Video-assisted surgery for thyroid cancer patients
Introduction
In the early phase of endoscopic surgery of the neck only benign diseases seemed to be viable for such an approach, in particular as far as thyroid and parathyroid glands were concerned. In fact the first endoscopic endocrinological operation in the neck was a parathyroidectomy (1) for a parathyroid hyperplasia. Likewise all the endoscopic accesses proposed for thyroid, either in the cervical area (2) or in an extra cervical region (3) implied the presence of a benign disease. Only few years later it was stated in some studies that an endoscopic thyroidectomy could reach the same level of completeness as a conventional operation (4). These studies encouraged many authors to use this access, in particular the minimally invasive video assisted thyroidectomy (MIVAT) to treat malignant thyroid tumors, at least low or intermediate risk differentiated carcinomas (5,6). In particular one of these studies clearly shows that in a prospective randomized controlled study it was demonstrated beyond any doubt that for these papillary carcinomas MIVAT had the same outcome as conventional surgery in terms of lymph-node recurrence after an adequate follow-up period. Certainly it is obvious that the demonstration of a similar mortality rate would necessitates of many more years of follow-up, but the 5-year follow-up which characterizes this study can be considered exhaustive in terms of lymph node recurrence and this was the conclusion of the paper: no statistically significant difference between patients that had undergone a MIVAT vs. patients that had undergone a conventional thyroidectomy.
Material and methods
We have been using MIVAT as our favorite minimally invasive access to thyroid diseases from the late nineties (2), at least until we started our experience also with robot via the axillary approach in 2013.
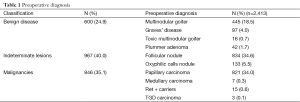
Our experience with MIVAT is represented by 2,413 cases between 1998 and 2014: one of the main indications was low risk papillary carcinoma, but another significant indication was Thy3 or undetermined follicular nodules.
In particular 821 patients were operated with a total thyroidectomy for a papillary carcinoma (34.0%), seven patients (0.3%) were affected by medullary carcinoma, all those cases were clinically negative (no suspicious lymph nodes at preoperative US examination) and were diagnosed by means of routine calcitonin blood measurement, 15 patients were RET + carriers (0.6%) who underwent prophylactic thyroidectomy and three patients were affected by TGD carcinoma, all of those diagnosed as incidentally specimen findings.
Furthermore 967 patients underwent a MVAT for the presence of an undetermined lesion (40.0%) (Table 1). Of course only a small percentage of the latter proved to be carcinomas (mainly papillary) at final histology, but if we consider these two groups as malignant or potentially malignant patients we must conclude that almost ¾ of the cases of MIVAT are carried out in patients that do not show a benign disease.
Full table
We could say that this is an operation that, moving from its prudential onset, has today a very clear indication for malignancies.
Results
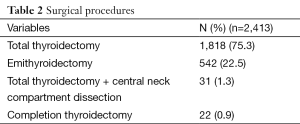
In only 22 patients we had to go back for a completion thyroidectomy after final histology: this happened in patients that had undergone a lobectomy for a follicular nodule or hurtle cells nodule referred as Thy3 lesions which had turned out to be a follicular variant of papillary carcinoma (FVPC). We operated via the same central access and repeating a MIVAT in all cases. The conversion rate was very low: 24 patients (1.0%), mainly due to: unexpected posterior tracheal invasions (nine patients), involvement of lymph nodes not evident at echography (four patients), esophageal infiltration (three patients), strap muscles infiltration (three patients) and finally in five cases the presence of serious thyroiditis that had escaped to ultrasonographic evaluation.
In 31 cases a central compartment clearance was associated to total thyroidectomy (3.9%) (Table 2).
Full table
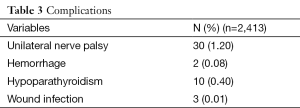
The mean duration of the operation was 41 minutes. The main complication is represented by unilateral recurrent laryngeal nerve palsy (1.2%) discovered by postoperative direct laryngoscopy performed for each patient with no regard to dysphonia. Surprisingly the definitive hypoparathyroidism, assessed when six months postoperative PTH value and serum calcemia were less than 13 pg/mL and 8.0 mg/dL respectively, was very low in the series (0.4%). Both wound infection and hemorrhage showed very low rate (respectively: 0.01% and 0.08%) (Table 3).
