Risk-reducing, conservative mastectomy—analysis of surgical outcome and quality of life in 272 implant-based reconstructions using TiLoop® Bra versus autologous corial flaps
Introduction
Breast cancer requires mastectomy in—at least—one out of four women, and the possibility to prevent breast cancer in families with known genetic inheritance by prophylactic surgery increases the demand for this procedure (1,2). If breast conservation (BCT) is not an option, the question arises which type of mastectomy shall be applied. The evolution of surgical techniques for removal of the mammary gland started from Rotter-Halsteds’ radical mastectomy (3) to Patey’s modified mastectomy (4) of the last millenium up to modern concepts with preservation of the skin envelope by skin-sparing mastectomy (SSM), subcutaneous mastectomy (SCM) or nipple-(areola) sparing mastectomy (NSM/NASM) which are considered as oncologically safe (5). Different approaches and incision patterns have been developed for these surgical procedures such as tennis-racket incision pattern, reduction mammaplasty technique as inverted T- or J-incision, up to total or partial periareolar incision. These techniques have been applied mostly according to the surgeons’ preference. The patients’ perspective was not always in the primary focus. BRCA-mutational status has attracted much attention in the last years when individuals of public interest submitted themselves to prophylactic mastectomy in cases of a positive BRCA1/2-mutational status (1). We investigated the patient’s view on these procedures with validated measurements of quality of life (QoL) and explored the surgical safety and acceptance of these surgical procedures.
Patients and methods
A consecutive cohort of a prospectively maintained database in a single-institution experience at European Breast Center Düsseldorf was analyzed for this study. All patients were eligible who were treated with an immediate implant-reconstruction after mastectomy for prophylactic and therapeutic indications between 2000 and 2014. Inclusion criteria were infeasibility of BCT and no necessity of post-mastectomy radiation as by pre-surgical assessment. Exclusion criteria were inflammatory breast cancer, skin infiltration/fixation and previous radiation. All autologous reconstructions were excluded from this study. Data was retrieved from patient charts and multiple detailed questionnaires. We used four validated QoL-questionnaires to evaluate patients reported outcome (PRO) and QoL: EORTC C-30 (6), EORTC B-23 (7), FACT-G (8) and Breast Cancer Treatment Outcome Scale (BCTOS) (9) and also a customized, study-specific questionnaire. Questionnaires were repeatedly sent by regular mail (thrice). We analyzed the surgical outcome with regard to the safety and the complication of the methods, as well as PRO regarding the volume, symmetry and aesthetic result including the evaluation of scars. Early complications were defined as first presentation of sequelae before 6 months after surgery and late complications as occurring beyond 6 months after surgery. In particular, we compared the use of a TiLoop® Bra for coverage of the lower pole of the breast with the coverage of the same region with an autologous corial fat flap. This study was approved by the Institutional Review Board (IRB) and complied with the declaration of Helsinki.
Reconstruction techniques
Reconstruction mode 1: technique developed for normal breast size (non-ptotic)—coverage with a titanized polypropylene mesh (TiLoop® Bra) (Figure 1A-C)
The glandular tissue is removed via a reduction mammaplasty pattern and the Musculus pectoralis (M. pectoralis) major incised at its insertion and with cautious mobilisation of the M. serratus in the lateral part and the titanized mesh is sutured to the edge of the M. pectoralis major to cover the lower pole and wrapped around the implant without attaching it to the chest wall (double-plane).

Reconstruction mode 2: technique developed for hypertrophic and ptotic breasts—coverage with a corial-fat flap (Figure 2A-C)
Initially, when the skin incision is performed in the sense of a reduction mammaplasty (inverted T), the skin of the lower hemisphere of the breast is de-epithelialized and the corium is separated from the glandula. The glandular tissue is removed and the M. pectoralis major incised at its insertion and a subpectoral pouch has been formed with cautious mobilisation of the M. serratus in the lateral part. The corial flap is then sutured to the edge of the M. pectoralis major to cover the lower pole of the implant (double-plane).

