A systematic review of donor site aesthetic and complications after deep inferior epigastric perforator flap breast reconstruction
Introduction
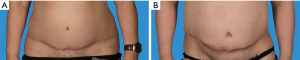
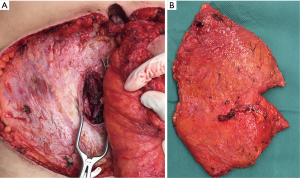
The deep inferior epigastric perforator flap (DIEP) has become a widely performed method for breast reconstruction in the past decade due to its assumed low donor site morbidity and natural aesthetic results (1-3). However, even though morbidity of the abdominal muscular wall itself tends to be lower compared to the harvest of a transversus rectus abdominis muscle flap (TRAM) (4-6), the aesthetic of the abdominal donor site are often a cause of dissatisfaction (Figure 1) (7). The resulting long transverse scar is frequently placed relatively high on the abdomen or appears to “migrate” up during the postoperative course, making it visible and difficult to hide by undergarments (8). Since DIEP flaps are increasingly performed in less suited patients resulting in closure of the donor site under tension, wound healing complications have the tendency to occur more frequently (9). In addition, scars may be hypertrophic, atrophic, widened, retracted or asymmetrical and visible lateral fat depots or dog-ears may result. A number of patients also report pain in the scar area when wearing tight pants, belts etc.
To overcome those unfavourable donor site results some authors proposed to routinely perform aesthetic revision surgery on the abdominal scar during breast touch-up procedures (fat grafting, nipple-areola reconstruction, etc.) during the second stage of breast reconstruction (8). Others have designed a lower DIEP pattern, which may be associated with a higher flap complication rate due to the necessity to choose low and potentially not optimal perforators (10) or to include higher perforators by skin undermining (11).
However, so far only little attention has been given to the aesthetic aspect of the DIEP donor site, since the understanding of less-invasive, and thus more tedious harvesting techniques were the main focus of reconstructive surgeons in the past decade. After establishment of these concepts, the focus must change given the fact that the number of breast reconstructions increases and the patients` expectations rise.
Based on this, the aim of this study was to identify crucial factors influencing donor site aesthetic and evaluate present recommendations for donor site improvement by performing a systematic review of the existing literature. A secondary goal was to evaluate the morbidity of the abdominal wall and donor site complications after a DIEP flap harvest.
Methods
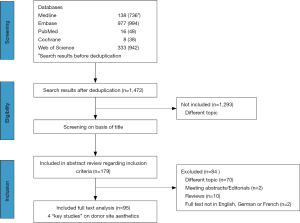
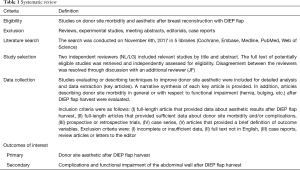
We performed a systematic review in accordance to the PRISMA guidelines (12) (Table 1). A review protocol was designed and registered on PROSPERO, the international prospective register of systematic reviews http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018083859.
Full table
Study selection
A literature research was conducted on November 6th 2017 using the following databases: Medline, Embase, PubMed, Cochrane, and Web of Science. Language was restricted to English, German and French. For search terms and details of the systematic review, see the Appendix (Table S1).
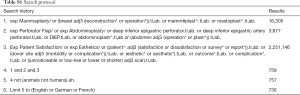
Full table
Inclusion and exclusion criteria
All studies on aesthetic and complications of the donor site after DIEP flap harvest for breast reconstruction were included in a qualitative analysis. Clinical studies on other topics related to breast reconstruction, e.g., breast reconstruction with other flaps or with silicone implants were excluded. Reviews and experimental research (i.e., anatomical/experimental studies and animal studies) were not considered eligible.
Data selection
Concrete reviews of abstracts were performed by two authors independently to select potentially eligible studies. A full-text review of potentially relevant studies was performed with independent assessment of eligibility. Disagreement between the reviewers concerning the inclusion of particular studies was resolved through discussion with the third author.
