Does nodule size predict compressive symptoms in patients with thyroid nodules?
Introduction
Thyroid nodules are present in as much as 65% of the population (1). Patients with thyroid nodules often complain of compressive symptoms, including neck fullness, dysphagia, odynophagia, choking, and dyspnea (2). Compressive symptoms may occur in both benign as well as malignant thyroid nodules (3). Surgery for large thyroid nodules or for diffuse thyromegaly often relieves compressive symptoms (4). Several authors have investigated the relationship between compressive symptoms and thyroid lobe volume (5). The exact relationship between thyroid nodule size, however, and compressive symptoms remains unclear. We hypothesized that compressive symptoms would be more likely to occur in patients with larger thyroid size and larger dominant thyroid nodules. We sought to determine whether compressive symptoms are directly related to nodule size and lobe size, and furthermore, to determine whether patients who undergo thyroidectomy for moderate-sized thyroid nodules experience resolution of symptoms postoperatively.
Materials and methods
A retrospective analysis was based on data acquired from an IRB-approved patient database and electronic records at Robert Wood Johnson University Hospital (New Brunswick, NJ, USA). A total of 99 consecutive patients who underwent thyroidectomy or thyroid lobectomy by a single surgeon between July 2008 and January 2012 were identified. These patients had uniform documentation on the presence or absence of compressive symptoms, (specifically of dysphagia, dyspnea, choking sensation, and/or neck fullness) and the presence or absence of visible thyromegaly on physical examination.
Patients were placed into one of two cohorts: those who experienced preoperative compressive symptoms (N=51) and those who did not (N=48). Compressive symptoms were defined as experiencing neck fullness, dysphagia, choking, or dyspnea. Odynophagia and globus were not included, as these were not uniformly identified on patient notes. Nodule and lobe sizes were obtained from preoperative thyroid ultrasound reports and compared between cohorts. We chose to define nodule size by the largest diameter obtained either in transverse, sagittal, or coronal plane. We used this as an alternative to thyroid lobe volume, given the variability in ultrasound technique and radiographic reporting among our various referring radiology centers. In patients with multiple nodules, we chose to focus on the largest diameter of the largest thyroid nodule. We felt that taking into account multiple, often subcentimeter, thyroid nodules would not provide a good assessment of thyroid bulk. Instead, we used the thyroid lobe diameter as a surrogate for thyroid bulk (i.e., multiple small nodules together resulting in thyroid lobe enlargement would be identified by an enlarged thyroid lobe size).
For patients with symptoms of dysphagia thought to be unrelated to the thyroid, diagnostic workup included a barium swallow, direct laryngoscopy and endoscopy, and computed tomography (CT) [or magnetic resonance imaging (MRI)] to rule out other causes of compressive symptoms. Only after other possible causes had been ruled out would thyroid surgery be offered for a <2.0 cm thyroid nodule when a patient insisted that the compressive symptoms were severe.
An assessment of resolution of symptoms on postoperative visits was also recorded. Descriptive statistics were calculated using SAS version 9.1, including student’s t-tests for continuous variables, chi-squared tests for categorical data, and Wilcoxon-Mann-Whitney rank sum tests for ordinal variables.
Results
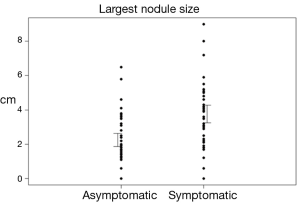
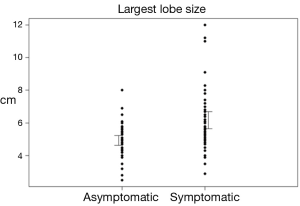
Patient demographics are shown in Table 1. The most common diagnosis in both asymptomatic and symptomatic groups was multinodular goiter (31.3% and 70.6% of patients respectively), with more patients in the symptomatic group diagnosed with multinodular goiter (P<0.0001). Mean thyroid nodule size in symptomatic patients was 3.8 cm [95% confidence interval (CI): 3.3-4.3] versus 2.2 cm (95% CI: 1.9-2.6) in asymptomatic patients (P<0.0001). Mean lobe diameter was 6.2 cm (95% CI: 5.7-6.7) in symptomatic patients versus 4.9 cm (95% CI: 4.6-5.2) in asymptomatic patients (P<0.001), Table 2. CIs and ranges of nodule size and diameter between groups are shown in Figures 1 and 2, respectively. Visible thyromegaly was present in 65.2% of patients with compressive symptoms compared to 15.4% of asymptomatic patients (P<0.0001), also shown in Table 2.
