/implant reconstruction (34).
Capsular contracture
Capsular contracture development is multifactorial. Numerous potential aetiologies and contributing factors have been described including bacterial colonization, the type and texture of the implant, the placement of the implant and the use of radiotherapy (35). Overall incidence of significant capsular contracture (Baker classification III or IV) ranges from 10.4% (36) to 29% (37). Capsular contracture rates in immediate reconstruction has been reported as being between 20% (38) to 40.4% (39) and rates for delayed reconstruction range from 17% (39) to 26.4% (38). Smoking, use of smooth implants (40) and hematoma increased the risk of developing contractures, as does the duration of implantation (41).
Staphylococcus epidermis’s is the bacteria most implicated in capsular contracture. It exists in the ductal system in the breast and has been cultured from breast milk, nipple secretions and biopsied from breast parenchyma (42). Bacterial etiology is a likely major contributor of capsular contracture. Bacteria adhere easily to silicone and form a biofilm comprised of extracellular polysaccharides and glycoprotein. Virden et al. (42) cultured 55 silicone implants at the time of removal. Bacterial growth was detected in 56% of implants surrounded by contracted capsules compared to 18% of implants without contracted capsules, a significant difference. Patients who undergo radiotherapy are at significant risk of developing capsular contracture. Patani et al. [2008] reports a rate of capsular contracture requiring capsulotomy as a staggering 87%, compared to 13% in those who did not have radiotherapy (43). Of the 71% of patients receiving radiotherapy who developed capsular contracture in the study conducted by Ringberg et al. [1999], 8% had Baker classification III and IV contractures (44). The use of a flap with the implant seems to mitigate capsular contracture, reducing the risk of capsular contracture to 6.8% compared to a rate of 25% of those who had implants alone (41).
In a series of 326 tissue expanders, Rheingold et al. [1994] reported an overall contracture rate of 78.5% Baker I, 12% Baker II, 8.6% Baker III and 0.9% Baker IV contractures (45). Holmes et al. [1989] reported that neither the speed of expansion, nor the degree of over-expansion influenced the onset of contracture. However, patients with Baker I contractures had a significantly longer interval been full expansion and definitive recon than did those who developed Baker III contractures (37).
Types of prostheses
Silicone vs. saline implants
Gylbert et al. [1990] reported a higher capsular contracture rate in silicone implants (50%) compared to 16% of saline implants. However, 16% of the saline implants deflated. Despite the higher contracture rates amongst the silicone implant group, 85% of the patients in this study reported that they were satisfied with the reconstruction (46). Both Macadam et al. [2010] (47) and McCarthy et al. [2010] (48) report that patients who have silicone implants have higher quality of life and satisfaction scores than those with saline implants. There is also a statistically significant difference in overall physical function (silicone implants performed better) and systemic side effects (higher in patents with saline implants).
Despite concerns, there has been no associations found between silicone implants and cancer, immunological or systemic disease (49).
A prospective review from 1990 to 1997 by Spear et al. [2000] reviewed 40 consecutive patients with saline implants (50). Almost half (47.5%) of irradiated breasts with saline implants required revision or replacement by a flap (compared to 10% of control group who required revision with a flap but none required replacement). Patients with saline implants also had higher contracture rate of 32.5%
One type of implant containing hydrogel filler (polyvinylpyrrolidone and guar gum) was reported as having similar contracture rates to saline implants but twice the rupture rate. This was subsequently withdrawn from use in the United Kingdom market in 2000 (51).
Round vs. anatomic implants
The consensus is that there is no difference seen between round and shaped implants including rippling, overall satisfaction with breast and outcome (52).
Cohesive gel implants are comprised of a textured silicone elastomer shell filled with cohesive silicone gel. There is increased number of cross links between gel molecules which results in better shape retention and less likely to collapse (53). Highly cohesive shaped devices have been reported to be firmer than the less cohesive round implants. In addition, because of the added cohesivity of the shaped implant, there may be less rippling (52). In cases that involve reconstructing an upper pole deficiency of the breast an anatomic implant is favoured. Round implants are usually favoured when there is no appreciable upper pole deficiency. Nahabedian et al. [2014] reported similar complication rates between the two strategies (54).