Results
We included 217 patients with 272 mastectomies (55 bilateral cases) and immediate breast reconstructions (IBR) in our study. Median follow-up was 3.5 years (range, 0-14 years). SSM was the most frequently performed procedure with 131 patients, whereas SCM was performed in 86 patients. Invasive breast-cancer was the indication for surgery in 106 patients, non-invasive breast cancer (DCIS) in 80 patients, prophylactic indication (BRCA1/2-mutation) in 30 patients and contralateral alignment in 1 patient. Comparing the two groups of coverage of the lower pole of the implant, groups were well balanced with 78 patients with a titanized, polypropylene mesh TiLoop® Bra and 79 cases with a corial fat flap. For evaluation of patient reported outcome, we were able to refer to a final questionnaire response rate of 70%.
Sequelae of surgery
Early complications
Early complications—defined as surgical sequelae occurring before 6 months after surgery—were low in our cohort: We registered 6 scar insufficiencies, 7 infections, 10 seroma, and 17 hematomas with the necessity of a wound revision. Seventeen patients had hypertrophic scars (keloid). A comparably frequent complication was the loss of sensitivity in any part of the breast or dysaesthesia, reported by 78 patients, which was due to skin incisions.
Late complications
Late complications were low in our cohort: 15 patients developed a capsula fibrosis. In none of these cases implant loss occurred. We recorded an implant rotation in three cases which did not necessitate surgery again. Seven patients reported any kind of dislocation of the implant. There was a significant correlation with the occurrence of an implant dislocation and the mode of coverage of the lower pole of the implant: all implant dislocations occurred in the group of corial-fat flaps, and none in the group of TiLoop® Bra meshes (P=0.01).
A rupture of implants was seen in one case only. A removal of implants was necessary in two cases. An exchange of implants was performed in 17 cases. Restrictions of movement were denoted by 22 patients and only six recurrences were seen in this large cohort.
Symmetry
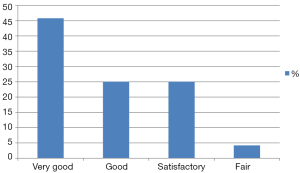
Patients were satisfied with symmetry after both SSM/SCM and immediate reconstruction, eventhough the reconstruction of the contralateral side was eventually performed as a two-point time procedure. As much as 45.8% rated the symmetry as very good, 25% as good and 25% as satisfactory. Thus, almost 96% of patients were satisfied with the symmetric result of the procedure; only 4.2% rated the result as “fair” (Figure 3). Patient reported outcome was best when the procedure was performed bilaterally (P=0.007).
Volume
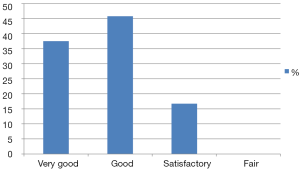
Satisfaction with volume was high with 37.5% rating “very good”, 45.8% as “good” and 16.7% as “satisfactory”. Thus all patients were satisfied with reconstruction volume (Figure 4).
Adhaerence to the decision
All patients in the corial-flap group and all patients in the TiLoop® Bra group considered the operation as the right choice and thus demonstrated adhaerence to the decision for this type of surgery.
Influencing factors on overall asthetic result
We found a significant improvement by use of titanized polypropylen meshes in the aesthetic results (P=0.049) as well as in the prevention of implant dislocation (P=0.009).
Patients with SCM expressed their satisfaction even to a higher extent than those with SSM. This referred particulary to satisfaction with symmetry (P=0.018) and satisfaction with scars (P=0.037).
Of note, genetic screening for BRCA1/2 mutation did not have an impact on partner interaction (P=0.200). Interestingly, radiotherapy—performed in 23 patients—was neither detrimental on cosmetic outcome (P=0.754) nor on body image (P=0.660). Smoking, however, was associated with a significant deterioration of the aesthetic outcome (P=0.007).
Quality of life (QoL) and implant reconstruction mode
QoL was good after both SSM and SCM, and rating of the result was best when the procedure was performed bilaterally. There was no difference in QoL depending on the use of either corial-flap or mesh-reconstruction (P=0.757), also no significant difference in perception of pain after surgery (P=0.237) with either of the two modes of coverage of the lower breast pole, however—as stated above—implant rotation and displacement was less often when meshes were used, which influences QoL strongly.
