Achieving ideal donor site aesthetics with autologous breast reconstruction
Introduction
For many years, the emphasis with autologous breast reconstruction was focused on achieving ideal breast aesthetics. Although this remains of paramount importance, achieving ideal donor site aesthetics has become increasingly important and is now expected by patients. With the introduction of muscle sparing flaps, the ability to maintain the normal dynamics of the donor site are certainly enhanced; however, adverse events can still occur. These may include contour abnormalities, bulge, hernia, muscle weakness, delayed healing, complex scaring, and pain. Because the abdomen is the most commonly used donor site, the manuscript will focus on prevention and management of adverse events related to this donor site to achieve ideal aesthetics.
There are essentially five flaps that are derived from the abdomen that include the pedicle transverse rectus abdominis musculocutaneous (TRAM), free TRAM, muscle sparing free TRAM, deep inferior epigastric perforator (DIEP), and superficial inferior epigastric artery (SIEA) flaps. Each of these flaps has unique characteristics that require special attention during harvest and closure to achieve ideal donor aesthetics. Reinforcement materials will sometimes be necessary; however, it should be remembered that maximal preservation of the natural abdominal anatomy should facilitate obtaining a desirable abdominal contour without the use of reinforcement materials.
The initial evaluation
As with all procedures, patient selection is critical (1). Some patients will be considered high risk for adverse events and less ideal abdominal aesthetics may result. These include patient that are actively using tobacco products, have poorly controlled diabetes mellitus, morbid obesity, and multiple prior operations. With overweight and obese patients, it is important to identify whether the fat is predominantly subcutaneous or intra-abdominal. Subcutaneous fat will lend itself nicely to having enough fat to adequately reconstruct the breast and usually result in improved abdominal aesthetics (Figure 1). Intraabdominal fat usually manifests as a convex anterior abdominal wall that is rarely ideally contoured (Figure 2). It is important to inform patients with a convex abdominal wall that they will most likely remain so postoperatively unless they lose weight before or after surgery.
Patient related factors can affect the aesthetic outcome of the abdomen. Tobacco use and poorly controlled diabetes mellitus will lead to delayed healing, poor scarring, and distortions in abdominal contour. Patients with elevated HbA1C levels (>7) or who are actively using tobacco products are discouraged from proceeding with autologous breast reconstruction because of these risks. Once controlled, the autologous outcomes are generally improved, predictable, and reproducible. Prior abdominal operations can affect the outcome of surgery and impact both the breast and donor site (2-4). Paramedian abdominal incisions can injure vascular perforating vessels, lower transverse incisions can disrupt the superficial and deep inferior epigastric vessels, and multiple abdominal incisions can disrupt the anterior rectus sheath. The effects of these incisions may include an increase in contour abnormalities such as bulge or hernia as well as delayed healing due to compromised perfusion. Prior liposuction can disrupt the perforator system and result in delayed healing or abdominal fat necrosis.
Once patient selection criteria have been established, achieving ideal abdominal aesthetics will be dependent on the type of flap selected, degree of fascial and muscle trauma, and operative technique. Preservation of the rectus abdominis muscle is classified based on subdivision into three vertical segments; medial, central, and lateral (3). Preservation of the entire muscle is classified as an MS-3 (DIEP) flap. Preservation of the medial and lateral segment is classified as an MS-2 (muscle sparing TRAM) flap. Preservation of the lateral or medial segment is classified as an MS-1 (muscle sparing TRAM) flap. Sacrifice of the entire width of the muscle is classified as an MS-0 (TRAM) flap. MS-1, MS-2, and MS-3 flaps preserve the continuity of the rectus abdominis muscle and therefore provide varying degrees of muscle function.