Textured vs. smooth implants
Textured implants form thinner and more pliable capsules that are less likely to contract than smooth implants. In a review of 16 randomized control trials and two retrospective trials, Liu et al. [2015] found that smooth implants were more likely to be associated with capsular contracture than textured implants (55). About 96% of textured implants were reported to have a satisfactory (Baker classification Grade II or better) result compared to 72% of patients who had a smooth implant inserted (56).
The contracture rate reported by Embrey et al. [1999] was 58% for smooth implants compared to 8% for textured implants (35). Hakelius et al. [1992] performed bilateral, sub-glandular implant insertion in 25 patients for mammary hypoplasia. In each case one smooth and one textured implant was inserted. It was found that at 1 year, the textured implant was less likely to develop contractures (57). Longer-term follow up at 10 years found a reduced rate of contractures in textured implants compared to smooth implants (58) with a reported contracture rate of 65% in smooth implants vs. 11% in textured implants (40). Not only are smooth implants associated with significant capsular contracture they also are more likely to be displaced as well as having higher rates of infection and pain on expansion (59). Textured implants, in contrast, maintained their position and expanded easily with minimal pain (59).
Integrated port vs. distant port tissue expanders
The Becker Expander, (TM) a textured tissue expander produced by Mentor, which has a distant port, offers the advantage of single-stage reconstruction. The expander is filled until the desired volume is reached prior to the ports being removed under local anesthetic and the expanders being left in-situ as implants. Large series have reported good outcomes at 3 years. However at 5 years Chew et al. [2010] found that 68% were removed due to complications (poor aesthetics, capsular contracture, infection). The congenital hypoplasia group had better retention rates (67% at 10 years) than oncological (2%) or risk reducing mastectomy (5%) groups (60).
Spear et al. [1998] performed 171 consecutive reconstructions using textured, integrated valve expanders. All were two-stage reconstructions. Four percent deflated over 7 years, 2 were removed for infection and 1 electively. About 98% of a subgroup of 42 patients were satisfied with their reconstructions (61). Yanko-Arzi et al. [2009] found more complications with integrated-valve expanders compared to those with distant inflation ports (62).
Timing of reconstruction with prostheses
Albornoz et al. [2013] reports that from 1998 to 2008, there was a 78% increase in the rate of IBR from 20.8% to 37.8%, an average of 5% per year (4). IBR gives the best aesthetic outcome if radiotherapy is not required (63), and patients who received IBR had better physical and psychosocial scores than those undergoing DBR (64). As mastectomy defects can result in the loss of body integrity and femininity, patients who have IBR have higher satisfaction levels than those who have delayed reconstructions (32). Factors associated with an increase likelihood of IBR included large hospital size with a high number of patients requiring IBR and surgeons who perform IBR regularly. Decreased likelihood was associated with increased age, black race, patients who were married, patients from rural locations and patients with increased comorbidities (8).
The early complication rate ranges from 9.2% (65) to 16% (66) and include skin flap necrosis, infection, sarcoma, hematoma and a 1.7% risk of explantation (65). Late complication rates have been reported to be as high as 23% (65). Unfortunately the cosmetic outcome following IBR diminished over time from 86% acceptable cosmetic appearance at 2 years to 54% acceptable cosmetic appearance at 5 years, independent of radiotherapy, type of implant, volume of implant, age of the patient or the type of mastectomy incision used (65).
There is a reported revisional surgery rate of 30.2% following IBR (65). Fifty seven percent of IBR required revision compared to 27% of DBR (67), although the two groups had similar complication rates and failure rates. Patients undergoing IBR also need more capsular intervention procedures which leads to greater expense but they can obtain good results due to revisional surgery (68). The risk of requiring revision is higher if the patient has undergone radiotherapy, is D-cup size or larger, or has grade 2 or 3 ptosis of the breast (67).
The rate of complications is higher in patients who have IBR compared to the DBR group (69), with capsular contracture being the most significant complication (40.4% vs. 17%) (39). The negative effect of radiotherapy is more significant with IBR than DBR groups (70). The rate of implant loss has been reported from 1.7% (65) to 18% (31). IBR is reported to have a higher overall complication and implant failure rate than DBR (71).
