
Day case parathyroidectomy: is this the right way for the patients?
Introduction
As demonstrated in the literature (1-6), minimally-invasive video-assisted parathyroidectomy (MIVAP) can be considered the treatment of choice for single parathyroid adenoma. In the major hospitals of the United States and in a few other countries, this technique is performed in a day surgery (DS) setting (7-9), even on adolescents (10), with high rates of success and a low incidence of complications. MIVAP is often associated with regional anaesthesia (RA) (11-13), because of the advantages compared with general anaesthesia (GA), including: continuous and direct monitoring of the recurrent laryngeal nerve, better postoperative pain control, and lower risk of postoperative nausea and vomiting (PONV). Owing to these advantages, elderly and/or high-risk patients can be more easily included as candidates to the operation (14).
MIVAP with RA was introduced in Italy in 2002 (11) but has been typically performed as an inpatient procedure. We believe it is time to perform this operation as a day case in our country as well.
Aim of study
Many studies have already reported the feasibility and safety of MIVAP in DS. Therefore, here our focus has been on the patient’s personal experience with these procedures through an assessment of their recovery at home. The first set of outcome measures of interest included the quality of care provided and to the well-being of the patient: information received, pain, PONV, and resumption of activities of daily living and work. The second set of outcome measures were related to the patient’s safety: complications at home, the need for medical advice and assistance, and unscheduled admissions.
Methods
After Local Ethics Committee approval, we conducted a prospective observational study in the University Hospital of Pisa Day Surgery Unit. Between June 2015 and November 2017, 48 patients were enrolled according to the following inclusion criteria:
- Anaesthesiology: outpatient criteria, age between 18 and 80 years, American Society of Anaesthesiologists (ASA) Classification I to III, no psychiatric disorders, no chronic therapy with anti-inflammatory drugs, and no osteo-articular pathologies or recent traumas in the cervical region.
- Surgical: no familial forms of hyperparathyroidism, preoperative ultrasonographic localization of adenoma, no previous neck surgery or irradiation, and no suspicion of thyroiditis or malignancy.
Patients were divided by personal choice of anaesthesia technique: a regional anaesthesia group (RAg) and general anaesthesia group (GAg). As supported in other studies (15), the patient’s emotional state is essential in this kind of procedure, so we, therefore, considered patient preference a better strategy than randomization.
Written informed consent to the study procedures was obtained from each patient. Data were extracted from the medical records and from three questionnaires: the first was self-compiled at discharge (Q1), while the second (Q2) and the third (Q3) were administered as a telephone survey, respectively the next day and after 4 weeks (Table 1). Most variables were rated as a score from 0 to 4 points. Some questions could be answered “yes” or “no”, and for others, the reference times (e.g., time of discharge) were recorded. Finally, the pain was assessed with the Numerical Rating Scale (NRS) as: 9 to 10, severe; 7 to 8, poorly controlled; 4 to 6, controlled; 1 to 3, well-controlled; 0 absent.
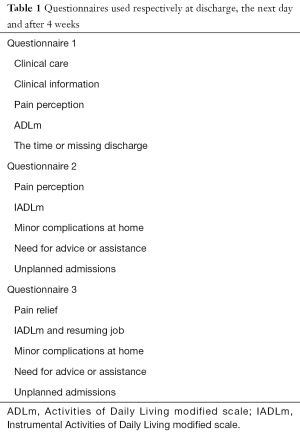
Full table
Anaesthesia technique
In RAg, a bilateral deep cervical block and an infiltration along the incision line was performed with a total of 30 mL of a mixture of lidocaine 2% (10 mL), ropivacaine 1% (10 mL), and levobupivacaine 0.75% (10 mL). A bilateral block was preferred to improve pain control and to permit exploration of the other side, if necessary, since this does not imply a greater risk (14,15). Remifentanil was used to provide mild intravenous sedation (0.05–0.10 µg/kg/min). During the operation, the patient remained in a spontaneous breath, conscious, and contactable.
In GAg, total intravenous anaesthesia was performed. GA was induced with propofol (2 mg/kg) and remifentanil (0.50 µg/kg/min), then maintained with the same drugs, respectively, at 4 mg/kg/h and 0.30 µg/kg/min. A laryngeal mask (LM) was used to secure the airways and ventilate the patient. At induction, ondansetron (4 mg) and dexamethasone (8 mg) were administered for anti-emetic purposes. Both groups received ketorolac (30 mg) and acetaminophen (1 g) for analgesia. The same drugs were administered in the ward 4 hours after the operation. Patients were discharged at home when they reached a modified Post-Anaesthetic Discharge Scoring System (PADSS) score of at least 9 points.