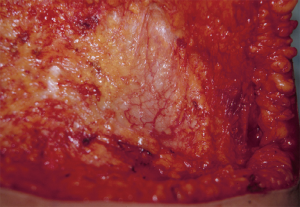
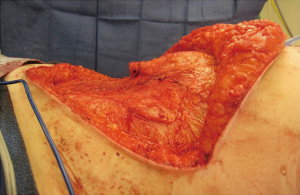
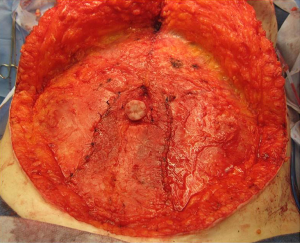
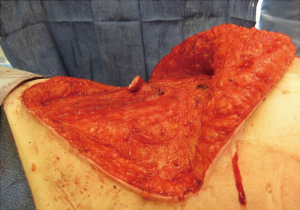
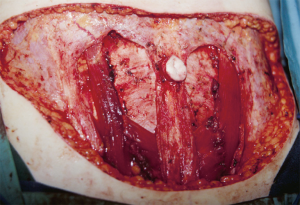
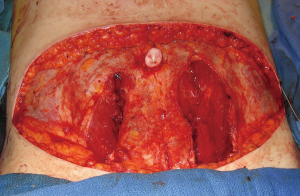
In general, the flaps that violate the integrity of the anterior abdominal least will provide the best outcomes (4). Theoretically, the SIEA flap should provide the best abdominal outcome because the anterior rectus sheath and rectus abdominis muscles are not incised. The DIEP flap requires a fasciotomy and myotomy to dissect out the deep inferior epigastric vessels (Figure 3). The free TRAM utilizes a short segment of the rectus abdominis muscle that can include the full or partial width of the muscle (Figure 4). The pedicle TRAM incorporates the full length of the muscle and either the entire or partial width of it.
The abdominal markings
All abdominal flaps can be designed in a similar fashion in terms of the preoperative markings (Figure 5). The location and dimensions of the flaps are similar and subject to modification based on body habitus and location of scars. Patient are marked standing. The anterior superior iliac spine (ASIS) are palpated and marked. The midline of the abdomen from the xiphoid to the pubic bone is delineated. The proposed upper and lower transverse incisions are delineated and communicated laterally at the ASIS. The final location of the lower transverse incision is determined intraoperatively when the patient is flexed about 30 degrees to ensure that the abdomen can be closed. Sometimes the proposed incision has to be elevated in order to ensure closure. This flap design incorporates the aesthetic units of the abdomen such that the final scar will be positioned as low as possible extending superolaterally towards the ASIS (5).
Operative strategies to achieve ideal abdominal contour
It is important to discuss with patients that performing an abdominal flap is different than a performing a cosmetic abdominoplasty except perhaps in the case of a SIEA flap where the abdominal fascia and muscle remain intact. With the MS—0-3 flaps, that anterior rectus sheath and muscle are violated therefore disrupting the normal anterior abdomen. More often than not, the disruption is beneficial but in some cases it is not and can be a source of consternation. The principles and techniques discussed in the ensuing paragraphs will assist in achieving ideal abdominal contours and characteristics, but it should be emphasized that it will be a different normal than previous.
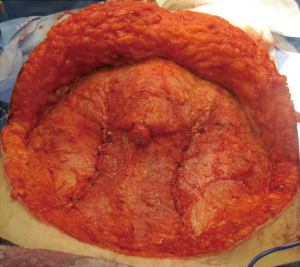
Harvesting the flaps
Following the initial incisions, the dissection proceeds to the anterior rectus sheath. It should be remembered that the anterior rectus sheath is a vascularized lattice of collagen fibers that should be preserved as much as possible (Figure 6). The anterior rectus sheath is comprised of the aponeurosis of the external and internal oblique muscles. There is a loose areolar layer of tissue over the anterior sheath that contains a plexus of vessels that should be preserved to ensure vascularity and viability following the operation. It should be noted that sensory nerves usually pass through the fascia as neurovascular bundles en route to the skin. These nerves should be identified a cut. Clipping these sensory nerves should be avoided to prevent a painful neuroma (6). This has been noted in our practice and therefore use of clips is avoided when possible. Incising the anterior rectus sheath is not without consequence because it disrupts the normal lattice of fibers that is considered one of the primary support systems of the anterior abdominal wall. Under normal circumstances, as intraabdominal pressure increases, the lattice will tighten to maintain contour. With sustained pressure over a long period of time, diastasis recti can develop. For this reason it is important to preserve as much of the sheath as possible and to adequately close all layers of the anterior rectus sheath during the closing phase.
The other important aspect of maintaining the integrity of the anterior abdominal wall is to preserve the lateral innervation of the rectus abdominis muscle (7,8). The rectus muscle is segmentally innervated. The motor nerves typically enter the muscle along its posterior surface at the junction of the lateral and central thirds. When harvesting MS-1, MS-2, or MS-3 flaps, the lateral innervation should be preserved to ensure muscle contractility. Each of these flaps requires a myotomy or segmental excision of muscle. There are crossover motor nerve branches that will be encountered. Sometimes these nerves can be preserved and other times they require division. This should be done sharply without clips to permit axonal sprouting and medial segment neurotization.