Delayed-immediate reconstruction
Patients who are anticipated to require radiotherapy who desire breast reconstruction are considered candidate for delayed-IBR (63). Using the delayed-immediate protocol enables surgeons to provide the near optimal reconstruction despite whether radiotherapy eventuates or not. Those patients who do not end up needing radiotherapy achieve aesthetic results comparable to patients who undergo IBR. For the patients who do end up receiving radiotherapy, the aesthetic problems usually associated with radiotherapy following IBR are avoided (30). This protocol of breast reconstruction also allows for skin-preserving DBR after radiotherapy for patients in whom radiotherapy only becomes apparent after review of the pathological sections post mastectomy. Preserving the breast skin envelope in patients who have undergone radiotherapy allows for the direct placement of an implant and decreases the need for addition of autologous flaps or at least minimizes the dimensions of the skin island required from an autologous flap.
In stage 1 of a delayed-immediate reconstruction, patients undergo a skin sparing mastectomy plus the insertion of an expander, with or without the addition of an acellular dermal matrix (ADM). The expander is then filled to the required volume intraoperatively. The pathology is subsequently examined and the patient discussed at a multidisciplinary team (MDT) meeting. If radiotherapy is not required, the patient proceeds to have definitive reconstruction (stage 2) with an autologous flap, flap plus implant or implant alone. If radiotherapy is required, however, the expander is deflated following the course of chemotherapy (if the patient is having it) and prior to radiotherapy planning. She then undergoes radiotherapy, has the expander re-expanded then completes stage 2 of the reconstruction three months after radiotherapy is completed.
Delayed breast reconstruction (DBR)
DBR is significantly more common in the USA than elsewhere in the world (72). A two-stage reconstruction gives a more predictable result as it can be adjusted at the second operation (24). Multiple authors have suggested that patients who undergo DBR have fewer complications than patients who have IBR. Francel et al. [1993] found that patients who had DBR were less likely to require surgery to correct capsular contracture (67). Cosmetic results in patients who have DBR 6 weeks after radiotherapy were found to be superior when compared to those who had IBR (73). The timing of reconstruction after radiotherapy is also important. Lentz et al. [2013] studied patients who had reconstruction within 4 months following compared to patients who had reconstruction greater than 4 months after radiotherapy. The former group had a non-significant trend towards increased infection whilst the latter tended to have a higher capsular contracture rate (74).
The concept of “delayed-delayed” prosthetic reconstruction is described by Kronowitz et al. [2015] (26). Neoadjuvant chemotherapy and radiotherapy in conjunction with skin sparing mastectomy in patients who have locally advanced breast cancer is increasingly resulting in good long-term disease control and survival (26). Following neoadjuvant chemotherapy, which decreases the need to resect skin at the time of mastectomy, patients with locally advanced breast cancer are discussed at an MDT and eligibility for skin sparing DBR is decided. For those that are deemed suitable, they undergo a skin-sparing mastectomy with insertion of a tissue expander with or without ADM. The expander is filled intra-operatively but then is partially deflated immediately prior to planning for radiotherapy. After the resolution of any radiation induced skin desquamation the expander is re-inflated to the pre-deflation volume and 3 months after radiotherapy and re-inflation, the definitive reconstruction is performed. The aim of this is protocol is to improve aesthetic outcome, decrease complications and reduce psychological disadvantages associated with DBR after radiotherapy.
Radiotherapy and prosthetic breast reconstruction
More centers globally are recommending radiotherapy for patients with breast cancer, including early breast cancer, which increases the complexity of reconstructive planning (26). The USA has been reported to have higher rates of reconstruction prior to radiotherapy than elsewhere in the world (72). Chen et al. [2013] found that 57% of 358 surveyed radiation oncologists felt that breast reconstruction challenged their ability to deliver effective radiation. Sixty percent preferred a moderately inflated expander (150-250 CC) compared to completely deflated (13%) or completely inflated (28%) (72).
In a review article by Fodor et al. [2003] the most common type of complication associated with radiotherapy was significant capsular contracture (Grade III or IV) (69). Rates of capsular contracture varied from 29% (75) to 68% (76) in patients who had radiotherapy compared to 10% (77) to 40% (34) of those who did not have radiotherapy. The risk of significant capsular contracture (Baker Grade III or IV) was also higher in irradiated breasts (33). Patients who had moderate skin changes and no induration had similar aesthetic outcomes to non-irradiated chest walls. However those who developed induration or severe post-radiotherapy skin changes had a greater chance of Baker IV contracture (78). Capsular contracture was also found to be associated with a significant increase in persistent pain 2 years following surgery (79).
