Dynamic body posture after unilateral mastectomy: a pilot study
Introduction
Improvements in diagnosis and treatment modalities for breast cancer have affected survival, but the rate of complications after treatment has also increased (1). These primarily include pain, fatigue, muscle weakness, lymphedema, psychological problems (e.g., anxiety, depression, insomnia), cognitive impairment, and postural changes (2). Another major postoperative complication is postural changes. However, while it can cause depression and debilitating back pain that can lead to the deterioration of quality of life, the standard diagnostic criteria and treatment modality for postural changes are yet to be established. Previous research showed a higher incidence rate of postural changes after treatment in breast cancer women than their healthy counterparts (82.3% vs. 35.1%) (3). Further, while undesirable postural changes were found in both radical mastectomy and breast-conserving surgery, postural changes were more severe after mastectomy (4).
Modified radical mastectomy (MRM), which involves resection of the whole breast and most axillary lymph nodes, is one of the standard surgical treatments for breast cancer (5). It is mainly performed in cases with metastasis or suspected lymph node involvement. While it has benefits, MRM is also associated with postoperative problems such as lymphedema and musculoskeletal complications (5). For example, compared to normal participants, women who underwent mastectomy were found to have an asymmetry in the trunk and shoulder, and there was forward-leaning of the trunk (6). Further, comparison of body posture between patients with immediate breast reconstruction (IBR) and only mastectomy showed a significant difference in the vertical alignment of the trunk, indicating trunk rotation (7). These results support the idea that postural changes may occur after unilateral mastectomy. However, the results of previous studies on postural changes after unilateral mastectomy are inconsistent, possibly because differences in surgical methods, dominant hand, and postoperative duration influenced body posture and symmetry, thus limiting the measurement of postural changes.
Visual observation is a simple method of measuring postural changes, but it does not provide quantitative data and has poor interrater reliability (8). Meanwhile, photogrammetric and radiographic methods provide relatively objective data in static posture (8), but they cannot measure dynamic postural changes. The balance board system (BBS) with an accelerometer has been reported to provide useful information in idiopathic scoliosis and pelvic deformities and has the advantage of being able to examine in the dynamic state (9). In addition, more accurate information on posture can be obtained by measuring muscle activity of the para-spinal muscles.
This study aimed to investigate the postural changes by inclination angles and muscle activities in the static or dynamic sitting position after mastectomy and validate the usefulness of BBS for evaluating body symmetry and posture. We present the following the article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/gs-20-466).
Methods
Study design
The observational study design was conducted to compare the changes of inclination angle and muscle activities when applied the BBS among women with Rt. MRM, Lt. MRM, and non-breast cancer.
The study protocol was approved by the Institutional Review Board of Chungnam National University Hospital (Approval number: CNUH 2016-10-009-001) and conducted in accordance with the Declaration of Helsinki (as revised in2013). Written informed consent was received from all participants before starting the study.
Participants
This study was conducted at Daejeon Chungcheong Regional Rehabilitation Center, Chungnam National University Hospital, Korea between November 2016 and November 2017.
The participants were women aged 35–55 years who underwent MRM more than 1 year prior. To minimize the potential source of bias in term of inclination angle and muscle activities, the exclusion criteria were bilateral mastectomy; upper-limb lymphedema (over stage II); breast reconstructed state; history of other cancer operation; and orthopedic, rheumatologic, peripheral polyneuropathy, neurological sequela that could affect the spine asymmetry. Potential participants during the period of study were 32, but 15 did not included because of not meeting the inclusion criteria. Therefore, 17 patients were included, and they were divided into the right MRM (Rt. MRM; n=7) and the left MRM (Lt. MRM; n=10) groups according to the sidedness of the mastectomy. All patients were right-handed. In addition, an aged-matched cohort of 8 healthy women were recruited for the non-breast cancer group.
Procedure
The BBS used in this study was a hemispheric unstable board that composed of an accelerometer and photo sensors for measuring the inclination angles of the body in the frontal and sagittal axes (Figure 1) (10). The board had a curvature radius that can be tilted in all directions, creating up to 20° of inclination angle of the pelvis. The upper part of this board was covered with a soft material to accommodate the buttocks. The tilting angle was calculated using the acceleration of gravity.