Surgical technique
All patients in both groups undergone MIVAP procedure. A 1.5-cm transverse minicervicotomy is performed 2 cm above the sternal notch, no skin flap is required, the anterior cervical fascia is opened for 2–3 cm on the midline, and the thyroid gland is exposed. Once reached the thyroid gland, infrahyoid muscles homolateral to the suspicious parathyroid gland is dissected from the thyroid lobe; the thyroid lobe is then retracted medially, and the strap muscles are retracted laterally. A 5-mm, 30-degree endoscope, is inserted through the cervicectomy to explore both the parathyroid of the same side. Once enlarged parathyroid is found, a blunt dissection plus a single ligation are performed for its removal. All patients of the study undergone parathyroid hormone (PTH) intraoperative assay by means of a preoperative PTH level (time 0') and an intraoperative PTH level 5 minutes later than the parathyroid gland removal (time +5') in order to prove a 50% PTH level decrease. If the PTH 50% level dropdown is not obtained, the contralateral side exploration is possible with the same surgical steps.
Statistic analysis
This study was conducted on a per-protocol basis. A descriptive analysis of data was performed using means and standard deviations for continuous variables. Statistical significance was evaluated using Fisher two-tailed tests, with an α error of 0.05. Qualitative and ordinal variables are expressed as percentages and measures of frequency.
Results
Of the total patients, 44 were women (91.7%), and 4 were men (8.3%). Mean age was 56.65±12.09 years (range, 30–79 years), with RAg aged 55.47±11.75 years (range, 30–79 years) and GAg aged 59.5±12.86 (range, 40–77 years). There were 34 patients (70.8%) in the RAg and 14 (29.2%) the GAg. Two patients were transferred to the Surgical Unit for an overnight stay, and another patient was transferred to the Cardiology Unit and discharged after 48 hours. These three patients were excluded from the study. The remaining 45 patients (32 in RAg and 13 in GAg) were discharged the same day. No patient reported PONV. No cases of regional block failure occurred and none of the surgical cases needed to be converted from RA to GA.
Surgical results
All patients in both groups underwent MIVAP; no bilateral exploration was needed. In the RA, there were 15 right side parathyroid adenomas: 7 superior right and 8 inferior right and 19 left side adenomas (8 superior left and 11 inferior left). In the GAg, there were 7 right side parathyroid adenomas: 3 superior and 4 inferior and 7 were on the left side (2 superior and 5 inferior). The parathyroid adenoma removal was demonstrated by the 50% intraoperative PTH level dropdown in all cases. All patients underwent calcium blood assay on the first postoperative day and on the second postoperative day; in all cases, we collected normal calcium level on the first and second postoperative day.
Pain
Considering the small population, none of whom reported severe pain, we grouped the pain intensity in two categories: absent/well-controlled (NRS, 0 and 1 to 3) and controlled/poorly controlled (NRS 4 to 8). Intraoperative pain was reported as absent in 21 patients (65.7%) and well-controlled in 11 patients (34.3%) of RAg.
Pain at Q1 was better controlled in RAg than GAg (Table 2). In fact, 31 of 32 patients (96.9%) in RAg reported absent/well-controlled pain against 9 of 13 (69.2%) in GAg (P=0.0061). At Q2, all RAg patients (100%) and 11 of 13 GAg patients (84.6%) reported absent/well-controlled pain (P=0.0085; Table 2).
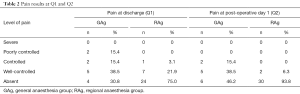
Full table
At Q3, we verified pain relief at home (Table 3). None of the patients in RAg reported pain for longer than 1 day after discharge, whereas 15% of patients in GAg reported pain relief the third day after discharge (P=0.0065).
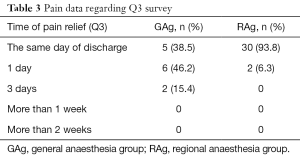
Full table
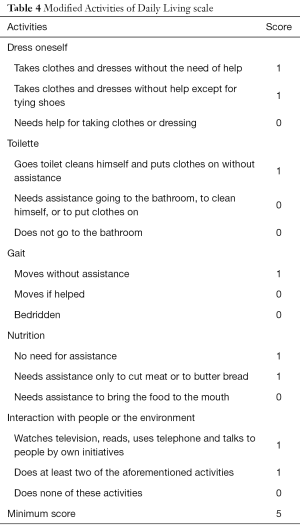
Resumption of basic activities and cognitive function in the hospital
During hospitalization, recovery of autonomy was assessed with the Activities of Daily Living modified scale (ADLm, Table 4). The results were 71.9% of patients in RAg ate within 2 hours after surgery and 28.1% within 3 hours, whereas 84.6% patients in GAg ate within 4 hours and 15.4% within 5 hours (P=0.0045; Table 5). Return of cognitive function was also faster in RAg: 93.8% of patients within 2 hours, 6.2% within 3 hours in RAg, and 15.4% of patients within 2 hours, 69.2% within 3 hours, and 15.4% within 4 hours in GAg (P=0.0107). Discharge in RAg occurred within 3 hours in 12.5% of patients, within 4 hours in 78.1%, and within 5 hours in 9.4%. Discharge in GAg occurred within 5 hours in 53.8% and more than 5 hours in 46.1% (P=0.0027).