The risk of overall complications was also found to be significantly higher in patients who had radiotherapy (80). Fodor et al. [2003] reports that 0-64% of IBR patients and 22-55% of DBR developed complications compared to 0-12% of IBR patients and 13-34% of DBR who did not have radiotherapy (70). Radiotherapy is also associated with significantly higher rates of reconstruction failure with rates varying from 22.7% (33) to 37% (34). As such, radiotherapy significantly increases the number of secondary procedures required in both unilateral and bilateral reconstruction (81,82). Reconstruction with prostheses following radiotherapy was found to be much more reliable when used in conjunction with a flap (83,84). Overall, patients who have radiotherapy have significantly lower satisfaction with their physical and psychosocial outcomes compared with non-irradiated patients when adjusted for other treatment factors (85).
Outcomes
Satisfaction rates following prosthetic breast reconstruction is up to 85% (16,44). Lifestyle and social relations had improved in 82% and 53% of patients respectively post reconstruction (3). Klit et al. [2013] reported that there was no significant difference in the reported levels of pain experienced by patients who had prosthetic reconstruction compared to those who did not. Also, the timing of the reconstruction (immediate vs. delayed) did was not associated with a significant difference in pain (86). Although 60% of reconstructions resulted in some complication or complaint, patients feel more balanced and whole, are less depressed and were glad they had the reconstruction (87).
The patient’s acceptance of cosmesis was found to be better if she could see photos or have a discussion with patients who had previously undergone similar process (88). Having bilateral (vs. unilateral) and not having radiotherapy were significant predictors in good cosmetic outcomes (36). Understandably, failure of the reconstruction was associated with significantly decreased aesthetic satisfaction (34).
In order to give all eligible patients equal opportunity to have the best possible outcomes with breast reconstruction, treatment should be centralized in hospitals with a MDT team comprising of, amongst others, an oncological breast surgeon, pathologist, radiologist, oncologists and plastic surgeons (89).
Conclusions
Implant reconstruction following mastectomy has increased at a steady rate since 1998 and is now utilized more frequently than autologous reconstruction. This trend can be attributed to the increased understanding of indications and patient selection for implant reconstruction. This understanding is derived from evidence regarding common and long-term complications, as well as evidence regarding type of prostheses; timing options for reconstruction; and the adjuvant use of radiotherapy (Table 1). We can now more reliably predict outcomes of reconstruction on an individual basis and assess patient suitability to many different reconstructive options.

Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Australian Institute of Health and Welfare (AIHW) 2015. Australian Cancer Incidence and Mortality (ACIM) books. Available online: http://www.aihw.gov.au/acim-books
- DellaCroce FJ, Wolfe ET. Breast reconstruction. Surg Clin North Am 2013;93:445-54. [PubMed]
- Asplund O, Körlof B. Late results following mastectomy for cancer and breast reconstruction. Scand J Plast Reconstr Surg 1984;18:221-5. [PubMed]
- Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg 2013;131:15-23. [PubMed]
- Albornoz CR, Cordeiro PG, Pusic AL, et al. Diminishing relative contraindications for immediate breast reconstruction: a multicenter study. J Am Coll Surg 2014;219:788-95. [PubMed]
- Radovan C. Breast reconstruction after mastectomy using the temporary expander. Plast Reconstr Surg 1982;69:195-208. [PubMed]