Discussion
This study provides evidence on the surgical outcome and the patient reported QoL after risk reducing surgery of the breast with SSM and SCM. In our study, we analyzed skin-sparing and subcutaneous mastectomies, all combined with immediate BR and evaluated both the physical as well as the psychological well-being after these surgical procedures. This is of major importance, as the demand for this type of surgery increases. As a recent publication indicated referrals to genetics services showed a rise from May 2013 onwards, with almost 2.5-fold quantity, in a consortium of over 30 UK breast cancer family history clinics and ten more genetics centres, when film actress Angelina Jolie decided to make public that she underwent BRCA testing and subsequent prophylactic mastectomy and salpingo-oophorectomy. This trend was perceived world-wide and is apparently long-lasting (1).
Quality of life (QoL) instruments
To analyze QoL and surgical outcome after these surgical procedures, as much as 272 reconstructions in 217 patients were analyzed retrieving data from patient charts, customized questionnaires and validated instruments of measurement of QoL in our study.
So far, these surgical procedures have not been evaluated with several QoL instruments at a time: We used EORTC C-30 (6), EORTC-BR23 (7), FACT-G (8) and BCTOS (9). These instruments focus on the self-reporting of patients concerning the following items: functional restrictions, disease symptoms, and global perception of QoL. For validation of surgical techniques by patients, BCTOS has been demonstrated to be a reliable instrument for functional and aesthetic assessment (9). Kanatas et al. also described these instruments as validated instruments of measuring QoL specifically for breast cancer patients (10). Furthermore, we developed a study-specific questionnaire which was comparable to similar studies (11,12). The design of our customized questionnaire put emphasis on individually perceived QoL under distress of the risk of breast cancer as well as measurements of surgical outcomes. We were able to retrieve information of these questionnaires by as much as 70% of all patients with three emissions by regular mail.
Breast cancer is a threat to life of patients, and the primary aim of breast cancer therapy is the risk reduction by local and systemic treatment. However, the side effects of either of the therapies affect the physical and psychological well-being of the patients. With views on the surgical therapy, surgeons need to be aware of the best surgical options for their patients and their physical and psychological effects. Physical, psychological and social well-being builds the dimensions of QoL and all three refer to each other (13). Psychological well-being is deteriorated massively by the diagnosis of breast cancer as every individual is confronted with the anticipated risk of mortality. When the probability of survival is higher, aspects of an unimpaired body image regain importance as the breast is a symbol of female identity and sexual attraction. Chen et al. (14) performed a systematic literature review to identify breast-surgery-specific PRO measures and reported significant shortcomings in terms of formal development and psychometric evaluation.
A systematic review conducted by Pusic et al. (15) found that only 1 out of 223 PRO measures used in breast surgery studies had psychometric evidence to support their use in the breast cancer population. The reviews by Chen et al. (14) and Pusic et al. (15) are limited to breast cancer surgery-specific instruments. We included both breast-cancer-surgery specific and general instruments of measurement of QoL.
The techniques analyzed in this study, subcutaneous and SSM and the latter with two different modes of coverage of the lower breast pole were examined with detailed questionnaires.
Patients satisfaction, body image
We detected a high grade of patient satisfaction with volume (99.8%), symmetry (96%) and scars in both forms of mastectomy and immediate reconstruction. Ueda et al. (16) found a smaller cohort of 74 patients that the median score for patient satisfaction including social activity, physical aspects and general condition, were the same in the three groups of BCT, mastectomy and mastectomy with immediate reconstruction. For body image however, BCS and IBR scored higher than with mastectomy only (P<0.05). Ueda’s study group included a scoring by four external reviewers for cosmetic outcome—which we did not apply to our study population to avoid subjective bias—and there was no difference in the estimated cosmetic outcome between BCT and IBR (P=0.20) nor between the SSM and NSM subgroups (P=0.09). Scores referring to pain perception and sexuality were better in the BCT than in the mastectomy group; however there was no difference between BCT and IBR regarding these items.
Adherance to decision and body image after surgery
We focussed primarily on satisfaction and QoL with SCM and SSM, and particularly on the mode of reconstruction of the lower pole of the breast in skin sparing mastectomy, with and without the use of meshes and corial flaps. So far, this item was not analyzed in a direct comparison in literature. All patients of our study expressed their conviction from the aesthetical viewpoint that this type of surgery was the right decision (100% adherance to the decision). The majority of patients rated their satisfaction with symmetry, volume and scars with “good” and “very good”.