This study was performed under two conditions: static and dynamic sitting state. In the static sitting posture, participants were instructed to sit in their usual manner on the board, which is located in the middle of stool, with their arms crossed on the contralateral shoulder for 30 seconds. In the dynamic sitting posture, participants were asked to lean the body toward eight directions, namely, the anterior (A), anterior-left (AL), left (L), posterior-left (PL), posterior (P), posterior-right (PR), right (R), and anterior-right (AR) side, using curvature structure of the board. The participants maintained the posture for 5 seconds for each direction. The feet were attached to the ground to avoid the effects of leg movement. Inclination angles were measured in the Rt. MRM, Lt. MRM, and non-breast cancer groups under the two conditions and analyzed at a rate of 100 Hz using LabVIEW 2010 (National Instrument CO., Texas, USA). After explaining all the procedures to the participants before applying, we measured them twice.
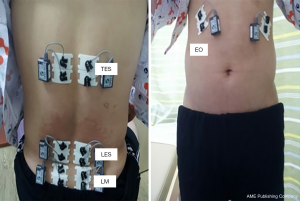
The patterns of muscular activities were recorded using the Noraxson Telemyo 2400T (Noraxson Inc., Scottsdale, USA). Wireless surface electrodes (Noraxson Inc., Scottsdale, USA) were attached to the external oblique (EO) (along the most inferior costal margin), thoracic erector spinae (TES) (5 cm lateral to the T9 spinous process), lumbar erector spinae (LES) (3 cm lateral to the L3 spinous process), and lumbar multifidus (LM) (L5 level) muscles bilaterally (Figure 2). Before placing the electrode, the skin was prepared with alcohol to minimize the skin resistance. To normalize the difference of muscle contraction for individuals, electromyography (EMG) data were expressed as a percentage relative to the maximum voluntary contraction (MVC) (11). In this procedure, participants attempted to flex or extend the upper trunk in the sagittal plane with maximum effort, and then hold it for 5 seconds while the examiner pushed down their shoulders. Total procedure took about 40 minutes for participant.
Statistical analysis
One-way analysis of variance (ANOVA) test and t-test were used to examine the difference in general characteristics, inclination angles, and muscle activities among the 3 or 2 groups. The post hoc test (Scheffe test) was performed when the significance was found in the one-way ANOVA test. If data did not satisfy the normal distribution using the Kolmogorov-Smirnov test and Shapiro-Wilk test, the nonparametric test (Kruskal-Wallis test) was performed. All statistical analyses were performed using IBM SPSS Statistics 24.0 version (SPSS Inc., Chicago, IL, USA). P values <0.05 were considered statistically significant.
Results
Participants’ general characteristics
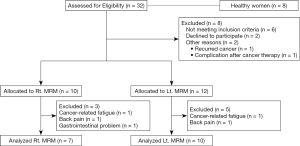
The numbers of potential eligible patients were 32, 6 patients did not satisfy inclusion criteria, 2 were declined to participate, and 2 have other reasons. Of the 22 patients, 10 patients were assigned to the Rt. MRM and 12 patients were allocated to the Lt. MRM, respectively, but 7 in the Rt. MRM and 10 in the Lt. MRM were each participated in finals (Figure 3).
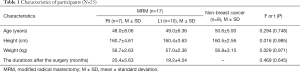
The general characteristics of all participants are shown in Table 1. All participants were right-handed women and mean age was 48.0±8.06 years in the Rt. MRM (n=7), 49.0±6.36 years in the Lt. MRM (n=10), and 50.6±5.93 years in the non-breast cancer (n=8), respectively. In homogeneity testing among three groups, there were no significant differences in age, height, and weight among the three groups. The average duration after surgery was 20.4±5.63 months in the Rt. MRM group and 19.2±4.54 months in the Lt. MRM group.
Full table
Inclination angle and muscle activity
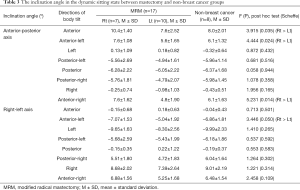
In the non-breast cancer group, the inclination angle was slightly tilted to the posterior and right side in the static sitting posture. Meanwhile, the MRM groups tended to move slightly to the anterior and left side compared with the non-breast cancer group, but the difference was not significant (P>0.05) (Table 2).

