
Therapeutic efficacy of two surgical methods on the secondary hyperparathyroidism
Introduction
With the improvement of renal replacement technology and medical security system in China, the life expectancy of patients receiving maintenance dialysis has been significantly prolonged, but the incidence of complications caused by dialysis has also increased. Secondary hyperparathyroidism (SHPT) is one of the serious complications caused by calcium and phosphorus metabolism disturbance secondary to long-term hypocalcemia hemodialysis or peritoneal dialysis in patients with chronic renal failure (CRF) (1). If left untreated, it will increase the risk for calcification, abnormal bone morphology, ectopic calcification and cardiovascular events, which seriously affect the patient’s quality of life (QOL) and survival time (2). Parathyroidectomy (PTX) can be performed via three main surgical procedures: subtotal parathyroidectomy (SPTX), total parathyroidectomy + autologous implantation (TPTX + AT) and TPTX (3). The first two are mainstream surgical methods, but there is no consensus on one is better over another (4). Currently, surgeons often select the surgical method mainly based on their judgement and preference.
This study aimed to investigate the therapeutic efficacy of two surgical methods on the HPT secondary to uraemia.
Methods
Patients
Patients who received PTX between May 2015 and May 2018 (n=38) were included into present study. Patients were divided into two groups according to the surgical methods used: 22 patients received SPTX (SPTX group) and 16 patients underwent TPTX + AT (TPTX + AT group).
Surgical methods
In these patients, SPTX or TPTX + AT was performed. If the number of parathyroid glands was smaller than 4, TPTX was employed.
SPTX: Three semi parathyroid glands are removed, and the smallest parathyroid gland is selected to retain half, about 30~60 mg. If the parathyroid glands in the lower thyroid gland are smaller and softer, try to keep them in place. The remaining half of the parathyroid glands need to be carefully separated when removing the other half, to protect the blood supply, and a metal clip can be placed on the reserved side glands to facilitate identification during future surgery.
TPTX + AT: select the smallest, relatively normal-looking parathyroid glands or tissues that have been diffusely hyperplasia confirmed by rapid freezing pathology. Cut about 0.5 cm3 from parathyroid gland, and store it in frozen Ringer’s solution or saline. After resection of all parathyroid glands, the gland to be transplanted are cut into small pieces of 1 mm × 1 mm × 1 mm and about 20–30 copies. Implant them in the forearm muscles on the non-dialysis fistula side of the patient. The muscle fascia at the transplantation site is sutured with a non-absorbable surgical thread as a marker for reoperation.
TPTX: completely remove all parathyroid glands detected during the operation.
Intraoperative PTH was used in SPTX. We conclude that the range of PTH reduction from 70% to 90% after 10 to 20 minutes of glandular resection can be considered as a sign that the surgery has achieved expectations. The surgeries of these 32 patients were performed by a surgeon.
Observations
The PTH, ALP, calcium, phosphorus and bone mineral density (BMD) were recorded before and after surgery. The success rate of surgery and recurrence rate were calculated. The post-operative complications (hypocalcemia, recurrent laryngeal nerve injury and wound infection) were recorded. Patients were followed up, and the PTH, ALP, BMD and clinical symptoms were monitored. The post-operative calcium supplement was calculated as follow: calcium supplement (mg) = 90 mg × volume of intravenous calcium gluconate × 10% + amount of calcium per tablet (mg) × number of tablets ×40%. The mean calcium supplement was calculated as follow: mean = total calcium supplement (mg)/days/body weight (kg). The above parameters were compared between two groups. The timepoint for all follow-up patients was 1 year.
According to the KDOQI clinical guidelines, the success of surgery is defined as: blood calcium levels continue to maintain normal levels for 6 months or more after surgery, and PTH <300 pg/dL, and/or clinical symptoms are reduced. Surgery failure is defined as: serum calcium level rises above the normal reference range within six months after surgery, or PTH fails to fall by more than 50% or PTH persists >800 pg/dL after surgery Hyperparathyroidism).
The latest definition of recurrence of hyperparathyroidism is more than 6 months after successful PTX, with serum calcium above the normal reference range, elevated PTH levels, and / or reoperation with typical clinical symptoms.
Postoperative hypocalcemia is defined as: when the serum protein concentration is normal postoperatively, the blood calcium is below 2.2 mmol/L. The main manifestation of incision infection is redness, swelling and pain. The definitions that need to be supplemented have been basically supplemented. Bone mineral density is measured by dual-energy X-ray bone density measurement (average of left femoral neck, Wards triangle, and trochanter). Postoperative QOL analysis was based on 12 aspects of appetite, mental, sleep, fatigue, pain and so on. The full score is 60 points, divided into 5 grades.