Data collection process
Studies on the aesthetic outcome of the abdominal donor site after DIEP flap harvest were included in chronological order for detailed analysis and data extraction. With regard to studies on the aesthetic outcome of the donor site key studies were defined of which a narrative synthesis is included in the results section (Table 2). Studies reporting the functional morbidity of the abdominal wall and complications are summarized in Tables 3,4. The parameters for data extraction were the following: number of patients, follow-up time, abdominal bulging, abdominal hernia, wound dehiscence, seroma, hematoma, infection, fat necrosis and umbilical necrosis. Two reviewers independently assessed the parameters and disagreements were resolved as previously discussed.
Full table
Full table
Full table
Outcomes of interest
The primary interest of this study was to evaluate the aesthetic outcome of the donor site after DIEP flap elevation. The secondary outcomes were functional impairment of the abdominal wall and general complications after DIEP flap harvest.
Results
Search result
The systematic search yielded 1,472 discrete articles. After deduplication and following review of title and abstract, 95 articles were included in full-text review. The detailed selection process is shown in Figure 2.
Donor site aesthetic
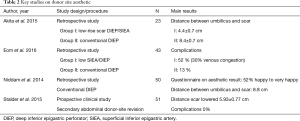
Only a very small number of studies specifically focusing on the aesthetic aspect of the abdominal donor site after DIEP flap harvest were found in the review process. Based on this, four key studies were identified (Table 2). One review article of a single surgeon on donor site aesthetic was screened, but not included as a key study based on the exclusion criteria (13).
In 2014, Niddam et al. investigated patient satisfaction with the abdominal result after breast reconstruction with a single DIEP flap (7). Fifty patients were included in the study and seen in consultation by a senior surgeon (not the operator) for a semi-directive interview and standardized questionnaire. The most prominent area of concern for the patients were lateral dog-ears, which were present in 50% of the cases. In 40% of the cases, the abdominal scar could not be hidden by undergarments. Patients frequently complained about the loss of sensibility of the abdominal wall in 44% of the cases. Nevertheless, 70% of the patients reported to be either happy or very happy with the appearance of the scar. The final scar was measured to be about 10.6 cm above the commissure. The revision rate to improve the aesthetic results of the abdominal donor site, such as scar or dog-ear revision, was 46% in. The author states that his technique includes a double-strand suture of the rectus fascia without opposite plicature which might result in a lateral displacement of the umbilicus that needs to be revised during a second operation. Given the high patients’ concern regarding dog-ears, they further recommend to approximate the skin edges from lateral to medial.
In 2015, Akita et al. proposed a new design with a low-rise scar for DIEP flap harvest in effort to improve donor site aesthetic (11). In this technique, the skin island is caudally located with a narrow vertical width regardless of the location of dominant perforators. A larger amount of adipose tissue is elevated to obtain enough volume for breast reconstruction and the skin is cranially undermined in order to harvest the dominant perforator, which was not in the area of the skin paddle in 9/12 cases in the study. They found that the distance between the umbilicus and donor site scar was significantly reduced in the low-rise DIEP group compared to standard DIEP (4.4 versus 8.4 cm) and the scar length significantly shorter. They reported that no vascular thrombosis or partial skin or fat necrosis occurred. However, with this technique an additional vertical scar in the midline resulted at the site where the umbilicus was excised.
In a similar approach, Eom et al. proposed a low DIEP flap in 2016 (10), which differs from the low-rise DIEP flap with respect to perforator selection. In this technique, a perforator always at the level of the low skin island was selected, and no flap undermining to include a potential dominant perforator further cranial was performed. The perforator was either a dominant perforator that was located lower than usual or a second dominant perforator that seemed to be able to nourish the whole flap. When compared to conventional DIEP flaps, all early complications occurred in the low DIEP flap group. Venous congestion requiring surgical intervention occurred in 30.4% of the cases and flap loss rate was 4.3%. Direct closure without umbilical repositioning was possible in most cases. The scar was 1–2 cm above the pubic rim and concealed by underwear in all cases. The pedicle was approximately 4 cm shorter than in a conventional flap. Based on this, the authors proposed to use the low DIEP flap when there is a dominant perforator more than 4 cm below the umbilicus or when there is second dominant perforator more than 4 cm below the umbilicus that is still large enough to nourish the whole flap. In addition, they proposed that if the low DIEP flap is based on a small perforator in the lower abdomen, venous supercharging with a superficial vein should be performed.