We detected a higher satisfaction in patients with reconstructions which were performed bilaterally. Nano et al. (17) analyzed the psychological impact and cosmetic outcome in 123 BR compared with 109 BCT and 78 mastectomies. QoL was similar in all groups, but the BCT group and patients with reconstruction had higher body image scores than patients with a mastectomy. Patient satisfaction was higher in the reconstruction group than the breast conservation group, while aesthetic outcome was similar in both groups. The authors concluded that the high satisfaction and cosmesis scores in the BR group were indicating the superior results that can be achieved with BR.
Corial flap
A study with a lower caseload of 27 patients (34 reconstructions) with mastectomy according to a modified Wise pattern with a tissue expander also used a fasciocutaneous flap for coverage of the lower pole of the breast in women with macromastia while the upper part of the breast was covered by the M. pectoralis major (18). The authors reported a fairly high unplanned re-operation rate of 15%, rate of post-surgical complications of 37%, including seroma of 18% which we did not see in our study. Ladizinsky et al. (19) report on a cohort of 60 patients with a de-epithelialized corial flap with a complication rate of 24% (i.e., skin necrosis, hematoma and infection) and analyzed risk factors for these events and found that overall complications were associated with a body mass index (BMI) greater than 35 (P=0.035) and prior smoking (P=0.0001). The most frequent complication in their study was mastectomy flap skin necrosis (30%). This correlated with placement of a permanent implant (P=0.029) and any history of smoking (P=0.0001). Skin necrosis led to implant loss in 1.2% in their study. In our study, we did not detect a correlation between implant loss and BMI (P=0.262) or history of smoking (P=0.363), however we detected that a higher BMI was a predictor for skin dehiscence (without implant loss) (P=0.043) whereas smoking exerted a negative impact on aesthetic outcome (P=0.007).
TiLoop® Bra
A recent study with a smaller cohort of 34 TiLoop® Bra meshes in the submuscular pocket than in our study compared this surgical approach with 39 TiLoop® Bra meshes with a prepectoral use (20). In their cohort, complications were very low, with two skin flap infections and one wound dehiscence only. No implant loss was recorded. The study group found that TiLoop® Bra was safe and effective in a short-term analysis, both for a retropectoral and a totally subcutaneous implant placement. Contrary to our study, follow-up of this study however was short with 13 months (range, 3-27 months) in the group of TiLoop® Bra mesh, whereas our study had a longer follow-up 3.5 years (range, 0-13 years). Also, inclusion criteria were strict in this study with normal BMI, no large and very ptotic breasts, no history of smoking, no diabetes, and no previous radiotherapy. In our study, we included all patients of any BMI, with large and ptotic breasts, smokers and patients with diabetes, however radiotherapy was allowed after, but also not before surgery. On this background, complication rates were low with no implant loss in the TiLoop® Bra group and only 7 infections, 6 scar insufficiencies, 10 seroma and 17 hematomas in this large cohort of 272 reconstructions. Casella’s study did not report on dysaesthesia which we recorded in our study: 78 patients declared to have experienced these sequelae.
Limitations of our study were that we did not randomize patients to each of the modes of reconstruction—like almost all other studies related to breast surgery—but used size and ptosis as criteria to choose the respective method. Questionnaires were sent to the patients by our own institution, however participation was voluntarily and patients were already discharged from hospital and no influence was exerted on the patients.
Conclusions
In our study, we saw the highest scores for aesthetic results in patient reported outcome with the use of titanized polypropylene meshes (TiLoop® Bra) compared with corial flap which was significantly differing. QoL in general was good in both modes of reconstruction and coverage of the lower breast pole.
We found a significant improvement by use of titanized polypropylen meshes in the aesthetic results as well as in the prevention of implant dislocation. All patients expressed their adherence to the decision for this type of surgery, with highest score with SCM, particularly to satisfaction with symmetry with scars.
Genetic screening for BRCA1/2 mutation did not have an impact on partner interaction and radiotherapy was neither detrimental on cosmetic outcome nor on body image. Smoking, however, was associated with a significant deterioration of the aesthetic outcome.
Dual-plane reconstruction with TiLoop® Bra in normal breasts size and corial flaps in ptotic breasts produces stable results with low complication rates and high levels of QoL in conservative mastectomies.
