The prognostic implication and potential role of BRAF mutation in the decision to perform elective neck dissection for thyroid cancer
Introduction
Papillary thyroid cancer (PTC) is the most common thyroid malignancy (1,2). Although PTC generally follows an indolent course with an excellent prognosis, lymph node metastases (LNMs), especially to the central compartment (level VI), are common and occur in an average of 60% of cases (3-5). LNM is commonly associated with an increased rate of locoregional recurrence in patients with PTC (6,7). The performance of therapeutic central neck dissection (CND) is generally accepted in patients with PTC with clinical evidence of lymph node involvement in the central compartment. However, prophylactic CND in clinically node-negative central necks remains controversial because of the limited survival benefit and an increasing rate of complications associated with the procedure (8,9). Unfortunately, methods with which to preoperatively assess the presence of central LNM preoperatively have not been established. Although ultrasonography and intraoperative assessment can help to identify grossly apparent LNM, both modalities have low sensitivity for the detection of central LNM (10,11). Therefore, many researchers have reported the identification of various factors (larger tumors, extrathyroidal extension, and aggressive histological subtypes) associated with occult metastasis to the central compartment to avoid unnecessary CND (12). However, some factors such as extrathyroidal extension and aggressive histological subtypes, associated with occult metastasis to the central compartment, can’t help in the decision regarding prophylactic CND because these factors are clear only postsurgical histology.
Many recent studies have reported that the BRAF V600E mutation is a novel prognostic marker that may be useful for risk stratification. The BRAF V600E mutation is the most common genetic change in patients with PTC, being observed in 30-80% of all cases (13-16). Among the various histological subtypes of PTC, conventional and tall-cell variants are most commonly associated with the mutation (67-68% and 80-83%, respectively); the mutation is least associated with the follicular variant (12-18%) (17,18). Detection of the BRAF V600E mutation in fine needle aspiration biopsy (FNAB) specimens may be useful for confirming or establishing the preoperative diagnosis of PTC (19-21), and the mutation has been associated with aggressive tumor characteristics or poor prognostic factors (22-26). Furthermore, some studies have examined the utility of preoperative detection of the BRAF V600E mutation for optimizing the surgical management of PTC and have suggested that BRAF-positive patients may benefit from a more extensive initial surgery, including the performance of CND (27,28). However, these issues remain very controversial.
Therefore, we reviewed the currently available literature regarding the prognostic and therapeutic role of the BRAF V600E mutation, especially its potential role in the decision to perform elective neck dissection for PTC.
Studies published in English were identified from PubMed and the Cochrane Register of Controlled Trials up to October 2013 with the search terms such as ‘BRAF mutation’, ‘neck dissection’, ‘LNM’ and ‘papillary thyroid carcinoma’.
The BRAF V600E mutation as a prognostic factor
Several clinicopathological risk factors have been used for stratifying PTC, including older age of patients at diagnosis, larger tumor size, cervical LNM, extrathyroidal invasion, distant metastasis, and advanced disease staging (29-31). Many recent studies have shown an association between the BRAF V600E mutation and aggressive clinicopathological characteristics of PTC, including LNM, extrathyroidal invasion, loss of radioiodine avidity, and failure of radioiodine treatment and resultant disease recurrence (22,32). Consequently, the mutation has drawn considerable attention and interest as a potential prognostic factor for PTC.
Kebebew et al. followed 314 patients with thyroid cancer prospectively for a median of six years and found that the BRAF V600E mutation was independently associated with recurrent and persistent PTC (24). Lupi et al. evaluated retrospectively 500 patients with PTC, 43% of whom had the mutation, and found that those patients had a higher incidence of extrathyroidal extension, nodal metastasis, multicentricity, and advanced tumors than patients without the mutation (33). Kim et al. suggested in prospective study that the mutation is associated with a higher clinical recurrence of disease in low-risk patients with conventional PTC (34). An association between the BRAF V600E mutation and disease-specific survival has also been demonstrated. Elisei et al. retrospectively evaluated a small cohort of PTC patients with a median follow-up of 15 years and observed shorter survival in the group with the mutation (35). Xing et al. investigated the relationship between the mutation and PTC-related mortality in 1,849 patients with PTC. In their retrospective multicenter study, the presence of the mutation was significantly associated with increased cancer-related mortality among patients with PTC (36). On the other hand, some investigators have shown that the BRAF V600E mutation is not associated with aggressive features in patients with PTC. Sancisi et al. reported in retrospective study that the mutation is not associated with the development of distant metastases or fatal outcomes in patients with PTC and may not predict aggressive behavior (37). Trovisco et al. reported in retrospective study that BRAF-mutated PTC does not exhibit signs of higher aggressiveness (size, vascular invasion, extrathyroid extension, and nodal metastasis) and is in fact less often multicentric than without the mutation (38).