Statistical analysis
Statistical analysis was performed with SPSS version 19.0. Data with normal distribution are expressed as mean ± standard deviation (SD) and those with abnormal distribution as median (interquartile range). Data with normal distribution were compared with t test or analysis of variance; data with abnormal distribution with nonparametric rank sum test. Correlation analysis was done for a part of data, and correlation coefficient was calculated. A value of two tailed P<0.05 was considered statistically significant.
Results
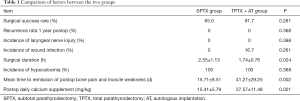
Of these patients, 23 were diagnosed with chronic glomerulonephritis (60.5%), 4 with hypertensive renal cirrhosis (10.5%), 4 with diabetic nephropathy (10.5%), 3 with chronic pyelonephritis (7.9%) and 1 with polycystic kidney (2.6%), but the cause was unknown in 3 patients (7.9%). In the SPTX group, there were 8 males and 14 females, the mean age was 50.55±7.82 years, the duration of dialysis was 107.95±45.12 months, 21 received hemodialysis and 1 underwent peritoneal dialysis. In the TPTX + AT group, there were 7 males and 9 females, the mean age was 48.44±8.51 years, the duration of dialysis was 104.13±52.25 months, and all the patients received hemodialysis. Among 38 patients, 20 received SPTX (52.6%) and 12 underwent TPTX + AT (31.6%); 6 patients received TPTX (15.8%), 2 from SPTX group and 4 from TPTX + AT group. In the final analysis, 32 patients were included. The incidence of hypocalcemia was 100% in both groups. The incidence of wound infection was 0 and 16.7% (2/12) in the SPTX group and TPTX + AT group, respectively. The infection incisions in the two patients were both in the forearm. Recurrent laryngeal nerve injury was not observed in both groups. The success rate was 85.0% (17/20) and 91.7% (11/12) in the SPTX group and TPTX + AT group, respectively. None had recurrence within 1 year after surgery (Table 1).
Full table
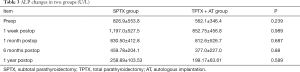
The serum PTH level was comparable between two groups before, during and after surgery (P>0.05). The serum PTH level was the lowest at 1–7 days after surgery (Table 2). The serum ALP level was comparable between two groups before, during and after surgery (P>0.05) (Table 3). The BMD was similar between two groups before surgery. At 3 months and 1 year after surgery, the BMD in the SPTX group was significantly higher than in the TPTX + AT group (P=0.03 and 0.000, respectively) (Table 4).

Full table
Full table

Full table
The mean post-operative daily calcium supplement was 15.41±5.79 mg/kg in the SPTX group and 27.57±11.48 mg/kg in the TPTX + AT group, showing significant difference (P<0.05) (Table 1). The mean time to remission of post-operative bone pain and muscle weakness was 15.71±8.51 days in the SPTX group and 41.27±29.25 days in the TPTX + AT group, showing marked difference (Table 1).
The pre-operative QOL score was 39.88±7.17 in the SPTX group and 36.00±7.80 in the TPTX + AT group, showing no marked difference, but the post-operative QOL in the SPTX group (47.35±7.85) was better than in the TPTX + AT group (37.82±8.15) (P=0.005; Table 5).

Full table
No patients were lost to follow-up. However, some indicators were lost due to failure to detect in time.
Discussion
Renal hyperparathyroidism is a type of SHPT. Levin et al. (5) found PTH began to increase when the glomerular filtration rate (GFR) was lower than 60 mL/min. The serum PTH increases as a response, aiming to maintain the mineral metabolism balance until the GFR was lower than 40 mL/min resulting in mineral metabolism imbalance (6). Under this condition, phosphorus-restricted diet, phosphorus chelating agent, calcium agent and active vitamin D are needed. The phosphorus-restricted diet is helpful for the control of blood phosphorus. The supplementation with active vitamin D can improve the deficiency of endogenous vitamin D and inhibit the synthesis and secretion of PTH. Calcium agent can increase the serum calcium and reduce the absorption of phosphorus in the intestine. As the disease progresses, the parathyroid glands progress from diffuse hyperplasia to nodular hyperplasia. The calcium receptors and vitamin D receptors in the parathyroid cells decrease, leading to the drug resistance, and PTH is synthesized and secreted autonomically. Under this condition, surgery is required to solve this problem (7).