Preservation of the recuts abdominis muscle and the anterior rectus sheath will usually improve functional outcomes related to the anterior abdominal wall (7,8). All variations of myotomy or myomectomy of the rectus abdominis will limit the contractility of the muscle because the contractile sarcomeres are replaced by scar. Loss of continuity of the muscle will result in a non-functional muscle; therefore MS-1, MS-2, and MS-3 flaps usually result in improved function as long as the nerves are preserved. Limiting the amount of anterior rectus sheath excision will minimize contour abnormalities of the abdomen (3,4).
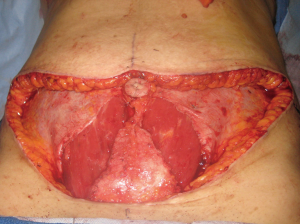
Closing the abdomen
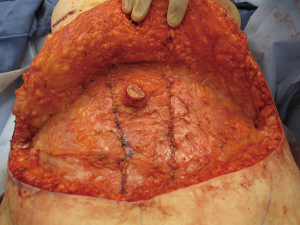
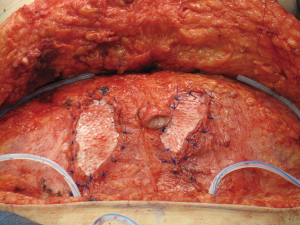
At time of closure, it is important to approximate the medial and lateral segments of muscle when an MS-2 or MS-3 flap has been performed (Figure 7). This will minimize the incidence of lateralization of the muscle as intraabdominal pressure increases. Closure of the anterior rectus sheath is perhaps the most important predictive aspect for outcome quality. When an MS-3 flap has been performed, a standard fascial approximation is typically performed using an absorbable or nonabsorbable monofilament suture placed in an interrupted figure-of-8 fashion. All lamellae of the anterior sheath are closed to ensure stability. A second row of sutures is typically placed in a running, continuous fashion for further reinforcement (Figure 8). When an MS-0, MS-1, or MS-2 flap has been performed, primary fascial closure is usually possible when there is enough laxity or redundancy of the fascia. In situations where it is not, the use of a mesh (biologic or synthetic) is typically necessary (9). The purpose of the mesh is to prevent undue tension on the fascial closure that will have a higher likelihood of dehiscence or attenuation. The mesh can be placed as an inlay (Figure 9) when there is a fascial deficit and as an onlay (Figure 10) when the fascial closure needs additional reinforcement. The type of mesh used can vary from biologic composed of porcine dermis, synthetic of polypropylene, and resorbable collagen. In our experience, the use of a mesh has been necessary in 11.8% of patients (9). Figures 11,12 demonstrate a pre and postoperative image of a woman following bilateral breast reconstruction with abdominal flaps.
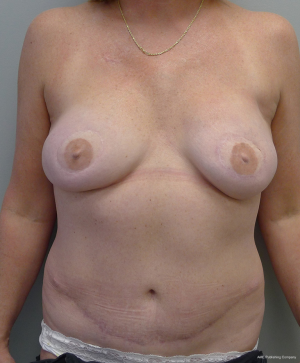
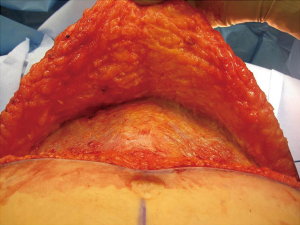
Following fascial closure, plication of the remaining fascia is sometimes necessary to achieve ideal contour (Figures 13-19). With unilateral reconstructions, contralateral plication will serve to achieve uniformity of the anterior abdominal wall and to centralize the umbilicus. With bilateral reconstructions, the supraumbillical fascia is often plicated along the midline to prevent an upper abdominal bulge. These sutures are usually monofilament and placed in a figure-of-8 fashion. Infraumbillical midline sutures are also sometimes useful to achieve ideal contour.