- Elliott LF, Hartrampf CR Jr. Breast reconstruction: progress in the past decade. World J Surg 1990;14:763-75. [PubMed]
- Hershman DL, Richards CA, Kalinsky K, et al. Influence of health insurance, hospital factors and physician volume on receipt of immediate post-mastectomy reconstruction in women with invasive and non-invasive breast cancer. Breast Cancer Res Treat 2012;136:535-45. [PubMed]
- Reaby LL. Reasons why women who have mastectomy decide to have or not to have breast recon-struction. Plast Reconstr Surg 1998;101:1810-8. [PubMed]
- Ng SK, Hare RM, Kuang RJ, et al. Breast reconstruction post mastectomy: patient satisfaction and decision making. Ann Plast Surg 2014. [Epub ahead of print]. [PubMed]
- Walton L, Ommen K, Audisio RA. Breast reconstruction in elderly women breast cancer: a review. Cancer Treat Rev 2011;37:353-7. [PubMed]
- Snell L, McCarthy C, Klassen A, et al. Clarifying the expectations of patients undergoing implant breast reconstruction: a qualitative study. Plast Reconstr Surg 2010;126:1825-30. [PubMed]
- Salhab M, Al Sarakbi W, Joseph A, et al. Skin-sparing mastectomy and immediate breast reconstruction: patient satisfaction and clinical outcome. Int J Clin Oncol 2006;11:51-4. [PubMed]
- Kronowitz SJ, Kuerer HM. Advances and surgical decision-making for breast reconstruction. Cancer 2006;107:893-907. [PubMed]
- Racano C, Fania PL, Motta GB, et al. Immediate and delayed two-stage post-mastectomy breast recon-struction with implants. Our experience of general surgeons. Minerva Chir 2002;57:135-49. [PubMed]
- Kim SW, Lee HK, Kang SM, et al. Short-term outcomes of immediate breast reconstruction using an implant or tissue expander after mastectomy in breast cancer patients. Breast Cancer 2014. [Epub ahead of print]. [PubMed]
- Roostaeian J, Sanchez I, Vardanian A, et al. Comparison of immediate implant placement versus the staged tissue expander technique in breast reconstruction Plast Reconstr Surg 2012;129:909e-18e. [PubMed]
- Chang LY, Hargreaves W, Segara D, et al. Experience in dermomyofascial pouch coverage of imme-diate implants following skin sparing reduction mastectomy. ANZ J Surg 2013;83:135-8. [PubMed]
- Robertson S, Wengström Y, Eriksen C, et al. Breast surgeons performing immediate breast reconstruc-tion with implants - assessment of resource-use and patient-reported outcome measures. Breast 2012;21:590-6. [PubMed]
- Gibney J. Use of a permanent tissue expander for breast reconstruction. Plast Reconstr Surg 1989;84:607-17; discussion 618-20. [PubMed]
- Davila AA, Mioton LM, Chow G, et al. Immediate two-stage tissue expander breast reconstruction compared with one-stage permanent implant breast reconstruction: a multi-institutional comparison of short-term complications. J Plast Surg Hand Surg 2013;47:344-9. [PubMed]
- Roostaeian J, Pavone L, Da Lio A, et al. Immediate placement of implants in breast reconstruction: patients selection and outcomes. Plast Reconstr Surg 2011;127:1407-16. [PubMed]
- Spear SL, Spittler CJ, et al. Breast reconstruction with implants and expanders. Plast Reconstr Surg 2001;107:177-87. [PubMed]
- Hodgson EL, Malata CM. Implant-based breast reconstruction following mastectomy. Breast Dis 2002;16:47-63. [PubMed]
- Argenta LC. Controlled tissue expansion in reconstructive surgery. Br J Plast Surg 1984;37:520-9. [PubMed]
- Kronowitz SJ. State of the art and science in postmastectomy breast reconstruction. Plast Reconstr Surg 2015;135:755e-71e. [PubMed]
- August DA, Wilkins E, Rea T. Breast reconstruction in older women. Surgery 1994;115:663-8. [PubMed]
- Gabriel SE, Woods JE, O'Fallon WM, et al. Complications leading to surgery after breast implantation. N Engl J Med 1997;336:677-82. [PubMed]