Although most studies that have reported an association between the BRAF V600E mutation and poor prognostic features are impressive, some of the data are retrospective, and the BRAF V600E status has not yet been incorporated into a standard PTC management algorithm. It remains unclear whether identification of the BRAF V600E mutation in isolation, regardless of the presence or absence of other clinicopathologic characteristics, should prompt clinicians to treat patients with PTC with more aggressive adjuvant therapies and/or closer long-term surveillance. Further study in this regard is required.
The BRAF V600E mutation as a measure of surgical extent
The BRAF V600E mutation is associated with a higher risk of progression in patients with PTC. However, it is not yet known whether preoperative BRAF V600E analysis in cytologic specimens may aid the determination of surgical extent and thus facilitate prophylactic CND for occult central neck LNM in patients with PTC and a clinically node-negative neck. Many studies have investigated the role of the mutation in the decision of the most optimal initial surgical extent, including prophylactic CND for PTC.
Many researchers have reported that preoperative identification of the BRAF V600E mutation may guide not only the initial extent of total thyroidectomy, but also the need for and extent of lymphadenectomy. Yip et al. compared the clinical, cytologic, and pathologic parameters of 106 consecutive surgically treated patients with BRAF-positive PTC with a concurrent cohort of 100 patients with BRAF-negative PTC (17). All patients was not performed initially routine CND (17). Eleven of the positive patients required reoperation for recurrent/persistent disease compared to three negative patients (P=0.04). Preoperative knowledge of BRAF V600E mutation positivity could have improved the initial surgical management of 24% of the patients. Therefore, they suggested that BRAF V600E mutations are associated with cervical recurrence and reoperation. They also insisted that preoperative cytologic identification of the BRAF V600E mutation has high specificity and may guide the initial extent of thyroidectomy and node dissection (17). Similarly, Xing et al. compared the clinical and pathologic parameters of 73 surgically treated patients with BRAF-positive PTC with a concurrent cohort of 117 patients with BRAF-negative PTC (39). In this study, CND was typically performed for treatment of lymph nodes that were suggestive of abnormality on intraoperative examination (39). They insisted that preoperative testing for the mutation in FNAB specimens provides a novel tool with which to preoperatively identify patients with PTC at higher risk for extensive disease (extrathyroidal extension and LNMs) and those who are more likely to show persistence/recurrence (39). In addition, they asserted that the BRAF V600E mutation, as a powerful prognostic risk marker, may be useful for appropriately tailoring the initial surgical extent for patients with PTC (39). We recently investigated whether preoperative BRAF V600E analysis may aid the determination of surgical extent, including prophylactic CND with variable clinicopathological risk factors for central LNM, in patients with PTC and a clinically node-negative neck (28). Our multivariate analysis showed that a tumor size of >1 cm [P=0.006; odds ratio (OR), 3.559], perithyroidal invasion (P=0.023; OR, 2.893), and preoperative positivity for the BRAF V600E mutation (P=0.029; OR, 2.727) were independent risk factors for the presence of occult central LNM. Therefore, we suggested that preoperative BRAF V600E analysis by FNAB and determination of primary tumor size based on ultrasonography may help predict occult central LNM in patients with PTC and a clinically node-negative neck (28). Alzahrani et al. reviewed records of 379 patients of PTC who underwent total or near-total thyroidectomy with or without CLN dissection (40). They reported that cervical LNMs found at the time of CND are closely associated with disease recurrence/persistence of PTC, both of which are strongly predicted by the BRAF V600E mutation (40). Therefore, they suggested that preoperative testing for the BRAF V600E mutation in thyroid needle biopsy specimens in combination with other conventional risk factors to determine the aggressiveness of CND may be a reasonable approach (40). Howell et al. investigated retrospectively records of 156 patients of PTC (41). Patients with suspicious or preoperatively detected LNM received a therapeutic CND (41). A prophylactic CND was performed for BRAF V600E mutation positive status without clinically or sonographically evident disease (41). They insisted that of the commonly used clinical parameters available preoperatively, the BRAF V600E mutation is the only independent predictor of central lymph node dissection in PTC and can be utilized to guide the extent of the initial surgery (41). So et al. investigated 71 patients with PTC prospectively (42). All patients were performed total thyroidectomy and CND (42). They reported that the mutation was a significant predictor of LNM, and that the mutation may have differential predictive values for LNM according to tumor size (42).
