Bilateral breast reconstruction with bipedicle transverse rectus abdominis myocutaneous (TRAM) flap for simultaneous delayed and immediate breast reconstruction after therapeutic modified radical mastectomy and prophylactic nipple sparing mastectomy
Introduction
Breast cancer is the most commonly diagnosed cancer in women and the second leading cause of cancer mortality in women (1). It is estimated that between 5% and 10% of all incidents of breast cancer can be attributed to hereditary breast cancer susceptibility genes, including BRCA1 and BRCA2 (2). Women who inherit a BRCA1/2 mutation have a 40% to 65% lifetime risk of breast cancer (3).
BRCA testing is suggested to perform after the completion of primary surgery for breast cancer in the high-risk patient, for example, early-age-onset breast cancer, triple negative breast cancer, patient with breast cancer in first degree relative at the age of 50 (4). BRCA gene mutation testing has become widely available in clinical and research settings, many women are being tested and once their genetic testing found to have deleterious BRCA mutations, they will be counseled to undergo a second breast surgery including prophylactic mastectomy or bilateral salpingo-oophorectomy (SO) as the preventive and management options for risk reduction.
Contralateral prophylactic mastectomy (CPM) is potentially indicated for risk reduction in patients at high risk for the contralateral breast cancer. After CPM is performed, breast reconstruction is the further options for patients. However, they have to choose between immediate reconstruction which has a better aesthetic outcome due to preservation of the three-dimensional breast skin envelope and the benefit in the psychological aspect. Whereas, delayed breast reconstruction is usually reserved for patients who will require post-mastectomy radiotherapy (PMRT) (5). Prostheses implant or autologous tissue for breast reconstruction is another topic that the surgeons must discuss with their patients.
We report a breast cancer patient who underwent immediate breast reconstruction and delayed breast reconstruction on the index breast.
Case report
A case of 29-year-old woman presented at breast cancer clinic concerned about her risk of developing contralateral breast cancer. Ten years ago when she was 19 year-old, she had breast cancer diagnosed. She underwent left modified radical mastectomy followed by adjuvant chemotherapy and radiation therapy. The pathological report was invasive ductal carcinoma, stage IIb T3N0M0, triple negative subtype. At the age of 25, she had large multiple intramural myoma uteri and underwent transabdominal hysterectomy (TAH) with left salpingo-oophorectomy (SO).
She has family history of breast cancer in first degree relatives. Her mother and her sister were diagnosed of breast cancer at the age of 30 and 35 respectively. Her grandmother also died from breast cancer with unknown age of onset. Since her strong family history of breast cancer, she came to the breast cancer clinic and asked for prophylactic mastectomy for her right breast. She survives for ten years without any locoregional recurrence and distant metastasis evidence.
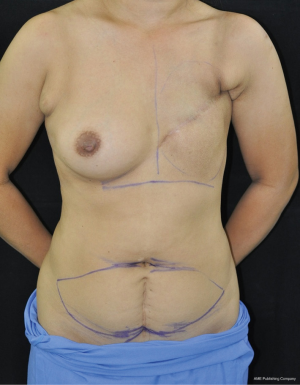
Right prophylactic nipple-sparing mastectomy with immediate breast reconstruction with ipsilateral pedicle transverse rectus abdominis myocutaneous (TRAM) flap was performed. Left delayed reconstruction with ipsilateral pedicle TRAM flap was done simultaneously. The entired operation lasted five hours and she had uneventful recovery during the admission. The pathological report of right breast showed benign breast parenchyma without evidence of malignancy. The last visit at the clinic three months post operation, there was no flap complication and the patient was very satisfied with her cosmesis appearance.
Discussion
The rate of CPM is increasing worldwide. There are several reasons for patient and physician to opt for CPM, such as, better understanding of genetic and hereditary risk or immediate breast reconstruction. This woman is a good candidate for CPM, because she has strong family history of breast cancer. Her mother and her sister were diagnosed of breast cancer in the young age.
The individuals most likely to benefit from prophylactic mastectomy are BRCA gene carriers and those who have a strong family history of breast cancer. And this patient who has a personal history of breast cancer is also at higher risk for developing contralateral breast cancer (6).
Even though the BRCA mutation testing have not been done because of her financial problem, but from her strong family history of breast cancer, her risk of a second breast cancer is up to 35% much higher by 16 years after the diagnosis of index cancer (7). Moreover, her history of breast cancer will increase the cumulative risk of 17% at 20 years after the diagnosis of first breast cancer (8).
CPM is potentially indicated for risk reduction in patients at high risk for the contralateral breast cancer, patients in whom subsequent surveillance of the contralateral breast would be challenging because of the increased density or diffuse indeterminate microcalcifications, and for achieving symmetry in the contralateral breast or achieving balance in non-reconstructed patients (9). According to the report CPM can reduce 94% to 96% of breast cancer at a median follow-up of ten years in 745 women with a first breast cancer and family history of breast cancer (10).
Therefore, CPM is a reasonable choice for this patient. Considering her compliance to perform second surgery, we chose to perform the right nipple-sparing mastectomy with immediate breast reconstruction. Pedicle TRAM flap were raise bilaterally and transferred to both chest for right immediate breast reconstruction and left delayed breast reconstruction. This case is also a good candidate for other reconstruction techniques, for example, implant based reconstruction, bilateral extended latissimus dorsi flaps, latissimus dorsi flap with implant or bilateral microvascular free tissue transfer using autologous tissue (Figures 1,2).
Conclusions
The more advance knowledge and technology in diagnosis of hereditary breast along with evolution of breast cancer surgery has already altered the current breast cancer treatment. The rate of prophylactic mastectomy is increasing and therefore its benefit is proven among genetic and very high risk patient. The quality of life for post mastectomy patient as well as for mastectomy candidates are also improved and maintained due to breast reconstructive surgery. This case report shows a successfully treated young breast cancer patient who has CPM done ten years after primary oncologic surgery and also had simultaneous bilateral breast reconstruction. The oncologic and reconstructive benefit should always be discussed for individual patient to achieve maximal satisfaction and survival.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin 2013;63:11-30. [PubMed]
- McPherson K, Steel CM, Dixon JM. Breast cancer: epidemiology, risk factors and genetics. BMJ 2000;321:624-8. [PubMed]
- Chen S, Parmigiani G. Meta-analysis of BRCA1 and BRC A2 penetrance. J Clin Oncol 2007;25:1329-33. [PubMed]
- National Comprehensive Cancer Network. Genetic/familial high-risk assessment: breast and ovarian version4.2013, BR/OV-1.
- Kronowitz SJ. Immediate versus delayed reconstruction. Clin Plast Surg 2007;34:39-50. [PubMed]
- Zakaria S., Degnim AC. Prophylactic mastectomy. Surg Clin North Am 2007;87:317-31. [PubMed]
- Harris RE, Lynch HT, Guirgis HA. Familial breast cancer: risk to the contralateral breast. J Natl Cancer Inst 1978;60:955-60. [PubMed]
- Rosen PP, Groshen S, Kinne DW, et al. Contralateral breast carcinoma:an assessment of risk and prognosis in stage I (T1N0M0) and stage II (T1N1M0) patients with 20-year follow-up. Surgery 1989;106:904-10. [PubMed]
- Barry M, Sacchini V. When is contralateral mastectomy warranted in unilateral breast cancer? Expert Rev Anticancer Ther 2011;11:1209-14. [PubMed]
- McDonnell SK, Schaid DJ, Myers JL, et al. Efficacy of contralateral prophylactic mastectomy in women with a personal and family history of breast cancer. J Clin Oncol 2001;19:3938-43. [PubMed]