Full table
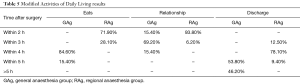
Full table
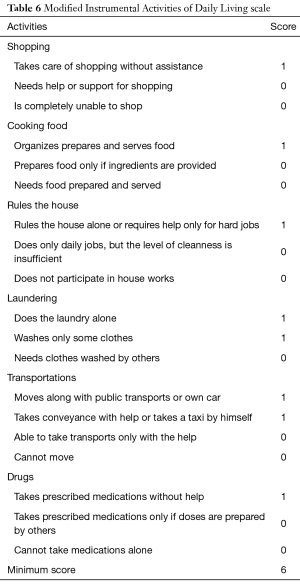
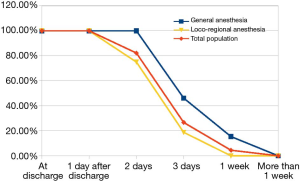
Resumption daily activities at home and work
Self-sufficiency at home was evaluated with Instrumental Activities of Daily Living modified scale (IADLm, Table 6). None of the patients regained complete self-sufficiency the first day after discharge. The next day, the RAg reached score of 5 in 43.7% of patients, 4 in 46.9%, and 2 in 9.4%, and the GAg scores were 4 in 38.5% of patients, 2 in 46.1%, and 0 in 15.4% (P=0.025). We did not find statistically significant differences between the two groups at Q3. However, we point out that 25% of the Rag patients were autonomous at the end of the second day after discharge, reaching 100% within a week. Conversely, in the GAg, 53.8% began to be self-sufficient after 3 days and 100% reached self-sufficiency after 1 week (Figure 1).
Full table
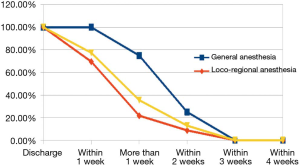
Resumption of work (Figure 2), excluding 31.1% of retired patients, occurred in 30.5% of RAg patients within 1 week, in 47.8% after 1 week, in 13.0% within 2 weeks, and in 8.7% within 3 weeks. Resumption for the GAg occurred in 25% after 1 week, in 50% within 2 weeks, and in 25% within 3 weeks. The difference between the two groups was significant (P=0.02).
Complications at home
Complications at home and the need for medical care (home visit, telephone advice, visiting a general practitioner), as well as access to the emergency department or unplanned hospitalization, were the same and not statistically significant in the two groups (2 patients in each group reported mild infection at the wound, and 2 reported gastritis). Eventually, symptomatic hypocalcaemia developed at home in RAg patient despite the consumption of calcium prescribed at discharge. No complications were directly dependent on the anaesthetic choice.
Clinical care satisfaction
Clinical care was reported as excellent in 71.9% of RAg patients and good in 28.1% at Q1, whereas GAg patients rated it excellent in 23.1% and good in 76.9%. Statistics were comparable between the two groups. At Q2 in the RAg, satisfaction was reported as excellent in 96.8% and good in 3.2%, and in GAg excellent in 69.2%, good in 23.1%, and enough in 7.7% (P=0.02).
At Q3, we asked patients whether they would return to our department in case of necessity or whether they would advise MIVAP to others. The response was an absolute yes in 96.9% of RAg patients and yes in 3.1%, whereas the response in GAg patients was an absolute yes in 61.5%, yes in 23.1%, and probably in 15.4% (P=0.018).
Discussion
The literature agrees on the feasibility and safety of MIVAP in DS performed in RA, considering it superior also to open techniques in some respects. Furthermore, reduced health care expenditure is another reason to prefer it. But what is the patient’s perception? Beyond the clinical outcome, is this the right way for the patient? Everything that happens in a hospital has a personal meaning for the patient, compared with the biological significance attributed by physicians (16). We, therefore, focused on the personal sense of hospitalization: perception of the quality of care and well-being (level of treatments and information received, pain, PONV, resumption of ADL), as well as patient safety (need for counselling or assistance, complications, unplanned hospitalization).