The resection of parathyroid gland can be performed with different methods, including SPTX, TPTX + AT and TPTX alone. SHPT is often managed by using SPTX or TPTX + AT.
Neagoe et al. (8) conducted a randomized study in which the PTX was compared with TPTX + AT. They failed to find the significant differences in the efficacy and post-operative recurrence. Thus, the selection of surgical methods is mainly dependent on the surgeon’s preference (9-12).
In the present study, our results showed SPTX had a lower success rate as compared to TPTX + AT, which might be ascribed to the difficulty in the determination and standardization of the weight of residual parathyroid gland and the possibility of residual nodular adenomatous hyperplasia.
SPTX is a relatively old surgical method, in which the parathyroid gland weighing 40–50 mg is preserved (13), but this method has been criticized by some experts due to the high recurrence rate (14). In recent years, some studies have reported that the efficacy of removal of 3 parathyroid glands plus 3/4–7/8 of remaining parathyroid gland is superior to that of traditional method (15). There is still no consensus on this issue in China, and the size of residual parathyroid gland ranges from 1/8 to 1/2 of the smallest parathyroid gland (16). Some clinicians even propose the resection of 3 or less parathyroid glands because not all the parathyroid glands are identified during surgery or this is their own preference. Studies have compared the efficacy between less-than subtotal resection (removal of no more than 3 parathyroid glands) and subtotal resection, and results reveal less-than subtotal resection significantly increases the risk for recurrence and persistent hyperparathyroidism (17).
Richards et al. (11) conducted a meta analysis on 53 studies which were published between 1983 and 2004 and investigated the surgical management of SHPT. Their results showed 501 patients received a second surgery due to recurrence or persistent hyperparathyroidism, of whom 42.5% received SPTX and 34% underwent TPTX + AT on first treatment.
It has been reported that the long term recurrence rate is 21.4% and 32.1% after SPTX and TPTX + AT, respectively (2,12). In the present study, the recurrence rate was similar between two groups.
In our study, recurrent laryngeal nerve injury was not observed in both groups. The lower parathyroid gland is close to the recurrent laryngeal nerve at the level of laryngeal entrance, and surgery has the risk for recurrent laryngeal nerve injury. Generally, it may be avoided for experienced surgeons. It has been reported that a second exploration has a higher risk for recurrent laryngeal nerve injury as compared to the first surgery (18), and theoretically, the risk for recurrent laryngeal nerve injury in SPTX is higher than that in TPTX + AT. In the surgery, the residual parathyroid glands can be marked with titanium clips, which is helpful for the identification of residual parathyroid glands and also avoids the recurrent laryngeal nerve injury in the second surgery.
The incidence of wound infection in the SPTX group was lower than in the TPTX + AT group because patients receiving TPTX +AT experienced forearm skin and sarcolemma incision, resulting in a higher incidence of wound infection. In the present study, forearm incision was made in all the patients.
Time of surgery: In the TPTX + AT, MIBI technique is employed, which may significantly shorten the time of surgical exploration. Although the MIBI has a favorable qualitative determination (with or without residual parathyroid gland), the capability of localization of parathyroid gland is poor for MIBI. Thus, MIBI is not used in SPTX, and intra-operative rapid PTH detection is employed, which is time-consuming. During the SPTX operation, intraoperative PTH monitoring is performed. The intraoperative PTH reduction rate reached 70% to consider the operation to have the expected effect. If the intraoperative PTH reduction rate is less than 70%, the exploration is continued. If no ectopic parathyroid glands are detected, it should be considered to repeat the parathyroid gland lymphoid, adipose tissue, and thymus tongue resection.
The change in serum PTH suggested that both methods were effective to reduce serum PTH in SHPT patients, and PTH reached a lowest level at 1–7 days after surgery, which may be related to incomplete compensation of implanted parathyroid gland, the reduction of PTH higher than the production of PTH. Within 7 days after surgery, the endogenous PTH is exhausted and thus serum PTH reaches a lowest level. After 7 days, the implanted and/or residual parathyroid cells and parathyroid cells in the thymus may compensate the reduction of PTH, and thereafter serum PTH begins to increase. The change in serum PTH was similar in both groups, and there was no marked difference between groups at different time points.