Full table
Mean hospital stay was 1.5 days after the operation, but in the last 1,300 cases patients are discharged on first post operative day.
Discussion
It can be assumed that, although MIVAT still represents an ideal indication for the simplest cases, in particular for small thyroids (7-9), and benign diseases more easily reflect this situation (9), malignancies are now currently treated via MIVAT as our series and others’ papers (10) clearly show. This change was certainly driven by the sound demonstration of the oncologic completeness of the operation (5), but was also implemented by the excellent post operative results: the reasonable rate of recurrent nerve palsy and the very low incidence of hypoparathyroidism (Table 3) have done the operation attractive for many surgeons also in USA (7). These data are not surprising when considering that, among the inclusion criteria for MIVAT, the nodule, the gland size and the absence of clear lymph node involvement are an important limit: so only T2N0 patients are enrolled for this operation: as a consequence dissection and preservation of parathyroid and recurrent nerve turned out to be simpler and more successful than in more advanced cases. Basically we prefer not to treat via MIVAT patients with an evident involvement of lymph nodes, but when necessary, as it can be seen in Table 2, a central compartment clearance is always possible.
The conversion rate is certainly very low: 1% of all cancers (Table 3) and basically it reflects the limits of pre-operative ultrasonography: in fact all the underscored diagnoses which provoked the conversion to open surgery can be considered as echography drawbacks.
Finally the more favorable post operative course which characterizes the operation (11), in particular in terms of post operative distress offers the possibility of discharging most of the patients on the same day of surgery, as widely practiced in USA (12), unlike our cohort where we had to keep patients hospitalized for at least one night, by law.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg 1996;83:875. [PubMed]
- Miccoli P, Berti P, Conte M, et al. Minimally invasive surgery for thyroid small nodules: preliminary report. J Endocrinol Invest 1999;22:849-51. [PubMed]
- Ikeda Y, Takami H, Niimi M, et al. Endoscopic thyroidectomy by the axillary approach. Surg Endosc 2001;15:1362-4. [PubMed]
- Miccoli P, Elisei R, Materazzi G, et al. Minimally invasive video-assisted thyroidectomy for papillary carcinoma: a prospective study of its completeness. Surgery 2002;132:1070-3. [PubMed]
- Miccoli P, Pinchera A, Materazzi G, et al. Surgical treatment of low- and intermediate-risk papillary thyroid cancer with minimally invasive video-assisted thyroidectomy. J Clin Endocrinol Metab 2009;94:1618-22. [PubMed]
- Lombardi CP, Raffaelli M, De Crea C, et al. Video-assisted versus conventional total thyroidectomy and central compartment neck dissection for papillary thyroid carcinoma. World J Surg 2012;36:1225-30. [PubMed]
- Terris DJ, Angelos P, Steward DL, et al. Minimally invasive video-assisted thyroidectomy: a multi-institutional North American experience. Arch Otolaryngol Head Neck Surg 2008;134:81-4. [PubMed]
- Liu J, Song T, Xu M. Minimally invasive video-assisted versus conventional open thyroidectomy: a systematic review of available data. Surg Today 2012;42:848-56. [PubMed]
- Miccoli P, Minuto MN, Ugolini C, et al. Minimally invasive video-assisted thyroidectomy for benign thyroid disease: an evidence-based review. World J Surg 2008;32:1333-40. [PubMed]
- Lai SY, Walvekar RR, Ferris RL. Minimally invasive video-assisted thyroidectomy: expanded indications and oncologic completeness. Head Neck 2008;30:1403-7. [PubMed]
- Del Rio P, Berti M, Sommaruga L, et al. Pain after minimally invasive videoassisted and after minimally invasive open thyroidectomy--results of a prospective outcome study. Langenbecks Arch Surg 2008;393:271-3. [PubMed]
- Terris DJ, Moister B, Seybt MW, et al. Outpatient thyroid surgery is safe and desirable. Otolaryngol Head Neck Surg 2007;136:556-9. [PubMed]