Pain
Intraoperative pain control in RAg was very satisfactory, confirming the efficacy of the technique: 65.7% of patients reported the absence of pain, and 34.3% indicated pain as controlled.
According to literature (3,11), postoperative pain assessment was lower in the RAg (P=0.0061) than in the GAg, despite the use of LM rather than an endotracheal tube. This choice permitted a decreased risk of severe coughing at the time of extubating and then of bleeding. The subsequent home survey confirmed the best results in the RAg for pain perception (Q2: P=0.0085) and on faster resolve (Q3: P=0.0065). Our data, therefore, confirm the efficacy of cervical block and intravenous sedation in this kind of operation, reducing pain, PONV, and complications that delay patient well-being and discharge.
Self-sufficiency at hospital and home, work resumption
To evaluate the resumption of ADL and human relations, we modified the Katz scale and Lawton-Brody scale (17-20). They are usually used to assess motor and psychologic skills in people with reduced ability and in the elderly, as well as in occupational therapy to check the patient’s progress in recovering from illness or injury. Changing some voices and deleting others, we adapted the scales (ADLm, IADLm) to the study context. Values obtained and the time taken to reach the minimum score of (5 for ADLm and 6 for IADLm) confirm the superiority of RA compared with GA. Thanks to the reduced psychophysical effect of local anaesthesia, the RAg patients ate earlier (P=0.0045), regained cognitive function and resumed human relationships more quickly (P=0.0107), and were discharged in a shorter time (P=0.0027) compared with the GAg patients, with better results than reported by other studies (21). Despite the use of the LM and short-term drugs (propofol and remifentanil), the prevalence of RA over GA was confirmed for other ADLm and IADLm entries, although they were not statistically significant. All patients returned to their work within 4 weeks, although RAg patients did so more rapidly in the first days after discharge (P=0.02). Eventually, we believe our study shows that RA guarantees greater well-being than GA.
Missing discharge
Three patients were admitted as inpatients for prolonged observation and were dropped from the study. One patient showed signs of heart failure in the afternoon, was transferred to the Cardiology Unit, and was discharged after 48 hours with a diagnosis of Takotsubo disease. The other two patients underwent the operation with an unclear diagnosis: parathyroid was found deep in the mediastinum in one patient, and thyroidectomy was associated with the other patient. Because the operations in both patients extended beyond 2 hours and the bleeding risk, they were transferred to the Surgery Unit and discharged the following morning. Considering these instances were not directly related to procedures, we can conclude that the care pathway is feasible and safe.
Complications at home
We considered complications at home not dangerous for the patient’s safety, but rather that could influence the quality of recovery, including mild respiratory disorders (e.g., hoarseness), gastritis, PONV, local edema, or infection. The only true complication recorded was symptomatic hypocalcaemia in one patient, despite calcium integration from the day after the operation (22,23). The patient went to the Emergency Department and was discharged in a few hours. No other complication occurred, and the care at home was limited to telephone counselling with surgeons or one or more accesses to the general practitioner. This confirms what has been highlighted in the literature on the safety of this procedure. No unplanned readmission to the hospital was necessary.
Clinical care satisfaction
The collected data at the Q3 survey showed the satisfaction of all patients for the clinical care received. Once again, however, the RAg patients were more satisfied then GAg patients (P=0.02), for pain relief and short duration, as well as for the feeling of well-being and quick recovery of autonomy after surgery.
Finally, all RAg patients would have made the same care path, whereas a small number of GAg patients (15.38%) appeared doubtful because the pain control was not perfect, and the pain lasted for some days.
Conclusions
Although the study was conducted on a small sample, the data showed that patients highly appreciated day-case parathyroidectomy. This is due to the quality of care provided and to well-being after the operation. Furthermore, the study demonstrates, at the parity of security, that the association of RA with MIVAP leads to better results than the association of GA and MIVAP.
Finally, we point out that, beyond the clinical ability and knowledge, it is fundamental that the physicians pay attention to what the patients consider important for them; that is, the personal meaning of the hospitalization.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the local ethics committee (No. 12450) and written informed consent was obtained from all patients.