In 2015, a different approach by Stalder et al. recommended a two-step approach to achieve satisfying donor site results after DIEP flap harvest (8). They performed abdominal revision surgery on all patients during the second stage of breast reconstruction three months after the initial operation. During the procedure liposuction was performed to reduce the thickness of the cranial flap and fat depots on mons pubis or flanks. The scar was lowered to a point 4 to 7 cm from the commissure of the labia majora, depending on the stature of the patient. The umbilical stalk was transected during cranial flap mobilization, and the umbilicus raised as part of the superior abdominal flap. Any residual fascial defect was closed and the umbilicus relocated inferiorly and anchored to the fascia. If rectus diastasis is present, the fascia was plicated at this time to further improve the abdominal contour. The authors claim that the described technique for lowering the donor-site scar consumes 27 minutes on and provides reproducible, aesthetically pleasing results without wound healing problems.
In summary, a surprisingly low number of studies have been published up to date that are primarily concerned with the aesthetic improvement of the abdominal donor site after DIEP flap harvest.
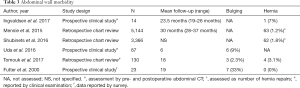
Functional morbidity of the abdominal wall
As a secondary interest outcome, we evaluated studies reporting functional donor site morbidity (Table 3). Functional donor site morbidities may include reduced abdominal strength, abdominal pain, and abdominal bulging or hernia. Based on the included studies, the overall rate of abdominal hernia ranges from 0 to 7% for DIEP flap procedures (2,14-17). Regarding abdominal bulging, the overall incidence seems to be even higher, ranging from 2.3% to 33% (2,16,18). However, the validity of these reported rates is limited by the different study designs (retrospective chart review vs. prospective study based on questionnaires) as well as the fact that several studies do not differentiate between abdominal bulging and hernias (2). Regarding abdominal strength, Uda et al. could observe a complete recovery of abdominal muscle function at 6 months postoperatively.
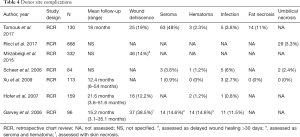
General complications
Abdominal wound complications can be a significant cause of postoperative morbidity after DIEP flap harvest. Studies showing the results of general donor site complication are summarized (Table 4). These include wound dehiscence, that occurs in 12% to 39% (16,19-21), as well as seroma (1–48%) (16,21-23) and hematoma (1–15%) (16,20-22). Furthermore infections (1–12%) (15,16,21-23), fat necrosis (0–11%) (16,23) and umbilical necrosis (0–3%) (22-24) might significantly impair the donor site appearance.
Discussion
Since it was first introduced nearly 20 years ago, the DIEP flap has become a popular technique for autologous breast reconstruction (3,25). While it became clear that the aesthetic results regarding the restoration of the breast with soft natural tissue are usually excellent and aesthetically pleasing (26), the appearance of the abdominal donor site remains a factor of dissatisfaction for patients and plastic surgeons alike (8). Microsurgical reconstruction of the breast has become a very safe and reliable method in the hands of the experienced surgeon and much attention has been given to successful results. In marked contrast to this stands the still largely neglected appearance of the donor site, which is usually expected to be tolerated by the patients.
Patients often choose breast reconstruction with an abdominal flap as they desire an improvement of the abdominal contour and the additional benefit of an abdominoplasty “for free” (7). However, this is often not the case. On the other hand, cosmetic abdominoplasty has also been associated with a high incidence of patient dissatisfaction and litigation for surgeons (27) and has a revision rate between 14–43% in literature (28,29). Stewart et al. analyzed 278 consecutive abdominoplasties and found dog-ears in 12%, localized fat excess in 10%, and unsatisfactory scars in 8% (30). Salgarello et al. reported in a meta-analysis of complications after DIEP flap harvest vs. elective abdominoplasty, that seroma was present in significantly more patients after abdominoplasty (16.1%) when compared to DIEP flap harvest (3.7%) (31). Given this relatively high proportion of unfavorable results after cosmetic abdominoplasty, the undesirable appearance of the donor site after DIEP flap harvest which involves an additional incision of the rectus fascia is not surprising. It is also not clear, which role functional abdominal morbidity plays in donor site aesthetic and wound healing. Certainly, the presence of additional bulging or even hernia will not improve aesthetic results after DIEP flap harvest.