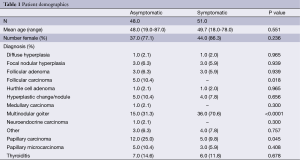
Full table
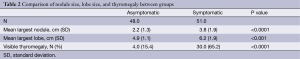
Full table
The most common symptom was dysphagia, occurring in 80% of patients in the cohort, followed by globus (69%), choking (49%), and dyspnea (32%). Patients in which the left lobe was enlarged or had an enlarged left-sided nodule trended towards experiencing more symptoms of dysphagia than those on the right; however, these differences were not statistically significant (P=0.354, P=0.435 respectively). Of patients who underwent surgery for compressive symptoms, 92.7% had relief of their symptoms postoperatively (P<0.0001). Of patients where the largest thyroid nodule was greater than 1.5 cm, 97% showed improvement in symptoms postoperatively. Of three patients with compressive symptoms with a negative barium swallow and dysphagia workup, and with a thyroid nodule <1.5 cm, only two of the three experienced resolution of compressive symptoms.
Discussion
Compressive symptoms are a common finding in patients with thyroid nodules (6,7). In two large series, compressive symptoms ranged between 11% and 22% of patients (6,7). Surgery for compressive symptoms for patients with marked thyromegaly has been shown to be effective (4,5,8). A study analyzing outcomes in 29 patients with marked thyromegaly who underwent thyroidectomy, of which 25 had compressive symptoms, found that all 25 patients in this group reported improvement in symptoms after surgery (4). Of note, 18 of these patients had evidence of tracheal compression and 19 had evidence of substernal extension preoperatively (4). Other studies have also shown that thyromegaly in the setting of tracheal compression, deviation, or substernal extension is often associated compressive symptoms, which improve with surgery (4,5,8,9).
The efficacy of thyroid surgery for compressive symptoms from smaller thyroid nodules is less well defined. A more recent study, and the only series to compare thyroid volume and compressive symptoms, analyzed 333 consecutive patients who underwent thyroidectomy (for all indications). The study found that as many as 52% of patients experienced some form of compressive symptoms preoperatively when adequately questioned during initial interview (5). The most common compressive symptom was dysphagia, found in 39% (131 patients), followed by dyspnea in 25% (83 patients), and globus found in 10% (32 patients). On average, patients with compressive symptoms were found to have a larger thyroid gland compared to asymptomatic patients (75.5 vs. 37.1 mL) (5). The authors, however, did not examine whether nodule size or volume correlated with compressive symptoms.
In our study, compressive symptoms were present preoperatively in 51.5% of our patients. The most common symptom was dysphagia, occurring in 80% of patients, followed by globus (69%), choking (49%), and dyspnea (32%). Patients with compressive symptoms were more likely to have larger thyroid lobes [6.2 cm (95% CI: 5.7-6.7) vs. 4.9 cm (95% CI: 4.6-5.2), P<0.001] and larger thyroid nodules [3.8 cm (95% CI: 3.3-4.3) vs. 2.2 cm (95% CI: 1.9-2.6), P<0.0001)].
In the study by Banks et al., 92% of patients with compressive symptoms who underwent thyroidectomy had improvement in their symptoms, however, 8% had persistent compressive symptoms (5). Interestingly, the average volume of thyroid gland removed in those patients whose compressive symptoms improved compared to those whose symptoms did not improve was statistically the same. In their series, the presence of anaplastic thyroid carcinoma, a history of subglottic stenosis, and the development of a postoperative hematoma was associated with the persistence of postoperative compressive symptoms (5).
In our study, 93% of patients experienced resolution of symptoms postoperatively. When excluding patients with thyroid nodules <1.5 cm, 97% of patients experienced resolution of symptoms postoperatively. Of three patients with compressive symptoms with a negative barium swallow and dysphagia workup, and with a thyroid nodule <1.5 cm, only two of three experienced resolution of compressive symptoms.
We chose visible thyromegaly as a physical exam finding to provide gross assessment of thyroid bulk despite its limitations, as this was an easily obtained finding, and because the World Health Organization and the International Council for the Control of Iodine Deficiency Disorders has already proposed a grading system for endemic goiter (10). In addition, there is published data mostly from the endemic goiter literature that shows good correlation between “visible goiter” physical examination findings with compressive symptoms (11). Banks et al. also investigated whether “marked thyroid enlargement” predicted compressive symptoms. The authors defined “marked thyroid enlargement” as a thyroid volume >40 mL for a lobe or >80 mL for bilateral lobes (5). They found that 31% of patients with compressive symptoms had marked thyromegaly compared to only 17% of patients without compressive symptoms (5). In our study, we instead chose to distinguish “visible thyromegaly” from “palpable thyromegaly” based on a physical examination findings rather than a calculated sonographic measurement. We found that visible thyromegaly was present in 65.2% of symptomatic patients and in only 15.4% of asymptomatic patients (P<0.0001).