Scarpas fascia in obese women that have abdominal flaps reconstruction is sometimes in excess along the pubic area as well as the upper abdomen. This fat is often less vascularized than the fat above scarpas layer. For this reason, it is sometimes excised. The thickness of the upper and lower adipocutaneous layers of the abdominal wall should be similar to prevent any step-off deformity. The slight depression of the midline anterior abdominal wall can be recreated by excision a few millimeters of fat along the midline of the adipose layer. This maneuver will also tend to provide a more natural abdominal contour.
Skin closure is the final stage of abdominal closure and includes the umbilicus and the incisions. The insetting of the umbilicus is another important step to achieve ideal abdominal aesthetics. Various skin incision patterns are possible that include circular, oval, and “U” designs all of which are capable delivering good results. A technique that has demonstrated success for achieving a natural appearance is the 2-dermal flap umbilical transposition flap technique (10). With this technique, the umbilicus is invaginated to shorten the umbilical stalk and yield a very natural appearance. Skin closure is always performed in three layers that include scarpas fascia, the dermis, and epidermis. Closure of scarpas layer is important to prevent separation of the fat resulting in an involuted scar. Monofilament sutures are used for the dermis and subcuticular layers. Lateral dog-ears should be identified at time of closure and addressed. This will lead to lengthening of the abdominal incision but an improvement in abdominal contour. Two closed suction drains are always used to minimize the occurrence of a fluid collection.
Correcting postoperative abdominal abnormalities
There are several postoperative abnormalities that can be a significant source of patient dissatisfaction that include abdominal bulge, abdominal hernia, persistent pain, delayed healing and chronic fluid collection (11-13). Each of these typically requires operative intervention to correct. The first step is to address the patient concerns by performing a history and physical examination. Areas of abnormal contour, pain, induration, fluid collections and delayed healing are noted.
Abdominal bulge
An abdominal bulge is most often due to attenuation of the anterior rectus sheath and secondarily due to dehiscence of the facial closure but it can be exacerbated by absence, weakness or denervation of the rectus abdominis muscle (4,12). It is important to differentiate between a bulge and hernia. A hernia will have a true facial defect that can be palpated whereas a bulge will not. Imaging studies are usually not necessary with a bulge. The area of the bulge is delineated with the patient standing. During the operation, lower transverse incision is opened and the upper adipocutaneous layer elevated. The bulge is identified and plicated in two vertical layers using a nonabsorbable monofilament suture in a figure-of-8 fashion as well as a continuous suture. The use of a synthetic mesh is usually considered to further reinforce the anterior abdominal wall and typically extends from the costal margin to the pubic region. The sutures are usually absorbable monofilament and placed around the periphery of the mesh and centrally to anchor it to the anterior rectus sheath.
Upper abdominal bulge is sometimes seen with pedicle TRAM flap (3). These flaps can be rotated ipsilaterally or contralaterally to gain access to the breast pocket. As such an upper abdominal fullness may result and be bothersome to some patients. With time many of these bulges will spontaneously resolve as the rectus abdominis muscles atrophies because of denervation. However, when persistent surgical correction is considered, this may include liposuction of the affected area or direct surgical excision. Both maneuvers have demonstrated success.
Abdominal hernia
The repair of a true hernia differs from that of the bulge (7). The initial phase of the repair includes defining the fascial edges of the defect and then excision of the hernia sac. An intra-abdominal approach to the repair is required. Mesh reinforcement is often necessary and can be used as an underlay or onlay fashion. Both synthetic and biologic meshes can be considered. Underlay and onlay mesh should span as much of the anterior abdominal wall as possible. Absorbable monofilament sutures are usually used to anchor the mesh to its surface. The fascial edges are re-approximated when possible using nonabsorbable monofilament sutures in an interrupted figure-of-8 fashion followed by a running continuous suture is placed along the linea alba. In complex situations associated with recurrence and loss of domain, the use of tissue expanders can be considered to repair a true hernia.
Pain
Chronic pain following abdominal flap reconstruction is usually due to a neuroma (6). The usual cause of this is a surgical clip that has been placed along a sensory branch of the intercostal neurovascular bundle as it traverses through the anterior rectus sheath to the adipocutaneous layer. Other etiologies may include entrapment of the ilioinguinal and iliohypogastric nerves. Conservative management is usually recommended for the first 6 months because most of these symptoms are self-limiting. However, when the pain is persistent and interferes with activities of daily living, surgical excision of the neuroma with burial of the nerve stump into the underlying muscle is recommended (6).
