The surgically altered breast: imaging technique and findings
Breast cancer is the most common malignancy of women in most western countries including Thailand and other developing countries. According to the World Health Organization 521,000 died of breast cancer in 2012. In Thailand Breast Cancer is the most common malignancy found in women (37.5%) follow by cervical cancer (14.4%) and colorectal cancer (9.6%) (1).
Early Diagnosis of breast cancer is the most importance factor that improve prognosis. Mammography is currently the best imaging modality for early detection of breast cancer and the result of several studies have demonstrated that mammographic screening can decreased the mortality rate due to breast cancer (2,3).
As for breast augmentation surgery, there is no definite evidence that support the association between implants and cancer risk but they can interfere with cancer detection (4). The prevalence of breast cancer in patient with breast implant is similar to the one found in general population. The distribution of cancers by stage in women with breast implants is also similar to that of screened populations, and there is no significant difference in breast cancer survival rates between women with and those without implants (5).
There are many different methods used for augmentation and reconstruction of the breast, which can be divided into three different groups: (I) autogenous tissue transplantation; (II) injectable materials; and (III) implanted prostheses (6). Therefore imaging appearances of breast augmentation and other surgical altered breast are diverse and it is important to be familiar with the spectrum of these appearances to prevent image misinterpretation.
These articles will review technique and spectrum of imaging findings in post surgical altered breast including breast augmentation, reduction mammoplasty and conservatively treated breast.
Breast augmentation
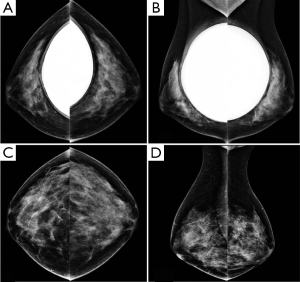
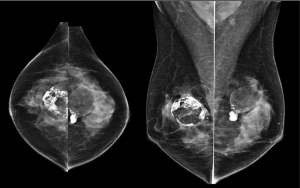
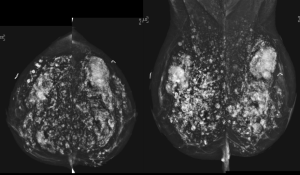
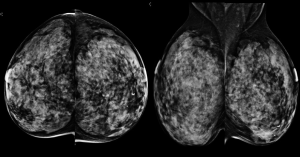
Regular mammography screening after breast implant is recommended at interval appropriate for the woman’s age. Special views called implant-displaced (ID) views have been developed to better visualize the breast tissue anterior to a silicone breast implant.
For silicone gel and saline implant, there are numerous changes that can potentially occur after implant placement such as implant deformity, herniation or rupture of implant. The presence of silicone outside the implant is a clear proof of implant rupture visible on mammography. In general, MRI seems to be the best imaging modality to evaluating implant (Figures 1-4).

Mammoplasty
Preoperative mammography for all women undergoing reduction mammoplasty is important to detect a lesion that requires further investigation or removal at the time of the reduction procedure.
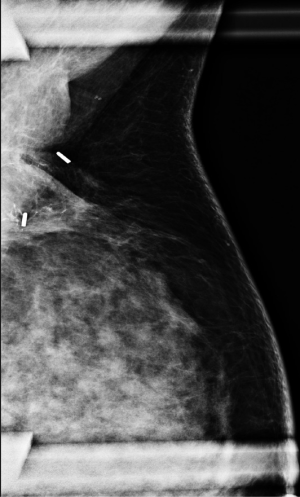
Characteristic mammographic changes have been reported after reduction mammoplasty. Regardless of the exact type of reduction procedure performed, the changes reflect the removal and repositioning of breast tissue and the nipple-areolar complex (6) (Figure 5).
The common mammographic findings include:
- Alteration of breast contour
- Elevation of the nipple
- Displacement of breast parenchyma
- Architectural distortion
- Skin thickening
- Retroareolar fibrotic band
- Disruption of subareolar ducts
- Fat necrosis
Conservatively treated breast
In order to evaluate the treatment options the patient will undergo preoperative imaging. An intraoperative specimen radiography is useful to assessing adequacy of tumor resection and extention of calcification at the time the patient is in the operating room.
A post-operative imaging evaluation is then performed to look for residual tumor, calcification or tumor recurrence. The early diagnosis of recurrence is extremely importance because early detection of the recurrent tumor leads to improved survival likelihood (7) (Figure 6).
For post surgical altered breast, it is helpful to have a mammogram performed 6-12 months after surgery to re-establish baseline findings.
It should be remembered that both benign and malignant processes can coexist in the treated breast. When it is not possible to determine whether the findings are due to carcinoma, fibrosis or other benign processes, biopsy should be performed.
Acknowledgements
The author would like to thank the kind support from Chairman of Thanyarak Breast Center, Siriraj Hospital, Dr. Tamnit Ansusinha and all colleagues.
Disclosure: The author declares no conflict of interest.
References
- National Cancer Institute, Department of Medical Services, Ministry of Public Health. Hospital-Based Cancer Registry, Thailand 2011.
- Kopans DB. Mammography screening is saving thousands of lives, but it survive medical malpractice? Radiology 2004;230:20-4. [PubMed]
- Tabár L, Vitak B, Chen HH, et al. Beyond randomized controlled trials: organized mammographic screening substantially reduces breast cancer mortality. Cancer 2001;91:1724-31. [PubMed]
- Kopans DB. Breast Imaging. 3rd ed. Philadelphia: Lippincott williams & wilkins, 2007.
- Bryant H, Brasher P. Breast implants and breast cancer--reanalysis of a linkage study. N Engl J Med 1995;332:1535-9. [PubMed]
- Bassett LW, Mahoney MC, Apple SK, et al. The surgically altered breast. Breast Imaging. Philadelphia: Saunders, 2011.
- Dershaw DD, Bracha A. The conservatively treated breast. Breast Imaging. Philadelphia: Saunders, 2011.