Banks et al. demonstrated that compressive symptoms occurred most frequently in patients with lymphocytic thyroiditis (72%) and anaplastic thyroid carcinoma (71%), followed by multinodular goiter (60%). Only 20% of patients with papillary thyroid carcinoma experienced compressive symptoms (5). Unfortunately, their study did not control for nodule size. Therefore, it is unclear whether patients with papillary thyroid carcinoma experienced less compressive symptoms than those with multinodular goiter, for example, because of the malignant nature of the nodule or because of a probable smaller nodule size. In our series, we found that 71% of symptomatic patients had multinodular goiter while 16% has papillary thyroid carcinoma, and only 12% had thyroiditis. In our analysis, only multinodular goiter was associated with more compressive symptoms.
We also investigated whether nodules on the left were more likely to cause compressive symptoms, especially dysphagia. We hypothesized that as the cervical esophagus normally lies in the left neck (posterolaterally to the left thyroid lobe), left sided thyroid nodules might be more likely to cause dysphagia. However, there was no difference in compressive symptoms of right vs. left sided thyroid nodules.
We acknowledge several limitations of this study. First, as a retrospective study, the design introduces selection bias and limits the ability to determine whether the relationship between nodule size and compressive symptoms is causal or predictive. In addition, patient factors such as ethnicity, height or body habitus, potentially contributing to the presence of compressive symptoms, were not assessed. Next, while our study was adequately powered to demonstrate significant improvement in compressive symptoms in patients with thyroid nodules >1.5 cm, our study does have a relatively small cohort of patients. Further, we did not evaluate whether thyroid nodules were calcified or not (ostensibly, calcified thyroid nodules might cause more compressive symptoms), nor did we qualify whether the thyroid nodules were in an anterior or posterior location (ostensibly, posterior left sided thyroid nodules might be more likely to cause dysphagia compared to anterior left sided thyroid nodules). Much of this information was not readily available from the sonography reports.
Conclusions
Nodule size and lobe size directly correlate with compressive symptoms. Of patients with compressive symptoms and a thyroid nodule >1.5 cm, 97% will experience improvement in symptoms postoperatively.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Dean DS, Gharib H. Epidemiology of thyroid nodules. Best Pract Res Clin Endocrinol Metab 2008;22:901-11. [PubMed]
- Greenblatt DY, Sippel R, Leverson G, et al. Thyroid resection improves perception of swallowing function in patients with thyroid disease. World J Surg 2009;33:255-60. [PubMed]
- Moumen M, Mehhane M, Kadiri B, et al. Compressive goiters. Apropos of 80 cases. J Chir (Paris) 1989;126:521-6. [PubMed]
- McHenry CR, Piotrowski JJ. Thyroidectomy in patients with marked thyroid enlargement: airway management, morbidity, and outcome. Am Surg 1994;60:586-91. [PubMed]
- Banks CA, Ayers CM, Hornig JD, et al. Thyroid disease and compressive symptoms. Laryngoscope 2012;122:13-6. [PubMed]
- Lacoste L, Gineste D, Karayan J, et al. Airway complications in thyroid surgery. Ann Otol Rhinol Laryngol 1993;102:441-6. [PubMed]
- Alfonso A, Christoudias G, Amaruddin Q, et al. Tracheal or esophageal compression due to benign thyroid disease. Am J Surg 1981;142:350-4. [PubMed]
- Netterville JL, Coleman SC, Smith JC, et al. Management of substernal goiter. Laryngoscope 1998;108:1611-7. [PubMed]
- Wormer BA, McHenry CR. Hashimoto’s thyroiditis: outcome of surgical resection for patients with thyromegaly and compressive symptoms. Am J Surg 2011;201:416-9; discussion 419. [PubMed]
- WHO, UNICEF, ICCIDD. Indicators for assessing Iodine Deficiency Disorders and their control through salt iodization. Geneva: WHO, 1994.
- Agarwal A, Agarwal S, Tewari P, et al. Clinicopathological profile, airway management, and outcome in huge multinodular goiters: an institutional experience from an endemic goiter region. World J Surg 2012;36:755-60. [PubMed]