The DIEP flap has increasingly replaced the free TRAM flap for breast reconstruction because it has been shown to shorten inpatient hospital stays, cause less postoperative pain and fewer donor site morbidities (15,32) especially regarding abdominal wall integrity. Although the DIEP flap contains less rectus muscle than a TRAM flap, harvest of the perforating vessel and the inferior epigastric artery may however still cause dysfunction of the abdominal wall and damage to the intercostal nerves through crossing of the vessels during harvest (33,34). The resulting contour of the abdominal wall is not only determined by abdominal bulging and hernia, but can also be significantly impaired by a visible step-off above the scar caused by difference in flap thickness, lateral dog-ears, lateral fat accumulations, sagging or bulky appearance of the mons pubis as well as displacement of the umbilicus. In order to improve donor site aesthetic, Tillet and Wilson observed a reduction of 26.2% in abdominal wound healing complications after the introduced a new regime of abdominal closure involving three layers of Monocryl to close the skin and subcutaneous tissues, with either the senior author supervising a senior trainee or performing the procedure himself (35). This dramatic reduction in complications indicates that donor site closure should not be taken lightly.
Local wound complications are an additional crucial factor that will determine the aesthetic outcome. Although local complication rates of the donor site show a wide range which is mainly due to the heterogeneity of included studies, a wound dehiscence at the donor site tends to be the most frequent local complication and especially accounts for an impaired aesthetic outcome. In this context, Mirzabeigi et al. observed an association of delayed wound healing with obesity, smoking, bilateral reconstruction and preoperative chemotherapy (19).
We have experienced, that besides the appearance of the scar, i.e., color, hypertrophy/atrophy, retraction, and widening, the localization of the scar and thus the possibility to hide the scar by undergarments is crucial regarding the final aesthetic outcome. In this context, the authors have observed that the scar is often intentionally placed low on the abdomen and still appears to move cranially in the healing process. One reason for this may be the actual tension on the skin, under which the donor site is closed. Since skin is stretchable and will adapt, the relatively soft skin on the mons pubis may yield to the cranial pulling forces and the scar will migrate cranially. Thus, cautious patient selection and donor site closure with as little tension as possible is important. In the authors experience, typically, patients with a normal to slightly elevated BMI and local fat deposition in the lower abdomen and some skin laxity may be the best candidates. In addition, previous pregnancies seem to have a positive influence on perforator perfusion and thickness.
Given the small number of studies dealing with the aesthetic aspect of the donor site, only a few recommendations for improvements of the donor site exist. These include plicature of the opposite rectus fascia and fixation of the umbilicus to the fascia to prevent any lateral displacement, either during the initial operation (7) or secondary as proposed by Stalder et al. (8). Based on the authors experiences, a very low scar about 5–7 cm above the commissure of the labia majora (Figure 3) and meticulous donor site closure in three layers, as proposed by Tillet and Wilson, has proven its worth in terms of wound healing and scar localization. Special attention should also be given to exactly mark the midline from the xiphoid to the labial commissure and secure the markings at the beginning of the operation with staplers.
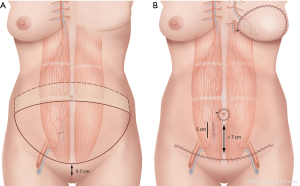
Regarding abdominal wall morbidity, the incision of the fascia to harvest the perforator vessel should be as short as possible (Figure 4) and motor branches of the intercostal nerves should be preserved. The design of a low-rise scar DIEP is reasonable in terms of scar localization but marred by its increased incidence of local complications and venous congestion (10,11). Nevertheless, the performance of secondary corrections as proposed by Stalder et al. during the second step of breast reconstruction remains a valuable option to further improve the aesthetic result (8).