Full table
In the dynamic sitting state, when leaning forward (i.e., anterior, anterior-left, and anterior-right directions), the anterior inclination angle was significantly increased in the Rt. MRM than in the Lt. MRM (P<0.05). Further, when tilted only to the anterior-left direction, the angle of inclination was significantly increased to the left side in the Rt. MRM group compared with Lt. MRM group (P=0.024). Meanwhile, when tilted backward, leftward and rightward, there was no statistically significant difference in the inclination angle between the MRM groups and the non-breast cancer group (P>0.05) (Table 3).
Full table
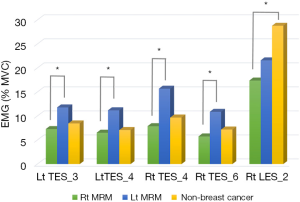
In analysis of muscle activities in the EO, TES, LES, and LM in the dynamic sitting posture, when tilted backward, the activities of TES were statistically significantly lower in the Rt. MRM group than in the Lt. MRM group (P<0.05). In addition, the activity of left TES in the left direction and the right LES in anterior-left direction was lower in the Rt. MRM group (Figure 4).
Discussion
The exact mechanisms for the postural changes after unilateral mastectomy are yet to be determined, and a standard diagnostic criterion have not been established to date. Our results show that MRM can lead to postural changes. Further, these changes can be reliably gauged using BBS and EMG. While there was no significant difference in the static sitting posture between the MRM groups and the non-breast cancer group, the posture tended to move slightly to the anterior-left side of the inclination angle in the MRM groups.
A previous study on spine deformity after unilateral mastectomy showed a significant shift in Cobb’s angle to the non-operated side before and 12 months after surgery (12), and this was aggravated in patients with previous idiopathic scoliosis (12). Mangone et al. also reported significant differences in anterior-posterior flexion of the trunk and pelvic inclination between mastectomy patients and controls (13). However, while postural changes can be more obvious in the dynamic than in the static sitting state, few studies on postural changes in the dynamic sitting state have been conducted. In the current study, the inclination angles were measured in the anterior-posterior (AP) and right-left (RL) axis when tilting in eight directions (A, AL, L, PL, P, PR, R, AR) while sitting on the balance board. Compared with the Lt. MRM group, when tilted forward, the inclination angle in the AP axis was significantly increased to the anterior side in the Rt. MRM group. Meanwhile, there were no significant changes in the non-breast cancer group. However, there was no significant difference in AP inclination angle between the MRM groups and the non-breast cancer group while tilting backward, leftward and rightward. There were also no significant differences in changes in inclination angles on the RL axis except for anterior-left tilting. Compared with the Lt. MRM group, inclination angles on the RL axis during anterior-left tilting increased to the left side in the Rt. MRM group.
It is postulated that loss of breast causes changes in center of pressure (COP), resulting in postural changes to maintain body balance (14). In the case of right-handed patients, COP changes were more severe in the Rt. MRM group, and this is presumed to be the result of body compensation due to loss of breast in the dominant side. That is, it can be inferred that in right-handed breast cancer patients, right MRM had more influence on body posture in the forward-leaning direction than left MRM.
The motions of humerus, scapula, and thoracolumbar spine motions interact synchronously (15). During arm movement, the non-dominant side has a significantly greater scapular upward rotation than the dominant side (15). In addition, rotation upward in the scapula on the mastectomy side is more pronounced than in the non-mastectomy side, and women who undergo following mastectomy show greater excursion than controls (16). The altered motor patterns of the scapula after unilateral mastectomy may be a factor in postural changes. Such changes would influence the movements of the glenohumeral joint and thoracolumbar spine, resulting in postural changes. The inconsistency in the patterns of postural changes is related to the dominant hand and differences in motor power, occupation, and daily lifestyle. Accordingly, some patients do not develop postural changes.
The results of IBR after mastectomy can be used to predict the impact of unilateral mastectomy on postural changes. A previous study by Ciesla et al. suggested that IBR played an important role for maintaining body posture and that photogrammetric examination provided useful information about body posture in breast cancer patients who underwent mastectomy (17). In a study by Jeong et al., the IBR group had a significantly smaller change of Cobb’s angle at 2 years after surgery than patients with only unilateral mastectomy (18). Collectively, these results indicate that IBR is beneficial for spinal alignment. In the current study, postural changes were more severe in the patients who underwent only right MRM. This could indicate that performing IBR immediately after right mastectomy helps prevent postural changes.