- Tsoi B, Ziolkowski NI, Thoma A, et al. Safety of tissue expander/implant versus autologous abdominal tissue breast reconstruction in postmastectomy breast cancer patients: a systematic review and meta-analysis. Plast Reconstr Surg 2014;133:234-49. [PubMed]
- Davies K, Allan L, Roblin P, et al. Factors affecting post-operative complications following skin spar-ing mastectomy with immediate breast reconstruction. Breast 2011;20:21-5. [PubMed]
- Bailey MH, Smith JW, Casas L, et al. Immediate breast reconstruction: reducing the risks. Plast Reconstr Surg 1989;83:845-51. [PubMed]
- Miller AP, Falcone RE. Breast reconstruction: systemic factors influencing local complications. Ann Plast Surg 1991;27:115-20. [PubMed]
- Cowen D, Gross E, Rouannet P, et al. Immediate post-mastectomy breast reconstruction followed by radiotherapy: risk factors for complications. Breast Cancer Res Treat 2010;121:627-34. [PubMed]
- Krueger EA, Wilkins EG, Strawderman M, et al. Complications and patient satisfaction following ex-pander/implant breast reconstruction with and without radiotherapy. Int J Radiat Oncol Biol Phys 2001;49:713-21. [PubMed]
- Embrey M, Adams EE, Cunningham B, et al. A review of the literature on the etiology of capsular contracture and a pilot study to determine the outcome of capsular contracture interventions. Aesthetic Plast Surg 1999;23:197-206. [PubMed]
- Cordeiro PG, McCarthy CM. A single surgeon’s 12-year experience with tissue expander/implant breast reconstruction: part II. An analysis of long-term complications, aesthetic outcomes, and patient satis-faction. Plast Reconstr Surg 2006;118:832-9. [PubMed]
- Holmes JD. Capsular contracture after breast reconstruction with tissue expansion. Br J Plast Surg 1989;42:591-4. [PubMed]
- Singh N, Reaven NL, Funk SE. Immediate 1-stage vs. tissue expander postmastectomy implant breast reconstructions: a retrospective real-world comparison over 18 months. J Plast Reconstr Aesthet Surg 2012;65:917-23. [PubMed]
- Sullivan SR, Fletcher DR, Isom CD, et al. True incidence of all complications following immediate and delayed breast reconstruction. Plast Reconstr Surg 2008;122:19-28. [PubMed]
- Collis N, Coleman D, Foo IT, et al. Ten-year review of a prospective randomized controlled trial of textured versus smooth subglandular silicone gel breast implants. Plast Reconstr Surg 2000;106:786-91. [PubMed]
- Pinsolle V, Grinfeder C, Mathoulin-Pelissier S, et al. Complications analysis of 266 immediate breast reconstructions. J Plast Reconstr Aesthet Surg 2006;59:1017-24. [PubMed]
- Virden CP, Dobke MK, Stein P, et al. Subclinical infection of the silicone breast implant surface as a possible cause of capsular contracture. Aesthetic Plast Surg 1992;16:173-9. [PubMed]
- Patani N, Devalia H, Anderson A, et al. Oncological safety and patient satisfaction with skin-sparing mastectomy and immediate breast reconstruction. Surg Oncol 2008;17:97-105. [PubMed]
- Ringberg A, Tengrup I, Aspegren K, et al. Immediate breast reconstruction after mastectomy for can-cer. Eur J Surg Oncol 1999;25:470-6. [PubMed]
- Rheingold LM, Yoo RP, Courtiss EH. Experience with 326 inflatable breast implants. Plast Reconstr Surg 1994;93:118-22. [PubMed]
- Gylbert L, Asplund O, Jurell G. Capsular contracture after breast reconstruction with silicone-gel and saline-filled implants: a 6-year follow-up. Plast Reconstr Surg 1990;85:373-7. [PubMed]
- Macadam SA, Ho AL, Cook EF Jr, et al. Patient satisfaction and health-related quality of life follow-ing breast reconstruction: patient-reported outcomes among saline and silicone implant recipients. Plast Reconstr Surg 2010;125:761-71. [PubMed]
- McCarthy CM, Klassen AF, Cano SJ, et al. Patient satisfaction with post-mastectomy breast recon-struction: a comparison of saline and silicone implants. Cancer 2010;116:5584-91. [PubMed]
- Schusterman MA, Kroll SS, Reece GP, et al. Incidence of autoimmune disease in patients after breast reconstruction with silicone gel implants versus autogenous tissue: a preliminary report. Ann Plast Surg 1993;31:1-6. [PubMed]