On the other hand, Barbaro et al. studied 110 patients with PTC who underwent BRAF analysis of FNAB specimens prospectively (43). In this study, total thyroidectomy and routine CND independent of BRAF V600E mutation was performed, and reported that the mutation did not appear to be a reliable risk factor for tumor aggressiveness (43). Therefore, they suggested that BRAF V600E analysis should not be the only guide for presurgical decisions regarding the extent of surgery or postsurgical decisions regarding the aggressiveness of the treatment (43). Lee et al. conducted a small series that included only 63 patients with PTC and underscored the prematurity of utilizing BRAF V600E mutation status to determine the surgical management of patients with PTC, specifically whether or not to perform CND (44). They suggested that prospective, multi-institutional studies that include only patients preoperatively known to have PTC and centers in which routine CND is performed are therefore greatly needed before we can accurately assess whether BRAF V600E mutation status should be incorporated into critical decisions regarding the appropriate operative management of patients with PTC. Dutenhefner et al. compared the clinical and pathologic parameters of 15 surgically treated patients with BRAF-positive PTC with a concurrent cohort of 36 patients with BRAF-negative PTC (45). In this study, total thyroidectomy and routine CND was performed (45). They showed that LNM is related to multifocality, angiolymphatic invasion, and age, but not to the BRAF V600E mutation, and concluded that BRAF V600E is not a helpful tool for deciding whether to perform elective neck dissection of the central compartment. Table 1 outlines the case series evaluating the role of the BRAF mutation in the decision to perform prophylactic CND in patients with PTC.
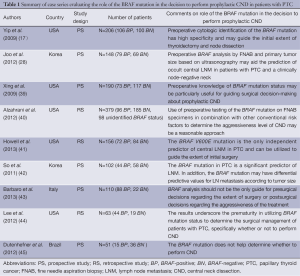
Full table
In summary, many studies have evaluated whether preoperative analysis of the BRAF V600E mutation and other risk factors may help delineate which patients with PTC should undergo prophylactic concurrent CND at the time of thyroidectomy because currently available methods, including ultrasonography, have been shown to be inaccurate for preoperatively identifying metastatic lymph nodes in the central compartment. However, the role of preoperative assessment of the BRAF V600E mutation status in decisions regarding the most optimal surgical extent in patients with PTC remains controversial. In the future, a prospective randomized study of a large population should be performed with a long-term follow-up period to assess the potential role of preoperative assessment of BRAF V600E mutation status in decisions regarding whether to perform prophylactic CND in patients with PTC.
Conclusions
Numerous studies have evaluated whether there is correlation between the BRAF V600E mutation and its usefulness as a prognostic factor for patients with PTC. In addition, many studies have attempted to confirm the value of the BRAF V600E mutation as a measure of the extent of surgery. Most reports agree that the mutation is associated with tumor aggressiveness, a poor prognosis, resistance to postoperative radioiodine therapy, and the need for a more extended surgery. However, the potential role of the preoperative assessment of BRAF V600E mutation status in decisions regarding whether to perform prophylactic CND remains controversial. When the necessity of prophylactic CND in patients with PTC is preoperatively determined, we should recommend to perform prophylactic CND if BRAF V600E mutation and other conventional clinical risk factors are coexistent.
Acknowledgements
Disclosure: This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MEST) (Grant number: 2012R1A1A2005393, 2013R1A2A2A01015281).