Acknowledgements
The authors are grateful to all patients participating in this study. The authors thank Hildegard Lax at Institute of Medical Informatics, Biometry and Epidemiology at University of Duisburg-Essen—Director, Prof. Dr. Karl-Heinz Jöckel—for statistical advice and data analysis.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Evans DG, Barwell J, Eccles DM, et al. The Angelina Jolie effect: how high celebrity profile can have a major impact on provision of cancer related services. Breast Cancer Res 2014;16:442. [PubMed]
- Kwok AC, Goodwin IA, Ying J, et al. National trends and complication rates after bilateral mastectomy and immediate breast reconstruction from 2005 to 2012. Am J Surg 2015;210:512-6. [PubMed]
- Halsted WS. The Results of Operations for the Cure of Cancer of the Breast Performed at the Johns Hopkins Hospital from June, 1889, to January, 1894. Ann Surg 1894;20:497-555. [PubMed]
- Patey DH, Dyson WH. The prognosis of carcinoma of the breast in relation to the type of operation performed. Br J Cancer 1948;2:7-13. [PubMed]
- Carlson GW, Bostwick J 3rd, Styblo TM, et al. Skin-sparing mastectomy. Oncologic and reconstructive considerations. Ann Surg 1997;225:570-5; discussion 575-8. [PubMed]
- Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85:365-76. [PubMed]
- Sprangers MA, Groenvold M, Arraras JI, et al. The European Organization for Research and Treatment of Cancer breast cancer-specific quality-of-life questionnaire module: first results from a three-country field study. J Clin Oncol 1996;14:2756-68. [PubMed]
- Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol 1993;11:570-9. [PubMed]
- Stanton AL, Krishnan L, Collins CA. Form or function? Part 1. Subjective cosmetic and functional correlates of quality of life in women treated with breast-conserving surgical procedures and radiotherapy. Cancer 2001;91:2273-81. [PubMed]
- Kanatas A, Velikova G, Roe B, et al. Patient-reported outcomes in breast oncology: a review of validated outcome instruments. Tumori 2012;98:678-88. [PubMed]
- Brandberg Y, Malm M, Blomqvist L. A prospective and randomized study, “SVEA,” comparing effects of three methods for delayed breast reconstruction on quality of life, patient-defined problem areas of life, and cosmetic result. Plast Reconstr Surg 2000;105:66-74; discussion 75-6.[PubMed]
- Curran D, van Dongen JP, Aaronson NK, et al. Quality of life of early-stage breast cancer patients treated with radical mastectomy or breast-conserving procedures: results of EORTC Trial 10801. The European Organization for Research and Treatment of Cancer (EORTC), Breast Cancer Co-operative Group (BCCG). Eur J Cancer 1998;34:307-14. [PubMed]
- Dorfmüller M, Dietzfelbinger H. Psychoonkologie. München: Urban & Fischer, 2009.
- Chen CM, Cano SJ, Klassen AF, et al. Measuring quality of life in oncologic breast surgery: a systematic review of patient-reported outcome measures. Breast J 2010;16:587-97. [PubMed]
- Pusic AL, Chen CM, Cano S, et al. Measuring quality of life in cosmetic and reconstructive breast surgery: a systematic review of patient-reported outcomes instruments. Plast Reconstr Surg 2007;120:823-37; discussion 838-9. [PubMed]
- Ueda S, Tamaki Y, Yano K, et al. Cosmetic outcome and patient satisfaction after skin-sparing mastectomy for breast cancer with immediate reconstruction of the breast. Surgery 2008;143:414-25. [PubMed]
- Nano MT, Gill PG, Kollias J, et al. Psychological impact and cosmetic outcome of surgical breast cancer strategies. ANZ J Surg 2005;75:940-7. [PubMed]
- Losken A, Collins BA, Carlson GW. Dual-plane prosthetic reconstruction using the modified wise pattern mastectomy and fasciocutaneous flap in women with macromastia. Plast Reconstr Surg 2010;126:731-8. [PubMed]
- Ladizinsky DA, Sandholm PH, Jewett ST, et al. Breast reconstruction with the Bostwick autoderm technique. Plast Reconstr Surg 2013;132:261-70. [PubMed]
- Casella D, Bernini M, Bencini L, et al. TiLoop® Bra mesh used for immediate breast reconstruction: comparison of retropectoral and subcutaneous implant placement in a prospective single-institution series. Eur J Plast Surg 2014;37:599-604. [PubMed]