References
- Bakkar S, Matteucci V, Corsini C, et al. Less is more: time to expand the indications for minimally invasive video-assisted parathyroidectomy. J Endocrinol Invest 2017;40:979-83. [Crossref] [PubMed]
- Melfa GI, Raspanti C, Attard M, et al. Comparison of minimally invasive parathyroidectomy under local anaesthesia and minimally invasive video-assisted parathyroidectomy for primary hyperparathyroidism: a cost analysis. G Chir 2016;37:61-7. [PubMed]
- Rio PD, Vicente D, Maestroni U, et al. A comparison of minimally invasive video-assisted parathyroidectomy and traditional parathyroidectomy for parathyroid adenoma. J Cancer 2013;4:458-63. [Crossref] [PubMed]
- Garimella V, Yeluri S, Alabi A, et al. Minimally invasive video-assisted parathyroidectomy is a safe procedure to treat primary hyperparathyroidism. Surgeon 2012;10:202-5. [Crossref] [PubMed]
- Gracie D, Hussain SS. Use of minimally invasive parathyroidectomy techniques in sporadic primary hyperparathyroidism: systematic review. J Laryngol Otol 2012;126:221-7. [Crossref] [PubMed]
- Augustine MM, Bravo PE, Zeiger MA. Surgical treatment of primary hyperparathyroidism. Endocr Pract 2011;17:75-82. [Crossref] [PubMed]
- Stack BC Jr, Moore E, Spencer H, et al. Outpatient thyroid surgery data from the University Health System (UHC) Consortium. Otolaryngol Head Neck Surg 2013;148:740-5. [Crossref] [PubMed]
- Dulfer RR, van Ginhoven TM, Geilvoet W, et al. Operative Treatment of Primary Hyperparathyroidism in Daycare Surgery. Scand J Surg 2015;104:196-9. [Crossref] [PubMed]
- Rajeev P, Sutaria R, Ezzat T, et al. Changing trends in thyroid and parathyroid surgery over the decade: is same-day discharge feasible in the United Kingdom? World J Surg 2014;38:2825-30. [Crossref] [PubMed]
- Langusch CC, Norlen O, Titmuss A, et al. Focused image-guided parathyroidectomy in the current management of primary hyperparathyroidism. Arch Dis Child 2015;100:924-7. [Crossref] [PubMed]
- Miccoli P, Barellini L, Monchik JM, et al. Randomized clinical trial comparing regional and general anaesthesia in minimally invasive video-assisted parathyroidectomy. Br J Surg 2005;92:814-8. [Crossref] [PubMed]
- Cohen MS, Finkelstein SE, Brunt LM, et al. Outpatient minimally invasive parathyroidectomy using local/regional anesthesia: a safe and effective operative approach for selected patients. Surgery 2005;138:681-7. [Crossref] [PubMed]
- Materazzi G, Rago R, Berti PF, et al. Paratiroidectomia mini-invasiva con blocco del plesso cervicale. In: Trattato Italiano di Endocrinochirurgia. vol. II, Publisher: L. Rosato, Editors: GS, 2008:541-3.
- Fang WL, Tseng LM, Chen JY, et al. The management of high-risk patients with primary hyperparathyroidism - minimally invasive parathyroidectomy vs. medical treatment. Clin Endocrinol (Oxf) 2008;68:520-8. [Crossref] [PubMed]
- Sanjay P, Marioud A, Woodward A. Anaesthetic preference and outcomes for elective inguinal hernia repair: a comparative analysis of public and private hospitals. Hernia 2013;17:745-8. [Crossref] [PubMed]
- Kiernan CM, Schlegel C, Isom C, et al. Ambulatory bilateral neck exploration for primary hyperparathyroidism: is it safe? Am J Surg 2016;212:722-7. [Crossref] [PubMed]
- Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged. the index of ADL: a standardized measure of biological and psychosocial function. JAMA 1963;185:914-9. [Crossref] [PubMed]
- Katz S, Downs TD, Cash HR, et al. Progress in the development of the index of ADL. Gerontologist 1970;10:20-30. [Crossref] [PubMed]
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9:179-86. [Crossref] [PubMed]
- Kopp VJ, Shafer A. Anesthesiologists and perioperative Communication. Anesthesiology 2000;93:548-55. [Crossref] [PubMed]
- Meltzer C, Klau M, Gurushanthaiah D, et al. Safety of Outpatient Thyroid and Parathyroid Surgery: A Propensity Score-Matched Study. Otolaryngol Head Neck Surg 2016;154:789-96. [Crossref] [PubMed]
- Udelsman R. Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg 2002;235:665-70; discussion 670-2. [Crossref] [PubMed]
- Gurnell EM, Thomas SK, McFarlane I, et al. Focused parathyroid surgery with intraoperative parathyroid hormone measurement as a day-case procedure. Br J Surg 2004;91:78-82. [Crossref] [PubMed]