References
- Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA 2006;295:2164-7. [PubMed]
- Jemal A, Siegel R, Xu J, et al. Cancer statistics, 2010. CA Cancer J Clin 2010;60:277-300. [PubMed]
- Mirallié E, Visset J, Sagan C, et al. Localization of cervical node metastasis of papillary thyroid carcinoma. World J Surg 1999;23:970-3; discussion 973-4. [PubMed]
- Wada N, Duh QY, Sugino K, et al. Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg 2003;237:399-407. [PubMed]
- Pereira JA, Jimeno J, Miquel J, et al. Nodal yield, morbidity, and recurrence after central neck dissection for papillary thyroid carcinoma. Surgery 2005;138:1095-100, discussion 1100-1. [PubMed]
- Mazzaferri EL, Jhiang SM. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 1994;97:418-28. [PubMed]
- DeGroot LJ, Kaplan EL, McCormick M, et al. Natural history, treatment, and course of papillary thyroid carcinoma. J Clin Endocrinol Metab 1990;71:414-24. [PubMed]
- Henry JF, Gramatica L, Denizot A, et al. Morbidity of prophylactic lymph node dissection in the central neck area in patients with papillary thyroid carcinoma. Langenbecks Arch Surg 1998;383:167-9. [PubMed]
- Lee YS, Kim SW, Kim SW, et al. Extent of routine central lymph node dissection with small papillary thyroid carcinoma. World J Surg 2007;31:1954-9. [PubMed]
- Hwang HS, Orloff LA. Efficacy of preoperative neck ultrasound in the detection of cervical lymph node metastasis from thyroid cancer. Laryngoscope 2011;121:487-91. [PubMed]
- Shen WT, Ogawa L, Ruan D, et al. Central neck lymph node dissection for papillary thyroid cancer: the reliability of surgeon judgment in predicting which patients will benefit. Surgery 2010;148:398-403. [PubMed]
- Iyer NG, Shaha AR. Central compartment dissection for well differentiated thyroid cancer … and the band plays on. Curr Opin Otolaryngol Head Neck Surg 2011;19:106-12. [PubMed]
- Kimura ET, Nikiforova MN, Zhu Z, et al. High prevalence of BRAF mutations in thyroid cancer: genetic evidence for constitutive activation of the RET/PTC-RAS-BRAF signaling pathway in papillary thyroid carcinoma. Cancer Res 2003;63:1454-7. [PubMed]
- Cohen Y, Xing M, Mambo E, et al. BRAF mutation in papillary thyroid carcinoma. J Natl Cancer Inst 2003;95:625-7. [PubMed]
- Xing M.. BRAF mutation in thyroid cancer. Endocr Relat Cancer 2005;12:245-62. [PubMed]
- Espinosa AV, Porchia L, Ringel MD. Targeting BRAF in thyroid cancer. Br J Cancer 2007;96:16-20. [PubMed]
- Yip L, Nikiforova MN, Carty SE, et al. Optimizing surgical treatment of papillary thyroid carcinoma associated with BRAF mutation. Surgery 2009;146:1215-23. [PubMed]
- Nikiforova MN, Kimura ET, Gandhi M, et al. BRAF mutations in thyroid tumors are restricted to papillary carcinomas and anaplastic or poorly differentiated carcinomas arising from papillary carcinomas. J Clin Endocrinol Metab 2003;88:5399-404. [PubMed]
- Handkiewicz-Junak D, Czarniecka A, Jarzab B.. Molecular prognostic markers in papillary and follicular thyroid cancer: Current status and future directions. Mol Cell Endocrinol 2010;322:8-28. [PubMed]
- Pelizzo MR, Boschin IM, Barollo S, et al. BRAF analysis by fine needle aspiration biopsy of thyroid nodules improves preoperative identification of papillary thyroid carcinoma and represents a prognostic factor. A mono-institutional experience. Clin Chem Lab Med 2011;49:325-9. [PubMed]
- Mathur A, Weng J, Moses W, et al. A prospective study evaluating the accuracy of using combined clinical factors and candidate diagnostic markers to refine the accuracy of thyroid fine needle aspiration biopsy. Surgery 2010;148:1170-6; discussion 1176-7.. [PubMed]
- Xing M.. BRAF mutation in papillary thyroid cancer: pathogenic role, molecular bases, and clinical implications. Endocr Rev 2007;28:742-62. [PubMed]
- Frasca F, Nucera C, Pellegriti G, et al. BRAF(V600E) mutation and the biology of papillary thyroid cancer. Endocr Relat Cancer 2008;15:191-205. [PubMed]
- Kebebew E, Weng J, Bauer J, et al. The prevalence and prognostic value of BRAF mutation in thyroid cancer. Ann Surg 2007;246:466-70; discussion 470-1. [PubMed]