In conclusion, the presented study reveals that the topic of donor site aesthetic and potential improvement of results has largely been neglected in the past decade. This study provides a thorough evaluation of potential problems the plastic surgeon may encounter and recommendations to improve results.
Acknowledgments
We would like to thank Sabine Klein and Martina Gosteli, University Library of Zurich for performing the systematic literature search, Carol De Simio-Hilton for the drawings of Figure 3, and to Michelle Mc Luckie for review and grammatical corrections of the manuscript. This work received none financial support.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Guerra AB, Metzinger SE. Use of the deep inferior epigastric perforator flap in a 15-month-old boy after resection of lymphatic malformation. J Pediatr Surg 2004;39:1428-31. [Crossref] [PubMed]
- Futter CM, Webster MH, Hagen S, et al. A retrospective comparison of abdominal muscle strength following breast reconstruction with a free TRAM or DIEP flap. Br J Plast Surg 2000;53:578-83. [Crossref] [PubMed]
- Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg 1994;32:32-8. [Crossref] [PubMed]
- Blondeel Ph N, Vanderstraeten GG, Monstrey SJ, et al. The donor site morbidity of free DIEP flaps and free TRAM flaps for breast reconstruction. Br J Plast Surg 1997;50:322-30. [Crossref] [PubMed]
- Bonde CT, Lund H, Fridberg M, et al. Abdominal strength after breast reconstruction using a free abdominal flap. J Plast Reconstr Aesthet Surg 2007;60:519-23. [Crossref] [PubMed]
- Egeberg A, Rasmussen MK, Ahm Sorensen J. Comparing the donor-site morbidity using DIEP, SIEA or MS-TRAM flaps for breast reconstructive surgery: A meta-analysis. J Plast Reconstr Aesthet Surg 2012;65:1474-80. [Crossref] [PubMed]
- Niddam J, Bosc R, Lange F, et al. DIEP flap for breast reconstruction: Retrospective evaluation of patient satisfaction on abdominal results. J Plast Reconstr Aesthet Surg 2014;67:789-96. [Crossref] [PubMed]
- Stalder MW, Accardo K, Allen RJ, et al. Aesthetic Refinement of the Abdominal Donor Site after Autologous Breast Reconstruction. Plast Reconstr Surg 2015;136:455-61. [Crossref] [PubMed]
- Gill PS, Hunt JP, Guerra AB, et al. A 10-year retrospective review of 758 DIEP flaps for breast reconstruction. Plast Reconstr Surg 2004;113:1153-60. [Crossref] [PubMed]
- Eom JS, Kim DY, Kim EK, et al. The Low DIEP Flap: An Enhancement to the Abdominal Donor Site. Plast Reconstr Surg 2016;137:7e-13e. [Crossref] [PubMed]
- Akita S, Mitsukawa N, Tokumoto H, et al. Low-rise scar deep inferior epigastric artery perforator flap for breast reconstruction. Microsurgery 2015;35:451-6. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006-12. [Crossref] [PubMed]
- Nahabedian MY. Achieving ideal donor site aesthetics with autologous breast reconstruction. Gland Surg 2015;4:145-53. [PubMed]
- Shubinets V, Fox JP, Sarik JR, et al. Surgically Treated Hernia following Abdominally Based Autologous Breast Reconstruction: Prevalence, Outcomes, and Expenditures. Plast Reconstr Surg 2016;137:749-57. [Crossref] [PubMed]
- Mennie JC, Mohanna PN, O'Donoghue JM, et al. Donor-Site Hernia Repair in Abdominal Flap Breast Reconstruction: A Population-Based Cohort Study of 7929 Patients. Plast Reconstr Surg 2015;136:1-9. [Crossref] [PubMed]
- Tomouk T, Mohan AT, Azizi A, et al. Donor site morbidity in DIEP free flap breast reconstructions: A comparison of unilateral, bilateral, and bipedicled surgical procedure types. J Plast Reconstr Aesthet Surg 2017;70:1505-13. [Crossref] [PubMed]