Fluid collections
Fluid collections following abdominal flap reconstruction can occur and may be due to premature drain removal, damage to the loose areolar layer of the anterior rectus sheath, and body habitus. Seromas are the most common but a hematoma is also possible. Fortunately many of these are small and self-limiting; however, when large and persistent, intervention is considered. This may include office procedures such as serial aspiration or by placing an indwelling catheter via interventional radiology. Operative evacuation may be considered when refractory to conventional maneuvers.
Conclusions
In summary, achieving ideal abdominal aesthetics following abdominal flap reconstruction is possible using various principles and concepts. Preoperative assessment is important to determine who is at risk for abdominal morbidity. Intraoperatively, it is important to preserve the vascularity of the anterior rectus sheath and minimize its excision. Closure of the anterior sheath can be performed primarily or with the assistance of a surgical mesh. Fascial plication will serve to improve abdominal contours. Preservation of the rectus abdominis muscle and maintenance of its innervation will improve the integrity and function of the anterior abdominal wall. Closure of the incisions, contouring of the scarpas fat, and umbilical transposition are also relevant considerations to achieve ideal abdominal aesthetics.
Acknowledgments
This research meets the ethical guidelines, including adherence to the legal requirements of the study country.
Disclosure: Dr. Nahabedian is a speaker and consultant for LifeCell (Bridgewater, NY, USA) and Allergan (Irvine, CA, USA). No financial or technical assistance was used in preparation of this manuscript.
References
- Nahabedian MY. Breast reconstruction: a review and rationale for patient selection. Plast Reconstr Surg 2009;124:55-62. [PubMed]
- Rozen WM, Garcia-Tutor E, Alonso-Burgos A, et al. The effect of anterior abdominal wall scars on the vascular anatomy of the abdominal wall: A cadaveric and clinical study with clinical implications. Clin Anat 2009;22:815-22. [PubMed]
- Nahabedian MY, Manson PN. Contour abnormalities of the abdomen after transverse rectus abdominis muscle flap breast reconstruction: a multifactorial analysis. Plast Reconstr Surg 2002;109:81-7; discussion 88-90. [PubMed]
- Nahabedian MY, Dooley W, Singh N, et al. Contour abnormalities of the abdomen after breast reconstruction with abdominal flaps: the role of muscle preservation. Plast Reconstr Surg 2002;109:91-101. [PubMed]
- Matarasso A, Wallach SG. Abdominal contour surgery: treating all aesthetic units, including the mons pubis. Aesthet Surg J 2001;21:111-9. [PubMed]
- Rosson GD, Dellon AL. Abdominal wall neuroma pain after breast reconstruction with a transverse abdominal musculocutaneous flap: cause and treatment. Ann Plast Surg 2005;55:330-4. [PubMed]
- Nahabedian MY. Abdominal Wall Considerations Following TRAM and DIEP flaps. In: Nahabedian MY, Bhanot P. eds. Abdominal Wall Reconstruction. Woodbury: CineMed publishing, 2014.
- Nahabedian MY, Momen B, Galdino G, et al. Breast Reconstruction with the free TRAM or DIEP flap: patient selection, choice of flap, and outcome. Plast Reconstr Surg 2002;110:466-75; discussion 476-7. [PubMed]
- Patel KM, Shuck J, Hung R, et al. Reinforcement of the abdominal wall following breast reconstruction with abdominal flaps: a comparison of synthetic and biological mesh. Plast Reconstr Surg 2014;133:700-7. [PubMed]
- Rozen SM, Redett R. The two-dermal-flap umbilical transposition: a natural and aesthetic umbilicus after abdominoplasty. Plast Reconstr Surg 2007;119:2255-62. [PubMed]
- Nahabedian MY. Secondary operations of the anterior abdominal wall following microvascular breast reconstruction with the TRAM and DIEP flaps. Plast Reconstr Surg 2007;120:365-72. [PubMed]
- Nahabedian MY, Momen B. Lower abdominal bulge after deep inferior epigastric perforator flap (DIEP) breast reconstruction. Ann Plast Surg 2005;54:124-9. [PubMed]
- Bajaj AK, Chevray PM, Chang DW. Comparison of donor-site complications and functional outcomes in free muscle-sparing TRAM flap and free DIEP flap breast reconstruction. Plast Reconstr Surg 2006;117:737-46; discussion 747-50. [PubMed]