There are several difficulties in accurately measuring postural changes. The first is that the relationship between the shoulder, spine, and pelvis should be evaluated in the three dimensions. Second, it is more meaningful to assess static and dynamic states simultaneously. Third, there is a difference in posture between sitting and standing. Previously, posture was evaluated via visual observation, but this has low reliability. Meanwhile, while photographic and radiographic assessments are useful for objective examination, this is also a two-dimensional scale. The values on photographic examination vary depending on the direction of the camera, while the usefulness of radiography is limited by exposure to harmful radiation. Photogrammetry is the most widely used method for postural changes, but it cannot measure postural changes in dynamic conditions. The BBS used in this study can measure both static and dynamic conditions and connects to the EMG system to determine muscular activities. Jung et al. reported that BBS with the patient in sitting position had excellent reliability in the assessment of asymmetric sitting posture and provided useful information in patients with idiopathic scoliosis (9). In current study, this system was used to measure postural changes in patients with unilateral mastectomy, and the results were similar to those of the earlier studies. Collectively, these results could help establish BBS as a useful tool for measuring postural changes under static and dynamic sitting conditions for mastectomy patients.
Muscle activities are recorded using a surface electrode in the dynamic state and expressed as % MVC (19). One study reported that muscle activities of the trunk varied according to body posture type in women with mastectomy (20). Hojan & Manikowska reported that the weight of the external breast prosthesis did not affect the activities of LES during dynamic state at after mastectomy (21). In our study, muscular activities were significantly lower in bilateral TES in the Rt. MRM group than in the Lt. MRM group. It can be speculated that increased inclination angle at AP axis was associated with decreased TES activities in the Rt. MRM group, and these led to postural changes in those who underwent unilateral mastectomy. Rehabilitation exercise programs after mastectomy have been previously reported to maintain trunk symmetry and the body inclination’s angle (6). Although further research is needed, it can be inferred that changes in the para-thoracic muscles after unilateral mastectomy will affect postoperative postural changes of the body. Further, if a rehabilitation exercise program is implemented, body balance can be maintained, and spinal deformity can be prevented.
This study had some limitations. First, the findings could be biased because of the small sample size, which were due to the stringent criteria of being right-handed and undergoing MRM more than 1 year prior. Therefore, there was a limit to generalizing the results. Second, we could not compare the change of inclination angles and muscle activities before and after the mastectomy in MRM groups. The lack of information on pre-operative angles and muscle activity in MRM groups could not confirm the impact of such conditions on post-operative angles and muscle activity. Lastly, there was no comparison according to hand dominance because we only included right-handed patients’ hand.
However, despite these limitations, we believe that our study is valuable because to our best knowledge, this is the first study to determine the effect of unilateral MRM on posture under the dynamic sitting state among right-handed breast cancer patients. Further research is needed to determine the influence of para spinal muscles on body balance after unilateral mastectomy.
Compared with left unilateral mastectomy, it is concluded that right unilateral mastectomy significantly influences postural changes in right-handed patients. Among patients who underwent Rt. MRM, the inclination angle increased to anterior side during tilting forward, and the activities of para-thoracic muscles were lower during tilting backward. Thus, to maintain the trunk balance and prevent the postural changes after unilateral mastectomy, the postoperative exercise programs for the para-thoracic muscles will be helpful. In addition, the BBS with EMG can evaluate postural changes in a dynamic sitting state, making it a useful tool to assess posture changes along with photogrammetry.
Acknowledgments
Funding: This work was supported by the Chungnam National University (No. 2019-0625-01).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/gs-20-466
Data Sharing Statement: Available at http://dx.doi.org/10.21037/gs-20-466
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/gs-20-466). The authors have no conflicts of interest to declare.