- Ingvaldsen CA, Bosse G, Mynarek GK, et al. Donor-Site Morbidity After DIEAP Flap Breast Reconstruction-A 2-Year Postoperative Computed Tomography Comparison. Plast Reconstr Surg Glob Open 2017;5:e1405. [Crossref] [PubMed]
- Uda H, Kamochi H, Sarukawa S, et al. Clinical and Quantitative Isokinetic Comparison of Abdominal Morbidity and Dynamics following DIEP versus Muscle-Sparing Free TRAM Flap Breast Reconstruction. Plast Reconstr Surg 2017;140:1101-9. [Crossref] [PubMed]
- Mirzabeigi MN, Wilson AJ, Fischer JP, et al. Predicting and managing donor-site wound complications in abdominally based free flap breast reconstruction: improved outcomes with early reoperative closure. Plast Reconstr Surg 2015;135:14-23. [Crossref] [PubMed]
- Hofer SO, Damen TH, Mureau MA, et al. A critical review of perioperative complications in 175 free deep inferior epigastric perforator flap breast reconstructions. Ann Plast Surg 2007;59:137-42. [Crossref] [PubMed]
- Garvey PB, Buchel EW, Pockaj BA, et al. DIEP and pedicled TRAM flaps: a comparison of outcomes. Plast Reconstr Surg 2006;117:1711-9; discussion 1720-1.
- Scheer AS, Novak CB, Neligan PC, et al. Complications associated with breast reconstruction using a perforator flap compared with a free TRAM flap. Ann Plast Surg 2006;56:355-8. [Crossref] [PubMed]
- Xu H, Dong J, Wang T. Bipedicle deep inferior epigastric perforator flap for unilateral breast reconstruction: seven years' experience. Plast Reconstr Surg 2009;124:1797-807. [Crossref] [PubMed]
- Ricci JA, Kamali P, Becherer BE, et al. Umbilical necrosis rates after abdominal-based microsurgical breast reconstruction. J Surg Res 2017;215:257-63. [Crossref] [PubMed]
- Koshima I, Soeda S. Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg 1989;42:645-8. [Crossref] [PubMed]
- Christensen BO, Overgaard J, Kettner LO, et al. Long-term evaluation of postmastectomy breast reconstruction. Acta Oncol 2011;50:1053-61. [Crossref] [PubMed]
- Bragg TW, Jose RM, Srivastava S. Patient satisfaction following abdominoplasty: an NHS experience. J Plast Reconstr Aesthet Surg 2007;60:75-8. [Crossref] [PubMed]
- Floros C, Davis PK. Complications and long-term results following abdominoplasty: a retrospective study. Br J Plast Surg 1991;44:190-4. [Crossref] [PubMed]
- Stevens WG, Spring MA, Stoker DA, et al. Ten years of outpatient abdominoplasties: safe and effective. Aesthet Surg J 2007;27:269-75. [Crossref] [PubMed]
- Stewart KJ, Stewart DA, Coghlan B, et al. Complications of 278 consecutive abdominoplasties. J Plast Reconstr Aesthet Surg 2006;59:1152-5. [Crossref] [PubMed]
- Salgarello M, Tambasco D, Farallo E. DIEP flap donor site versus elective abdominoplasty short-term complication rates: a meta-analysis. Aesthetic Plast Surg 2012;36:363-9. [Crossref] [PubMed]
- Rozen WM, Ashton MW. Improving outcomes in autologous breast reconstruction. Aesthetic Plast Surg 2009;33:327-35. [Crossref] [PubMed]
- Bajaj AK, Chevray PM, Chang DW. Comparison of donor-site complications and functional outcomes in free muscle-sparing TRAM flap and free DIEP flap breast reconstruction. Plast Reconstr Surg 2006;117:737-46; discussion 747-50. [Crossref] [PubMed]
- Chen CM, Halvorson EG, Disa JJ, et al. Immediate postoperative complications in DIEP versus free/muscle-sparing TRAM flaps. Plast Reconstr Surg 2007;120:1477-82. [Crossref] [PubMed]
- Tillett R, Wilson S. Reducing abdominal complications from breast reconstruction using DIEP flaps. Eur J Surg Oncol 2012;38:438. [Crossref]