- Jo YS, Li S, Song JH, et al. Influence of the BRAF V600E mutation on expression of vascular endothelial growth factor in papillary thyroid cancer. J Clin Endocrinol Metab 2006;91:3667-70. [PubMed]
- Kim J, Giuliano AE, Turner RR, et al. Lymphatic mapping establishes the role of BRAF gene mutation in papillary thyroid carcinoma. Ann Surg 2006;244:799-804. [PubMed]
- Melck AL, Yip L, Carty SE. The utility of BRAF testing in the management of papillary thyroid cancer. Oncologist 2010;15:1285-93. [PubMed]
- Joo JY, Park JY, Yoon YH, et al. Prediction of occult central lymph node metastasis in papillary thyroid carcinoma by preoperative BRAF analysis using fine-needle aspiration biopsy: a prospective study. J Clin Endocrinol Metab 2012;97:3996-4003. [PubMed]
- American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer, Cooper DS, Doherty GM, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009;19:1167-214. [PubMed]
- Tuttle RM, Ball DW, Byrd D, et al. Thyroid carcinoma. J Natl Compr Canc Netw 2010;8:1228-74. [PubMed]
- Brown RL, de Souza JA, Cohen EE. Thyroid cancer: burden of illness and management of disease. J Cancer 2011;2:193-9. [PubMed]
- Kim TH, Park YJ, Lim JA, et al. The association of the BRAF(V600E) mutation with prognostic factors and poor clinical outcome in papillary thyroid cancer: a meta-analysis. Cancer 2012;118:1764-73. [PubMed]
- Lupi C, Giannini R, Ugolini C, et al. Association of BRAF V600E mutation with poor clinicopathological outcomes in 500 consecutive cases of papillary thyroid carcinoma. J Clin Endocrinol Metab 2007;92:4085-90. [PubMed]
- Kim TY, Kim WB, Rhee YS, et al. The BRAF mutation is useful for prediction of clinical recurrence in low-risk patients with conventional papillary thyroid carcinoma. Clin Endocrinol (Oxf) 2006;65:364-8. [PubMed]
- Elisei R, Ugolini C, Viola D, et al. BRAF(V600E) mutation and outcome of patients with papillary thyroid carcinoma: a 15-year median follow-up study. J Clin Endocrinol Metab 2008;93:3943-9. [PubMed]
- Xing M, Alzahrani AS, Carson KA, et al. Association between BRAF V600E mutation and mortality in patients with papillary thyroid cancer. JAMA 2013;309:1493-501. [PubMed]
- Sancisi V, Nicoli D, Ragazzi M, et al. BRAFV600E mutation does not mean distant metastasis in thyroid papillary carcinomas. J Clin Endocrinol Metab 2012;97:E1745-9. [PubMed]
- Trovisco V, Soares P, Preto A, et al. Type and prevalence of BRAF mutations are closely associated with papillary thyroid carcinoma histotype and patients’ age but not with tumour aggressiveness. Virchows Arch 2005;446:589-95. [PubMed]
- Xing M, Clark D, Guan H, et al. BRAF mutation testing of thyroid fine-needle aspiration biopsy specimens for preoperative risk stratification in papillary thyroid cancer. J Clin Oncol 2009;27:2977-82. [PubMed]
- Alzahrani AS, Xing M. Impact of lymph node metastases identified on central neck dissection (CND) on the recurrence of papillary thyroid cancer: potential role of BRAFV600E mutation in defining CND. Endocr Relat Cancer 2013;20:13-22. [PubMed]
- Howell GM, Nikiforova MN, Carty SE, et al. BRAF V600E mutation independently predicts central compartment lymph node metastasis in patients with papillary thyroid cancer. Ann Surg Oncol 2013;20:47-52. [PubMed]
- So YK, Son YI, Park JY, et al. Preoperative BRAF mutation has different predictive values for lymph node metastasis according to tumor size. Otolaryngol Head Neck Surg 2011;145:422-7. [PubMed]
- Barbaro D, Incensati RM, Materazzi G, et al. The BRAF V600E mutation in papillary thyroid cancer with positive or suspected pre-surgical cytological finding is not associated with advanced stages or worse prognosis. Endocrine 2013. [Epub ahead of print]. [PubMed]
- Lee KC, Li C, Schneider EB, et al. Is BRAF mutation associated with lymph node metastasis in patients with papillary thyroid cancer? Surgery 2012;152:977-83. [PubMed]
- Dutenhefner SE, Marui S, Santos AB, et al. BRAF, A tool in the decision to perform elective neck dissection? Thyroid 2013. [Epub ahead of print]. [PubMed]