Ethical Statement: All authors are accountable for this research in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the appropriate institutional review boards (CNUH 2016-10-009-001) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Harbeck N, Gnant M. Breast cancer. Lancet (London, England) 2017;389:1134-50. [Crossref] [PubMed]
- Abrahams HJ, Gielissen MF, Schmits IC, et al. Risk factors, prevalence, and course of severe fatigue after breast cancer treatment: a meta-analysis involving 12327 breast cancer survivors. Ann Oncol 2016;27:965-74. [Crossref] [PubMed]
- Malicka I, Barczyk K, Hanuszkiewicz J, et al. Body posture of women after breast cancer treatment. Ortop Traumatol Rehabil 2010;12:353-61. [PubMed]
- Głowacka I, Nowikiewicz T, Siedlecki Z, et al. The assessment of the magnitude of frontal plane postural changes in breast cancer patients after breast-conserving therapy or mastectomy - Follow-up results 1 year after the surgical procedure. Pathol Oncol Res 2016;22:203-8. [Crossref] [PubMed]
- Reiland-Smith J. Diagnosis and surgical treatment of breast cancer. S D Med 2010;Spec No:31-7.
- Rostkowska E, Bak M, Samborski W. Body posture in women after mastectomy and its changes as a result of rehabilitation. Adv Med Sci 2006;51:287-97. [PubMed]
- Atanes Mendes Peres AC, Dias de Oliveira Latorre MD, Yugo Maesaka J, et al. Body posture after mastectomy: Comparison between immediate breast reconstruction versus mastectomy alone. Physiother Res Int 2017;22:1642. [Crossref] [PubMed]
- Singla D, Veqar Z. Methods of postural assessment used for sports persons. J Clin Diagn Res 2014;8:LE01-4. [PubMed]
- Jung JY, Cha EJ, Kim KA, et al. Influence of pelvic asymmetry and idiopathic scoliosis in adolescents on postural balance during sitting. Biomed Mater Eng 2015;26:S601-10. [Crossref] [PubMed]
- Jung JY, Kim BO, Kwon TK, et al. Measurement of asymmetric sitting posture using unstable board with accelerometer. Int J Biol Biomed Eng 2014;8:44-50.
- Vera-Garcia FJ, Moreside JM, McGill SM. MVC techniques to normalize trunk muscle EMG in healthy women. J Electromyogr Kinesiol 2010;20:10-6. [Crossref] [PubMed]
- Serel S, Tuzlali ZY, Akkaya Z, et al. Physical effects of unilateral mastectomy on spine deformity. Clin Breast Cancer 2017;17:29-33. [Crossref] [PubMed]
- Mangone M, Bernetti A, Agostini F, et al. Changes in spine alignment and postural balance after breast cancer surgery: A rehabilitative point of view. Biores Open Access 2019;8:121-8.
- Ruhe A, Fejer R, Walker B. Center of pressure excursion as a measure of balance performance in patients with non-specific low back pain compared to healthy controls: a systematic review of the literature. Eur Spine J 2011;20:358-68. [Crossref] [PubMed]
- Crosbie J, Kilbreath SL, Hollmann L, et al. Scapulohumeral rhythm and associated spinal motion. Clin Biomech (Bristol, Avon) 2008;23:184-92. [Crossref] [PubMed]
- Crosbie J, Kilbreath SL, Dylke E, et al. Effects of mastectomy on shoulder and spinal kinematics during bilateral upper-limb movement. Phys Ther 2010;90:679-92. [Crossref] [PubMed]
- Ciesla S, Polom K. The effect of immediate breast reconstruction with Becker-25 prosthesis on the preservation of proper body posture in patients after mastectomy. Eur J Surg Oncol 2010;36:625-31. [Crossref] [PubMed]
- Jeong JH, Choi B, Chang SY, et al. The effect of immediate breast reconstruction on thoracic spine alignment after unilateral mastectomy. Clin Breast Cancer 2018;18:214-9. [Crossref] [PubMed]
- Dankaerts W, O’Sullivan PB, Burnett AF, et al. Reliability of EMG measurements for trunk muscles during maximal and sub-maximal voluntary isometric contractions in healthy controls and CLBP patients. J Electromyogr Kinesiol 2004;14:333-42. [Crossref] [PubMed]
- Malicka I, Hanuszkiewicz J, Stefańska M, et al. Relation between trunk muscle activity and posture type in women following treatment for breast cancer. J Back Musculoskelet Rehabil 2010;23:11-9. [Crossref] [PubMed]
- Hojan K, Manikowska F. Can the weight of an external breast prosthesis influence trunk biomechanics during functional movement in postmastectomy women? Biomed Res Int 2017.9867694. [PubMed]