- Spear SL, Onyewu C. Staged breast reconstruction with saline-filled implants in the irradiated breast: recent trends and therapeutic implications. Plast Reconstr Surg 2000;105:930-42. [PubMed]
- Hardwicke J, Gaze NR, Laitung JK. A retrospective audit of Novagold “hydrogel” breast implants. J Plast Reconstr Aesthet Surg 2007;60:1313-6. [PubMed]
- Macadam SA, Ho AL, Lennox PA, et al. Patient-reported satisfaction and health-related quality of life following breast reconstruction: a comparison of shaped cohesive gel and round cohesive gel implant recip-ients. Plast Reconstr Surg 2013;131:431-41. [PubMed]
- Brown MH, Shenker R, Silver SA. Cohesive silicone gel breast implants in aesthetic and reconstructive breast surgery. Plast Reconstr Surg 2005;116:768-79; discussion 780-1. [PubMed]
- Nahabedian MY. Shaped versus round implants for breast reconstruction: indications and outcomes. Plast Reconstr Surg Glob Open 2014;2:e116. [PubMed]
- Liu X, Zhou L, Pan F, et al. Comparison of the postoperative incidence rate of capsular contracture among different breast implants: a cumulative meta-analysis. PLoS One 2015;10:e0116071. [PubMed]
- Shapiro MA. Smooth vs. rough: an 8-year survey of mammary prostheses. Plast Reconstr Surg 1989;84:449-57. [PubMed]
- Hakelius L, Ohlsén L. A clinical comparison of the tendency to capsular contracture between smooth and textured gel-filled silicone mammary implants. Plast Reconstr Surg 1992;90:247-54. [PubMed]
- Handel N, Cordray T, Gutierrez J, et al. A long-term study of outcomes, complications, and patient satisfaction with breast implants. Plast Reconstr Surg 2006;117:757-67; discussion 768-72. [PubMed]
- Maxwell GP, Falcone PA. Eighty-four consecutive breast reconstructions using a textured silicone tis-sue expander. Plast Reconstr Surg 1992;89:1022-34; discussion 1035-6. [PubMed]
- Chew BK, Yip C, Malyon AD, et al. Becker expander implants: truly a long term single stage recon-struction? J Plast Reconstr Aesthet Surg 2010;63:1300-4. [PubMed]
- Spear SL, Majidian A. Immediate breast reconstruction in two stages using textured, integrated-valve tissue expanders and breast implants: a retrospective review of 171 consecutive breast reconstructions from 1989 to 1996. Plast Reconstr Surg 1998;101:53-63. [PubMed]
- Yanko-Arzi R, Cohen MJ, Braunstein R, et al. Breast reconstruction: complication rate and tissue ex-pander type. Aesthetic Plast Surg 2009;33:489-96. [PubMed]
- Kronowitz SJ, Hunt KK, Kuerer HM, et al. Delayed-immediate breast reconstruction. Plast Reconstr Surg 2004;113:1617-28. [PubMed]
- Rosson GD, Shridharani SM, Magarakis M, et al. Quality of life before reconstructive breast surgery: A preoperative comparison of patients with immediate, delayed, and major revision reconstruction. Microsurgery 2013;33:253-8. [PubMed]
- Clough KB, O'Donoghue JM, Fitoussi AD, et al. Prospective evaluation of late cosmetic results fol-lowing breast reconstruction: I. Implant reconstruction. Plast Reconstr Surg 2001;107:1702-9. [PubMed]
- Radovanovic Z, Radovanovic D, Golubovic A, et al. Early complications after nipple-sparing mastec-tomy and immediate breast reconstruction with silicone prosthesis: results of 214 procedures. Scand J Surg 2010;99:115-8. [PubMed]
- Francel TJ, Ryan JJ, Manson PN. Breast reconstruction utilizing implants: a local experience and comparison of three techniques. Plast Reconstr Surg 1993;92:786-94. [PubMed]
- Singh NK, Reaven NL, Funk SE. Cost comparison of immediate one-stage and tissue-expander breast reconstructions after mastectomy in commercially insured patients. Manag Care 2013;22:36-43. [PubMed]