In addition, the serum ALP increased (but not decreased) within 1 week after surgery. The elevated ALP before surgery is mainly ascribed to the secreted ALP by osteoblasts, which may antagonize the PTH induced activation of osteoclasts. After surgery, the osteolysis effect disappears, and the activity of osteoblasts peaks within 1 week after surgery. These osteoblasts secret a large amount of ALP, which promotes the deposition of calcium and phosphorus in the bone. Thus, the serum ALP within 1 week after surgery was higher than that before surgery. At 1 week after surgery, the osteogenic effect is inhibited as a feedback due to the reduced activity of osteoblasts, and then ALP production reduces. No significant difference was observed at different time points after surgery.
The BMD increased gradually after surgery. In the SPTX group, the BMD peaked within 3 months after surgery, which suggests early compensation of residual parathyroid gland. In the TPTX + AT group, the BMD peaked at 3–6 months after surgery, which reflects the compensation of implanted parathyroid gland. Significant difference was found in the BMD between group after surgery.
The hypocalcemia in the TPTX + AT group was more severe than in the SPTX group, but the duration of hypocalcemia in the SPTX group was shorter than in the TPTX + AT group, which was also confirmed by our previous study (19). The blood supply to the parathyroid gland is preserved in the SPTX and thus the residual parathyroid gland is easy to survive to compensate the reduction in serum calcium. Thus, the hypocalcemia is compromised. However, the survival of implanted parathyroid gland is hard to estimate in the TPTX + AT, and thus patients receiving TPTX + AT have a higher risk for permanent hypoparathyroidism as compared to those undergoing SPTX (20).
In the SPTX group, the time to remission of bone pain and muscle weakness was significantly shorter than in the TPTX + AT group. 2 patients were unable to walk after surgery, which was still observed at 1 year after surgery. This might be ascribed to the destruction of trabecular bone due to long term hypocalcemia hemodialysis and hyperphosphatemia. Although the bone mineral content increases to a certain extent after surgery, it is hard to return to the normal level (21).
Currently, the surgical method is determined based on the surgeon’s preference and the clinical condition of patients (possibility of renal transplantation, age, expected survival time, vascular compliance of medication and medical cost). Exploring and resecting all the parathyroid glands (including ectopic and excess glands) is important for the surgical success.
For patients requiring long-term hemodialysis after parathyroid surgery, the risk of recurrence is not negligible (up to 20% after 10 years) (8). Relatively, removing residual parathyroid gland from the forearm is safer than re-exploring the neck. However, the implanted glands are easy to grow into muscle tissues, and thus they are not easily identified during re-operation. On the other hand, TPTX + AT has a higher risk for permanent hypoparathyroidism than SPTX because the survival of the implanted parathyroid glands is difficult to estimate in TPTX + AT.
QOL scoring system can be used to comprehensively assess the QOL of patients. Our results showed the QOL within 1 year after SPTX was significantly better than that after TPTX + AT.
On the basis of our findings, we speculate that SPTX may achieve a better short term efficacy, but patients receiving TPTX + AT may have a better long term effectiveness. We recommend TPTX + AT for patients who have no renal transplantation plan and will receive long term hemodialysis. For patients who will received renal transplantation, are old and have a poor compliance to long term calcium supplement, SPTX is recommended.
The biggest limitations of this study are the small sample size of our patients and the short follow-up time of our study. Therefore, some errors may be caused, leading to biased conclusions. Further expanding the sample size and increasing the follow-up time can increase the reliability of our conclusions. In addition, more detailed hierarchical research may reveal some new information.
Acknowledgments
Funding: The present study was partially supported by the Youth Science and Technology Project of Promoting Health Through Science and Education in Suzhou (no. kjxw2016029), the national Natural Science Foundation of China (no. 81672970), the Natural Science Foundation of Jiangsu Province (no. bk20160338), the Projects of Suzhou Technology Bureau (nos. sys201552, ss201753 and sys2018054), Found of Suzhou Introduced Team of Clinical Medical Experts (no. szyjtd201803), Jiangsu Province’s Graduate Student Research Innovation Project (no. kycx19_1986) and the Second Affiliated Hospital of Soochow University Preponderant Clinic Discipline Group Project Funding.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/gs.2020.03.08). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Ethics Committee of The Affiliated Suzhou Hospital of Nanjing Medical University (Ethical batch number is KL901058). All patients provided written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhou X, Zhang H. Experience of diagnosis and treatment of 44 patients with hyperparathyroidism. Chin J Endocr Surg 2019;13:40-3.
- Zitt E, Lhotta K. Management of secondary hyperparathyroidism-current impact of parathyroidectomy. Wien Med Wochenschr 2016;166:254-8. [Crossref] [PubMed]
- Magnabosco FF, Tavares MR, Montenegro FL. Surgical treatment of secondary hyperparathyroidism: a systematic review of the literature. Arq Bras Endocrinol Metabol 2014;58:562-71. [Crossref] [PubMed]
- Tominaga Y, Matsuoka S, Uno N. Surgical and medical treatment of secondary hyperparathyroidism in patients on continuous dialysis. World J Surg 2009;33:2335-42. [Crossref] [PubMed]
- Levin A, Bakris GL, Molitch M, et al. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int 2007;71:31-8. [Crossref] [PubMed]
- Batista DG, Neves KR, Graciolli FG, et al. The bone histology spectrum in experimental renal failure: adverse effects of phosphate and parathyroid hormone disturbances. Calcif Tissue Int 2010;87:60-7. [Crossref] [PubMed]
- Conti-Freitas LC, Foss-Freitas MC, Lucca LJ, et al. Dynamics of parathyroid hormone secretion after total parathyroidectomy and autotransplantation. World J Surg 2009;33:1403-7. [Crossref] [PubMed]
- Neagoe RM, Muresan M, Voidazan S, et al. Subtotal parathyroidectomy versus total parathyroidectomy with autotransplant in secondary hyperparathyroidism - a single-centre prospective cohort of 43 patients. Endokrynol Pol 2016;67:202-9. [Crossref] [PubMed]
- Komaba H, Taniguchi M, Wada A, et al. Parathyroidectomy and survival among Japanese hemodialysis patients with secondary hyperparathyroidism. Kidney Int 2015;88:350-9. [Crossref] [PubMed]
- Li C, Lv L, Wang H, et al. Total parathyroidectomy versus total parathyroidectomy with autotransplantation for secondary hyperparathyroidism: systematic review and meta-analysis. Ren Fail 2017;39:678-87. [Crossref] [PubMed]
- Richards ML, Wormuth J, Bingener J, et al. Parathyroidectomy in secondary hyperparathyroidism: Is there an optimal operative management? Surgery 2006;139:174-80. [Crossref] [PubMed]
- Sakman G, Parsak CK, Balal M, et al. Outcomes of total parathyroidectomy with autotransplantation versus subtotal parathyroidectomy with routine addition of thymectomy to both groups: single center experience of secondary hyperparathyroidism. Balkan Med J 2014;31:77-82. [Crossref] [PubMed]
- Ohe MN, Santos RO, Neves MC, et al. Autotransplant tissue selection criteria with or without stereomicroscopy in parathyroidectomy for treatment of renal hyperparathyroidism. Braz J Otorhinolaryngol 2014;80:318-24. [Crossref] [PubMed]
- Konturek A, Barczynski M, Stopa M, et al. Subtotal parathyroidectomy for secondary renal hyperparathyroidism: a 20-year surgical outcome study. Langenbecks Arch Surg 2016;401:965-74. [Crossref] [PubMed]
- Low TH, Yoo J. Subtotal parathyroidectomy and relocation of the parathyroid remnant for renal hyperparathyroidism: modification of a traditional operation. J Otolaryngol Head Neck Surg 2017;46:60. [Crossref] [PubMed]
- Zhang Y, Zheng C, Sun W, et al. Comparison of therapeutic efficacy between two surgical methods for parathyroidism secondary to uremia. Chinese Journal of Integrated Traditional and Western Nephrology 2008;9:710-2.
- Hamouda M, Ben Dhia N, Aloui S, et al. Surgical treatment of secondary hyperparathyroidism in patients with chronic renal failure. Nephrol Ther 2011;7:105-10. [Crossref] [PubMed]
- Rayes N, Seehofer D, Schindler R, et al. Long-term results of subtotal vs total parathyroidectomy without autotransplantation in kidney transplant recipients. Arch Surg 2008;143:756-61; discussion 761. [Crossref] [PubMed]
- Gu C, Chen S, Tian B, et al. Early treatment of postoperative hypocalcemia in uremic patients with secondary hyperparathyroidism. Acta Medica Mediterr 2014;30:213-9.
- Yuan Q, Liao Y, Zhou R, et al. Subtotal parathyroidectomy versus total parathyroidectomy with autotransplantation for secondary hyperparathyroidism: an updated systematic review and meta-analysis. Langenbecks Arch Surg 2019;404:669-79. [Crossref] [PubMed]
- Neves MCD, Rocha LAD, Cervantes O, et al. Initial surgical results of 500 Parathyroidectomies for Hyperparathyroidism related to chronic kidney disease - mineral and bone disorder. J Bras Nefrol 2018;40:319-25. [Crossref] [PubMed]