- Giacalone PL, Rathat G, Daures JP, et al. New concept for immediate breast reconstruction for inva-sive cancers: feasibility, oncological safety and esthetic outcome of post-neoadjuvant therapy immediate breast reconstruction versus delayed breast reconstruction: a prospective pilot study. Breast Cancer Res Treat 2010;122:439-51. [PubMed]
- Fodor J, Gulyás G, Polgár C, et al. Radiotherapy and breast reconstruction: the issue of compatibility. Orv Hetil 2003;144:549-55. [PubMed]
- Alderman AK, Wilkins EG, Kim HM, et al. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg 2002;109:2265-74. [PubMed]
- Chen SA, Hiley C, Nickleach D, et al. Breast reconstruction and post-mastectomy radiation practice. Radiat Oncol 2013;8:45. [PubMed]
- Kuske RR, Schuster R, Klein E, et al. Radiotherapy and breast reconstruction: clinical results and do-simetry. Int J Radiat Oncol Biol Phys 1991;21:339-46. [PubMed]
- Lentz R, Ng R, Higgins SA, et al. Radiation therapy and expander-implant breast reconstruction: an analysis of timing and comparison of complications. Ann Plast Surg 2013;71:269-73. [PubMed]
- Fodor J, Gulyás G, Polgár C, et al. Radiotherapy and delayed breast reconstruction with implant: ex-amination of compatibility. Magy Onkol 2002;46:323-6. [PubMed]
- Cordeiro PG, Pusic AL, Disa JJ, et al. Irradiation after immediate tissue expander/implant breast re-construction: outcomes, complications, aesthetic results, and satisfaction among 156 patients. Plast Reconstr Surg 2004;113:877-81. [PubMed]
- Rosato RM, Dowden RV. Radiation therapy as a cause of capsular contracture. Ann Plast Surg 1994;32:342-5. [PubMed]
- Parsa AA, Jackowe DJ, Johnson EW, et al. Selection criteria for expander/implant breast reconstruction following radiation therapy. Hawaii Med J 2009;68:66-8. [PubMed]
- Behranwala KA, Dua RS, Ross GM, et al. The influence of radiotherapy on capsule formation and aesthetic outcome after immediate breast reconstruction using biodimensional anatomical expander implants. J Plast Reconstr Aesthet Surg 2006;59:1043-51. [PubMed]
- Rusby JE, Waters RA, Nightingale PG, et al. Immediate breast reconstruction after mastectomy: what are the long-term prospects? Ann R Coll Surg Engl 2010;92:193-7. [PubMed]
- Losken A, Carlson GW, Schoemann MB, et al. Factors that influence the completion of breast recon-struction. Ann Plast Surg 2004;52:258-61; discussion 262. [PubMed]
- Wong JS, Ho AY, Kaelin CM, et al. Incidence of major corrective surgery after post-mastectomy breast reconstruction and radiation therapy. Breast J 2008;14:49-54. [PubMed]
- Chang DW, Barnea Y, Robb GL. Effects of an autologous flap combined with an implant for breast reconstruction: an evaluation of 1000 consecutive reconstructions of previously irradiated breasts. Plast Reconstr Surg 2008;122:356-62. [PubMed]
- Jugenburg M, Disa JJ, Pusic AL, et al. Impact of radiotherapy on breast reconstruction. Clin Plast Surg 2007;34:29-37. abstract v-vi. [PubMed]
- Albornoz CR, Matros E, McCarthy CM, et al. Implant breast reconstruction and radiation: a multicen-ter analysis of long-term health-related quality of life and satisfaction. Ann Surg Oncol 2014;21:2159-64. [PubMed]
- Klit A, Mejdahl MK, Gärtner R, et al. Breast reconstruction with an expander prosthesis following mastectomy does not cause additional persistent pain: a nationwide cross-sectional study. J Plast Reconstr Aesthet Surg 2013;66:1652-8. [PubMed]
- Corsten LA, Suduikis SV, Donegan WL. Patient satisfaction with breast reconstruction. Wis Med J 1992;91:125-6, 129. [PubMed]
- Baker RR. The management of breast cancer with immediate or delayed reconstruction. Adv Surg 1992;25:51-64. [PubMed]
- Jahkola T, Asko-Seljavaara S, von Smitten K. Immediate breast reconstruction. Scand J Surg 2003;92:249-56. [PubMed]
- Jónsdóttir K, Rafnsdóttir SL, Kjartansdottir T, et al. Results of immediate breast reconstructions at Landspítali-The National University Hospital of Iceland, in 2008-2010. Laeknabladid 2012;98:459-63. [PubMed]